Notes on the Cardiovascular System: The Heart
The heart is a powerful muscular pump that plays a critical role in supplying oxygenated blood to the body's tissues while also facilitating the removal of waste products. Its pumping action creates pressure essential for the dispersal of blood into the major vessels: the aorta—responsible for carrying oxygen-rich blood to the body—and the pulmonary trunk, which directs deoxygenated blood to the lungs for oxygenation. The term "cardiology" originates from the Latin word "kardia," which means heart, highlighting the central focus of this field of study.
Chapter Objectives
Identify the anatomical parts of the heart, including both interior and exterior components.
Describe the intricate pathways that blood takes within the cardiac circuits, understanding their functional significance.
Discuss the heart's size, shape, and location within the thoracic cavity, emphasizing its relationship with surrounding organs.
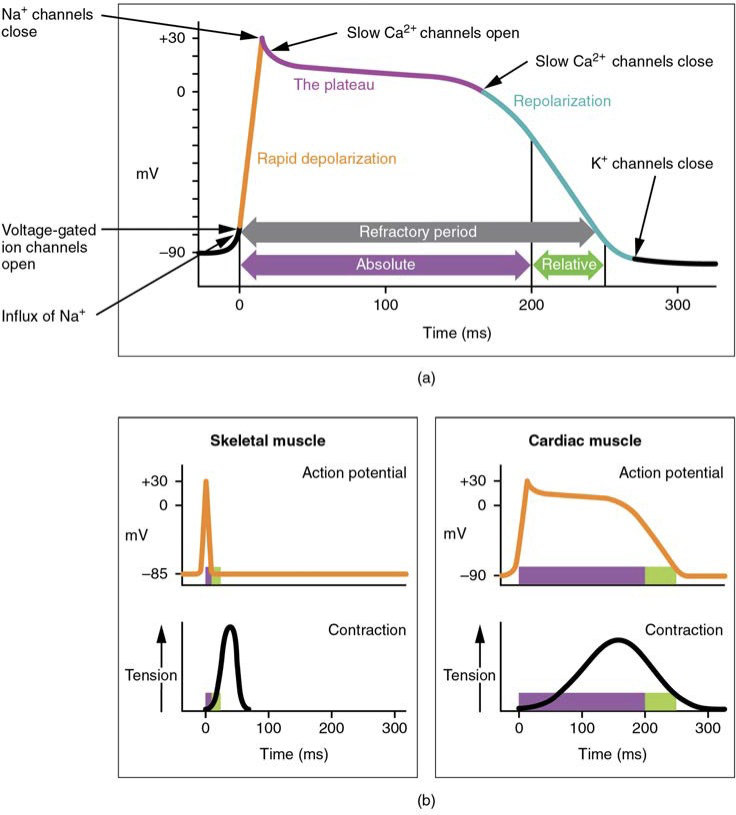
Compare and contrast cardiac muscle with skeletal and smooth muscles to highlight the unique characteristics of myocardial tissue.
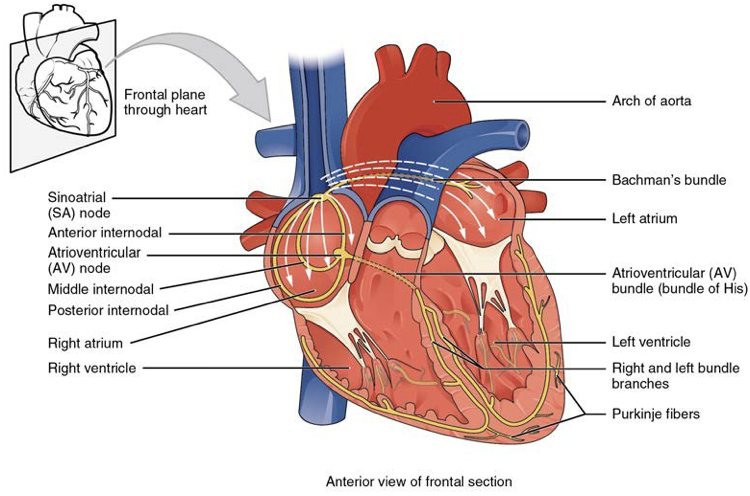
Explain the cardiac conduction system, its components, and essential functions in maintaining a consistent heartbeat.
