2.9 Tissue types
Physiclogy
The body’s control systems require cell or tissue of organs to “communicate” with others via chemical means.
Most communication involve a specific chemical and a specific receiver for its signal - the receptor. the strength of the signal is often dependent on the concentration of the chemical.
Receptors
Most are protein macromolecules
Most of them are in the cell membrane, but there are some that are in the nucleus
tend to be in families
Naturally occurring chemical bind at multiple different receptor types
Example: Serotonin has 20 different receptors which controls appetite, mood, sleep, sex, nausea, homeostasis and bowel motility
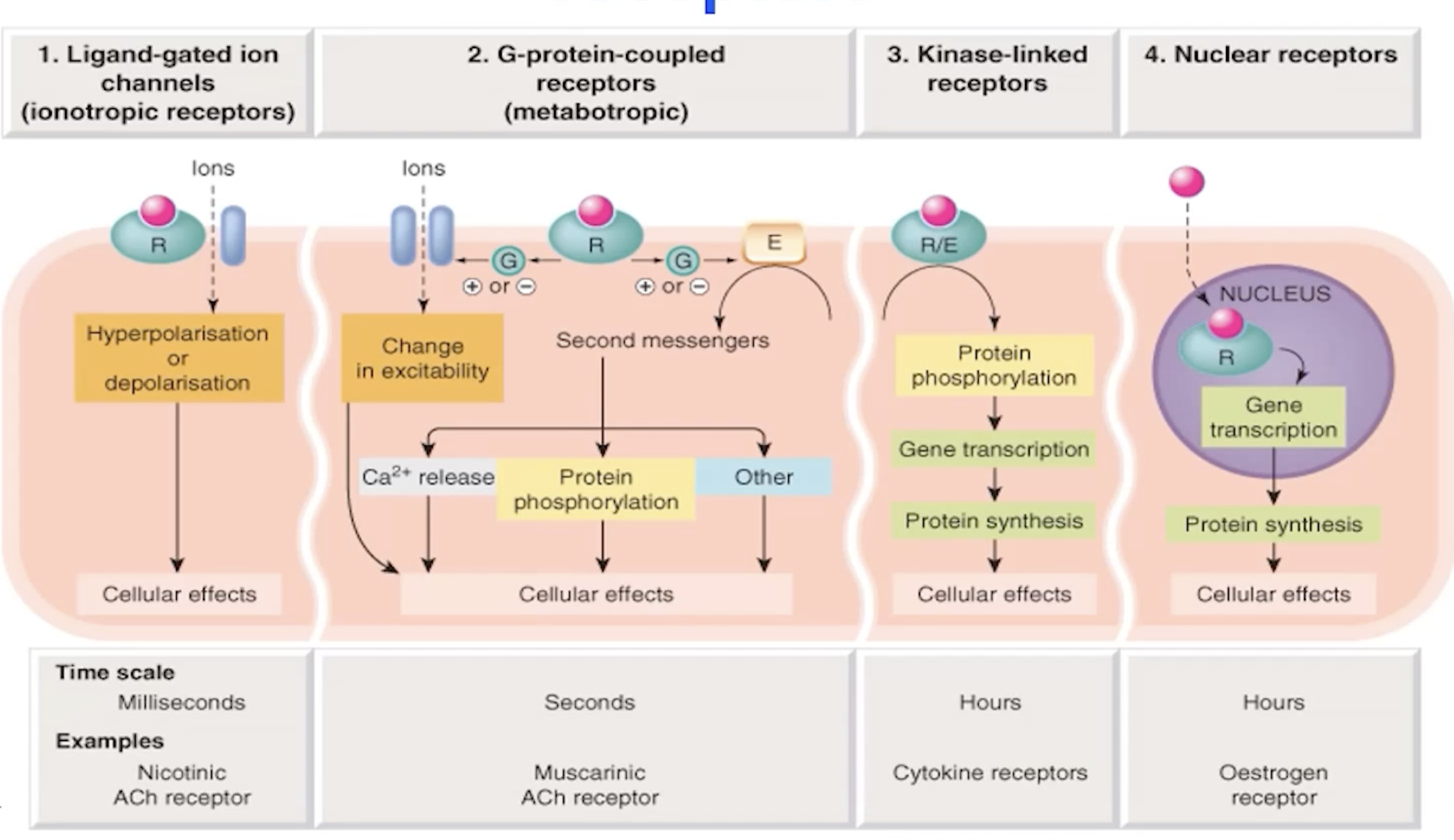
Four types of small molecule receptors
Ligand-gated channels (Ionotropic receptors)
G-protein-coupled receptors (metabotropic)
Kinase-linked receptors
Nuclear receptors
Actions of monoclonal antibodies
Direct Delivery: Monoclonal antibodies can deliver drugs, toxins, or radioactive substances directly to specific cells.