Detail the process and interpretation of an electrocardiogram (ECG), which reflects the electrical activities of the heart.
Understand the phases of the cardiac cycle, including systole and diastole, which are crucial to heart function.
Heart Anatomy
Location
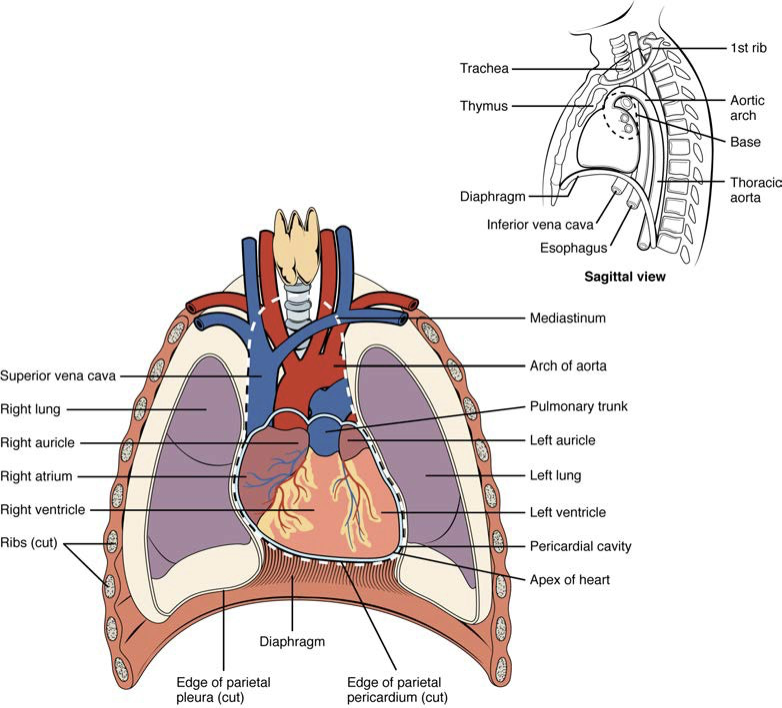
The heart resides within the thoracic cavity, positioned medially between the lungs within a space known as the mediastinum. This anatomical positioning is essential for the heart's interaction with surrounding structures.
A protective membrane called the pericardium encasing the heart creates the pericardial cavity, which contains serous fluid that reduces friction during heartbeats.
The base of the heart is aligned approximately with the third costal cartilage, while the apex rests between the fourth and fifth ribs, allowing for a mechanical advantage in blood pumping.
Size & Shape
The heart's dimensions are roughly the size of a fist, measuring approximately 12 cm in length, 8 cm in width, and 6 cm in thickness.
Its weight varies between the sexes: females typically weigh between 250–300 grams, whereas males range from 300–350 grams. These differences can significantly impact cardiovascular health and disease susceptibility.
Notably, among athletes, the heart may undergo physiological adaptations where their heart is larger due to exercise, leading to a condition known as hypertrophy, where the heart muscle becomes enlarged to accommodate increased blood flow demands during physical activity.
Chambers and Circulation
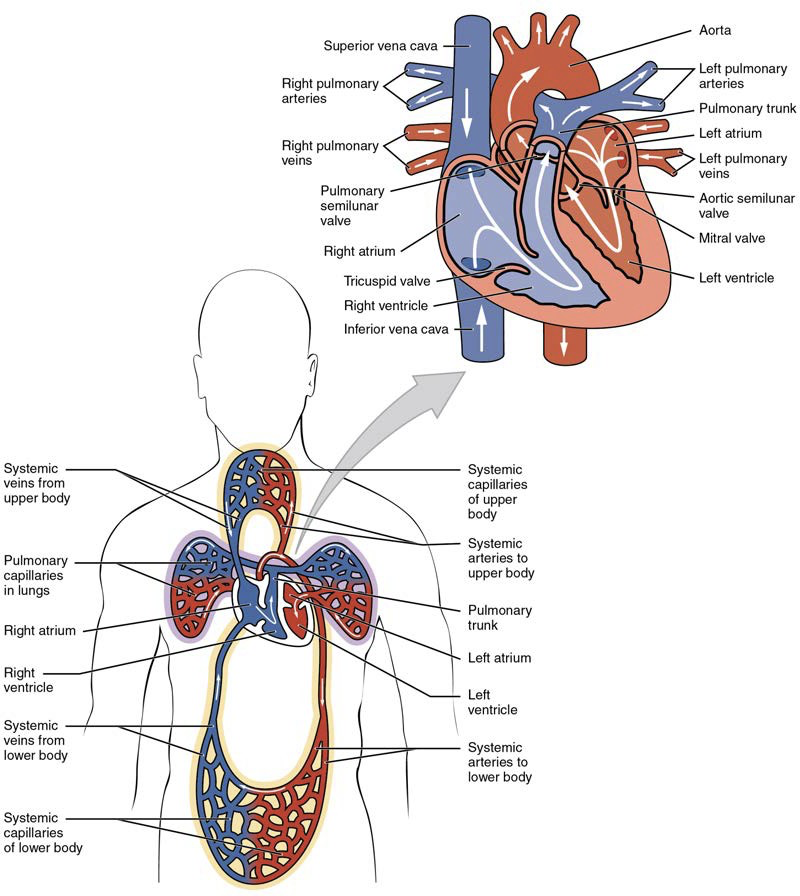
Comprising four main chambers, the heart includes two atria (right and left) and two ventricles (right and left).
the atriums receive blood and contract to push blood to the ventricles
the ventricles propel blood to the lungs and rest of the body
The right side of the heart is responsible for managing deoxygenated blood traveling towards the lungs for oxygenation, while the left side handles oxygen-rich blood, distributing it to the rest of the body.
The sequence of blood flow is crucial: it follows this path — right atrium → right ventricle → pulmonary trunk → lungs → pulmonary arteries → pulmonary capillaries → pulmonary veins → left atrium → left ventricle → aorta → systemic circuit → systemic capillaries → superior/inferior vena cava
Blood Circulation Pathways
Pulmonary vs. Systemic Circulation
The pulmonary circuit is vital as it transports deoxygenated blood from the heart to the lungs for gas exchange, where carbon dioxide is expelled, and oxygen is absorbed.
The systemic circuit distributes oxygenated blood from the heart to body tissues, supplying them with necessary oxygen and nutrients, while also collecting carbon dioxide and other metabolic wastes for return to the heart.
Membranes and Layers
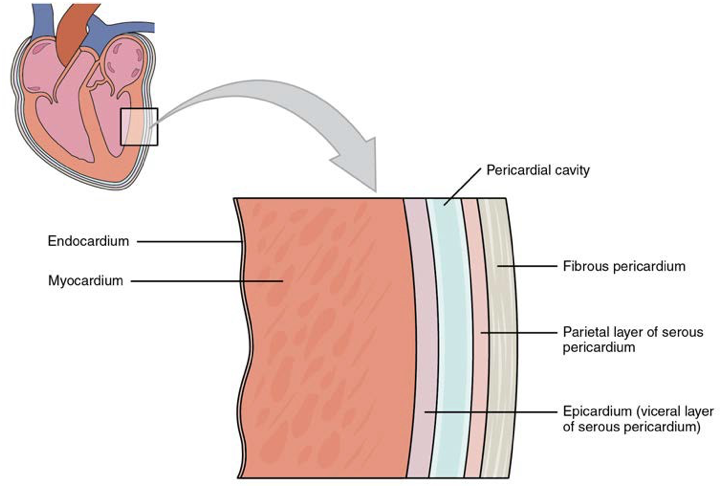
The structure of the heart consists of three main layers:
Epicardium: This protective outer layer is synonymous with the visceral pericardium, providing a barrier against potential injury.
Myocardium: The middle muscular layer is primarily responsible for heart contractions, and its thickness varies between chambers; the ventricles have a more robust myocardium to pump blood more forcefully than the atria.
Endocardium: The innermost layer, lining the heart chambers and valves, provides a smooth surface that minimizes turbulence as blood flows through the heart.