Receptor Blockage: They can block the interaction between receptors and their ligands, inhibiting the signaling pathways.
Ligand Blockage: Similar to receptor blockage, they can prevent ligands from binding to their respective receptors.
Receptor Downregulation: Monoclonal antibodies can induce the internalization and degradation of receptors, decreasing their availability on the cell surface.
Signal Induction: They can activate receptors to induce a cellular response.
Depletion: Monoclonal antibodies can lead to the depletion of target cells through various mechanisms.
A cell has many receptors
Contration
Receptors involved in contraction are typically found in muscle tissues and can include specific types of receptors that respond to neurotransmitters and hormones, facilitating muscle contraction.
Types of receptors that may be involved in contraction include:
Adrenergic Receptors: Respond to adrenaline and are important in the contraction of smooth muscle.
Muscarinic Receptors: Respond to acetylcholine and are involved in the contraction of cardiac and smooth muscle.
Activation of these receptors leads to cellular signaling pathways that promote muscle contraction through mechanisms such as increasing intracellular calcium levels.
Relaxation
Receptors that facilitate muscle relaxation typically counter the actions of contraction receptors, helping to decrease muscle tone and promote relaxation.
Types of receptors involved in relaxation may include:
Beta-Adrenergic Receptors: These receptors, when activated by catecholamines like epinephrine, cause relaxation of smooth muscle, particularly in the airways and blood vessels.
Muscarinic Receptors (M2 subtype): Activation can lead to relaxation in certain smooth muscles by inhibiting adenylate cyclase, which decreases cyclic AMP and calcium levels, promoting relaxation.
The relaxation process often involves the decrease of intracellular calcium levels and the activation of signaling pathways that promote smooth muscle relaxation.
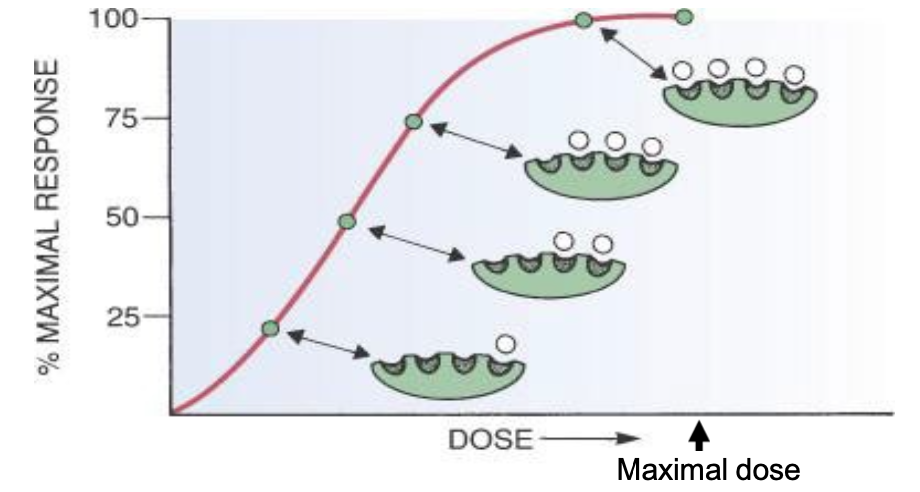
Receptor occupancy theory
Higher the dose, more drug available to bind to the different receptors that are involved, more effect.
In general, with 50% of maximal dose, resulting in about 80% of the benefit
Generally drugs work by mimicking nature
Using nature might have unwanted side effects. Can’t get into the body except by injection, and oftentimes the duration of the action is too short
Drugs can be more or less specific than the rael thing by binding to only a single subtype can be more specific.