Pericardium Structure: The pericardium comprises two key parts:
the fibrous pericardium, which protects and anchors the heart
the serous pericardium, which includes the visceral and parietal layers, contributing to the heart’s lubrication during movement.
parietal pericardium (fused to fibrous pericardium)
epicardium (fused to heart)
Surface features of Heart
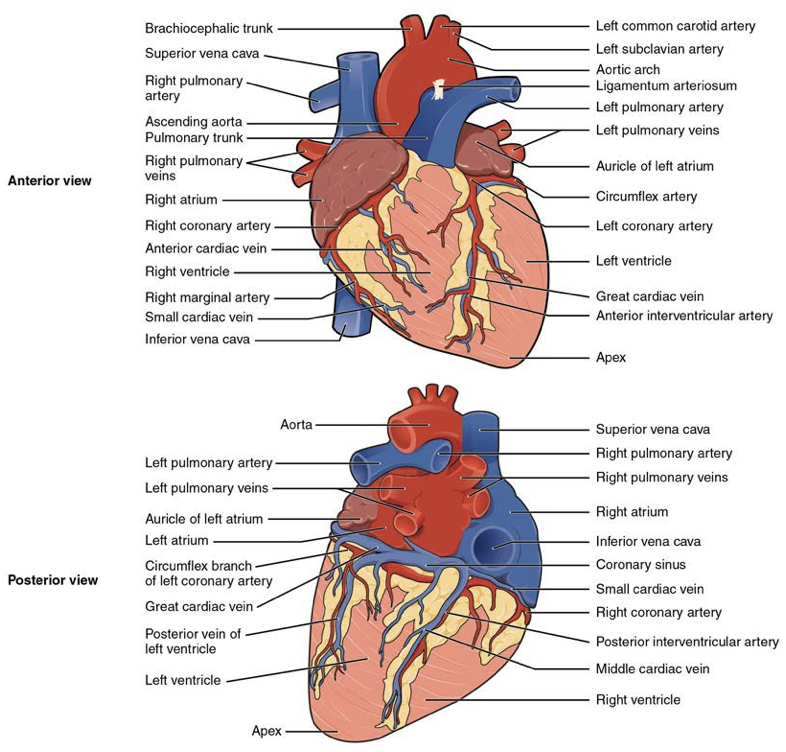
auricle: an ear-shaped projection on the upper chambers of the heart, assisting in the expansion of the atria to accommodate varying blood volumes.
sulcus: a groove on the surface of the heart that separates the various chambers and serves as a pathway for coronary arteries and veins.
coronary sulcus: the indentation that encircles the heart, marking the boundary between the atria and ventricles, crucial for the attachment of coronary arteries and aiding in the coronary circulation.
interventricular sulcus: the groove that separates the left and right ventricles, playing a significant role in the anatomy of the heart by providing a surface for blood vessels and nerves.
Internal Structure of the Heart
Septum: the muscular wall that divides the left and right sides of the heart, preventing the mixing of oxygenated and deoxygenated blood, thus ensuring efficient circulation.
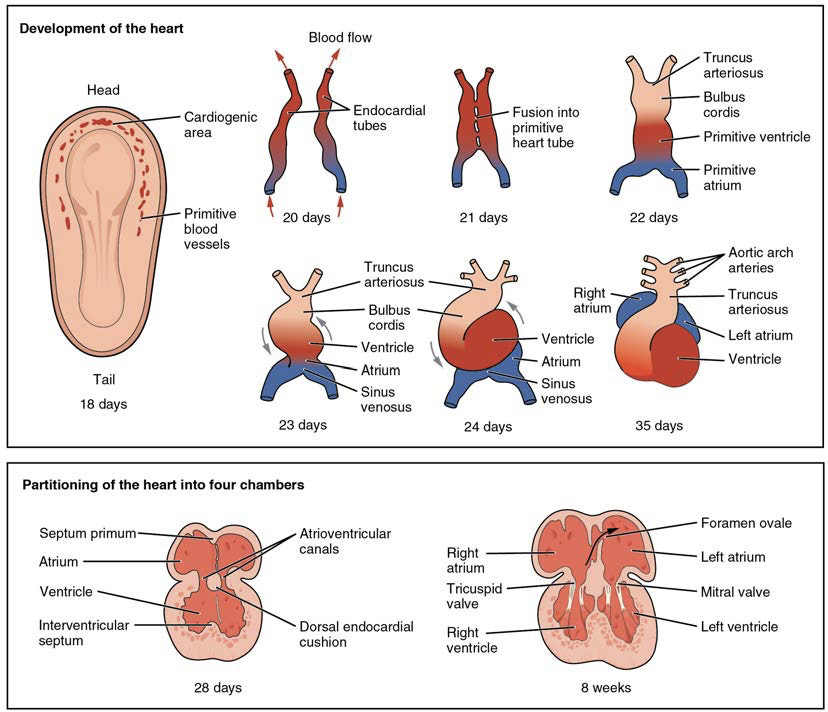
interatrial septum: the thin muscular partition between the left and right atria, also crucial for maintaining separate blood flows and aiding in the heartbeat rhythm.