Drugs which rely on receptors to work
Examples:
Adrenaline or epinephrine
binds to α1 (vascular smooth muscles (constrict)), α2 (nerve terminals), β1 (heart) , β2 (bronchial smooth muscles (relax)) and β3 (fats)
Action: Seconds/minutes
Salbutamol or ventoline (used for asthma)
binds to β2 agonist
action: <4 hours
Salmeterol
binds to β2 agonist
action: >12 hours
Drugs which do not work via receptors
Some drugs exert their effects through mechanisms that do not involve interaction with receptors. These may include:
Enzyme Inhibitors: Drugs that inhibit specific enzymes to alter biochemical pathways (e.g., statins reducing cholesterol synthesis).
Antacids: Substances that neutralize stomach acid physically rather than through receptor-mediated action.
Diuretics: Some diuretics work by affecting ion transport mechanisms in the kidneys without direct receptor interactions.
Chemotherapeutic Agents: Certain cancer drugs may work by directly interacting with cellular DNA or other cellular components to inhibit cell division.
These drugs often act through broader biological effects rather than targeting specific receptor pathways.
Potency, efficacy, agonism
Definition of potency: Potency describes how strong a drug is and its ability to create an effect at a specific dose. A drug is more potent if it needs a smaller amount to have the same impact as another drug. Higher potency means you need less of the drug to get the desired effect.
Definition of efficacy: Efficacy refers to the maximum effect that a drug can produce regardless of the dose, indicating the drug's ability to achieve its intended therapeutic effect when administered at the optimal dose.
Definition of agonism: Agonism is when a drug attaches to a receptor and activates it, causing a response in the body.
Definition of agonist: An agonist is a substance that binds to a receptor and activates it, leading to a biological response.
Types of Agonists:
Full Agonists: These create the strongest possible response.
Partial Agonists: These produce a weaker response, even if they completely fill the receptor sites.
Antagonism (competitive)
Definition: Competitive antagonism occurs when a drug (the antagonist) binds to the same receptor as an agonist but does not activate it.
Mechanism: This binding prevents the agonist from attaching and activating the receptor, thus inhibiting the biological response that would normally occur.
Effect: The presence of the competitive antagonist can be overcome by increasing the concentration of the agonist, making it possible for the agonist to outcompete the antagonist for receptor binding sites.
Antagonism (non-competitive)
Definition: Non-competitive antagonism occurs when a drug (the antagonist) binds to a receptor at a different site than the agonist, preventing the agonist from producing its effect regardless of its concentration.
Mechanism: The binding of the antagonist changes the shape or function of the receptor in such a way that the agonist cannot activate it, leading to a reduced biological response.
Effect: Non-competitive antagonism cannot be overcome by simply increasing the concentration of the agonist, as the antagonist permanently affects the receptor's ability to respond to the agonist.
Toxicity
Definition: Toxicity refers to the degree to which a substance can cause harmful effects in living organisms. It is important in pharmacology as it helps determine the safety and permissible dosage of drugs.
Sources of Toxicity:
Drug Overdose: Taking higher than recommended doses of a medication can lead to toxic effects.
Individual Sensitivity: Some individuals may have unique reactions to certain drugs due to genetic, metabolic, or health factors, leading to toxicity even at normal doses.
Drug Interactions: Combining drugs can sometimes result in toxic effects that do not occur when drugs are taken individually.
Immunological response: generally called an allergy
Metabolite (breakdown products): A metabolite is a substance produced during the metabolism of a drug or compound in the body.
Measurement: Toxicity is often measured via the therapeutic index, which compares the dose that produces a therapeutic effect to the dose that produces a toxic effect. A lower therapeutic index indicates a narrower margin of safety for the drug.
Scenario of efficacy anfd adverse effects
Ideal scenario: The drug achieves maximum efficacy with minimal adverse effects, ensuring patient safety and optimal therapeutic outcomes.
Common scenario: The drug may provide effective treatment but is associated with significant adverse effects, leading to challenges in patient compliance and potential harm.
Worst-case scenario: The drug not only fails to provide the desired therapeutic effect but also results in severe adverse effects, posing significant risks to patient health and necessitating immediate intervention.