fossa ovalis: a depression in the interatrial septum, serving as a remnant of the foramen ovale from fetal circulation, which allowed blood to bypass the non-functioning lungs.
foramen ovale: a temporary opening in the fetal heart that connects the right atrium to the left atrium, enabling bypass of pulmonary circulation; after birth, it typically closes to form the fossa ovalis.
septum primum: a thin membrane that acts as a precursor to the interatrial septum, developing in the embryonic heart to separate the atria during gestation.
interventricular septum: the muscular wall that separates the left and right ventricles of the heart, playing a crucial role in preventing the mixing of oxygenated and deoxygenated blood.
atrioventricular septum: the fibrous tissue structure that separates the atria from the ventricles, ensuring that electrical signals travel appropriately through the heart and preventing backflow of blood during contraction.
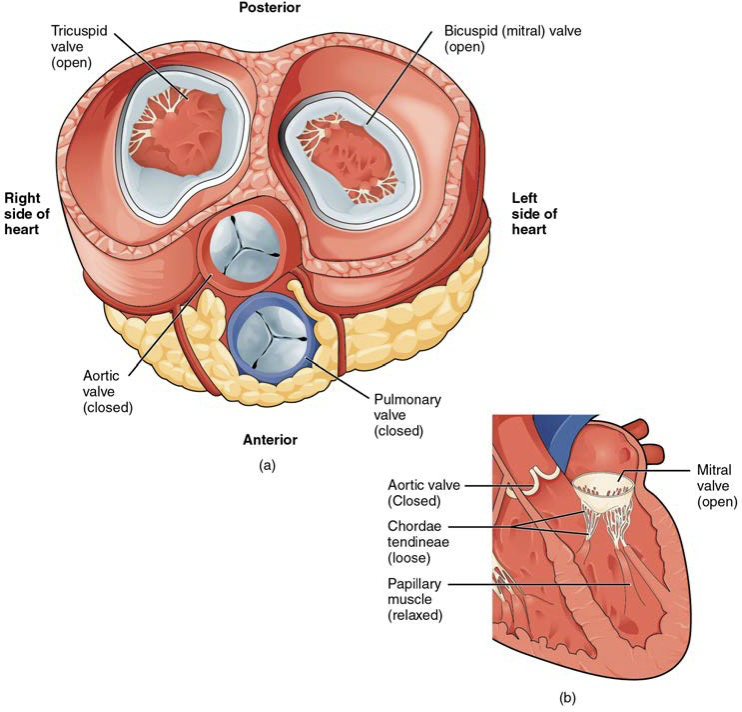
valve: structures that open and close to regulate blood flow through the heart chambers and prevent backflow, including the mitral and tricuspid valves.
atrioventricular valves: the valves located between the atria and ventricles, specifically the mitral valve on the left and the tricuspid valve on the right
semilunar valves: the valves located at the exit of the ventricles, responsible for preventing blood from flowing back into the heart after contraction, including the aortic valve and the pulmonary valve.
cardiac skeleton: a fibrous skeleton that provides structural support, anchors the heart valves, and serves as an electrical insulator between the atria and ventricles, ensuring coordinated contractions.
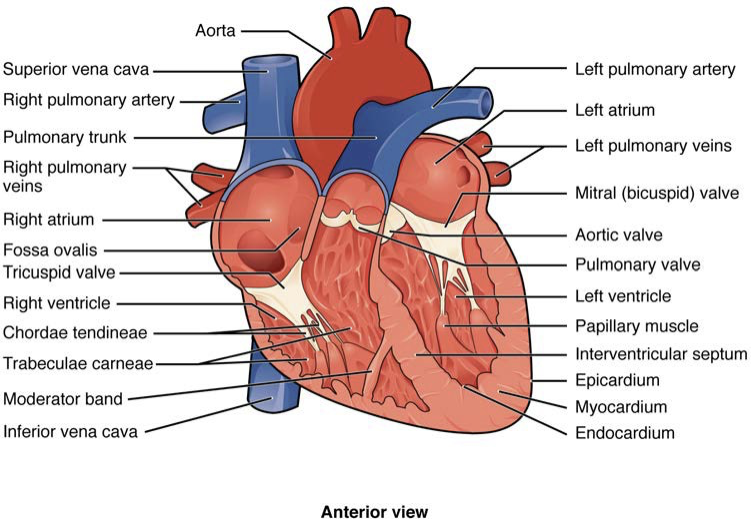
Atriums, Ventricles, & Valves
Right Atrium: the upper right chamber of the heart that receives deoxygenated blood from the body through the superior and inferior vena cavae and the coronary sinus; it then pumps this blood into the right ventricle.
superior vena cava empties blood from the head, neck, upper limbs, and thoracic region
inferior vena cava empties blood from lower limbs and abdominopelvic region
contains pectinate muscles that help increase the strength of contractions and facilitate the movement of blood into the right ventricle.
Right Ventricle: The chamber of the heart responsible for pumping deoxygenated blood to the lungs via the pulmonary arteries for oxygenation.
receives blood from right atrium through tricuspid valve
chordae tendineae: fibrous cords that connect the papillary muscles to the tricuspid valve, preventing it from inverting during ventricular contraction.
papillary muscle: muscle tissue located within the ventricles that attaches to the chordae tendineae and helps maintain the position of the tricuspid valve during contraction.
trabeculae carneae: irregular muscular ridges that project from the inner surface of the ventricles, providing structural support and aiding in the contraction of the heart.
moderator band: a muscular band in the right ventricle that extends from the interventricular septum to the anterior papillary muscle, playing a role in coordinating ventricular contraction.
Left Atrium: The chamber of the heart that receives oxygenated blood from the lungs via the pulmonary veins, and serves as a conduit for this blood to flow into the left ventricle.
Left Ventricle: The chamber of the heart that receives oxygenated blood from the left atrium and pumps it into the aorta, supplying oxygen-rich blood to the body.
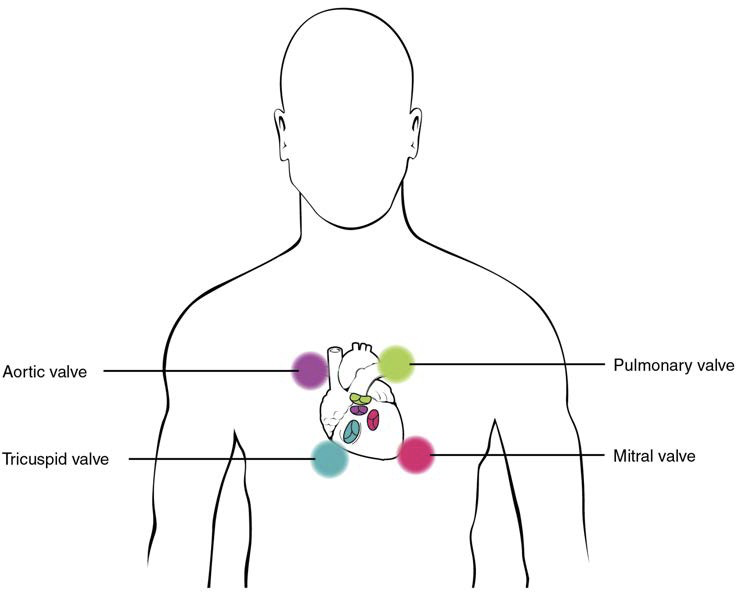
Valves
Tricuspid valve: The heart valve that consists of three flaps located between the right atrium and the right ventricle that prevents backflow of blood into the atrium during ventricular contraction.
Pulmonary valve: The valve comprised of three small flaps located between the right ventricle and the pulmonary artery that allows blood to flow from the heart into the lungs for oxygenation, preventing backflow into the ventricle.
Bicuspid valve: The heart valve consisting of two flaps located between the left atrium and the left ventricle that ensures proper blood flow into the ventricle during atrial contraction and prevents backflow into the atrium.
Aortic valve: The valve located between the left ventricle and the aorta that regulates blood flow from the heart into the aorta, preventing backflow into the ventricle during diastole.
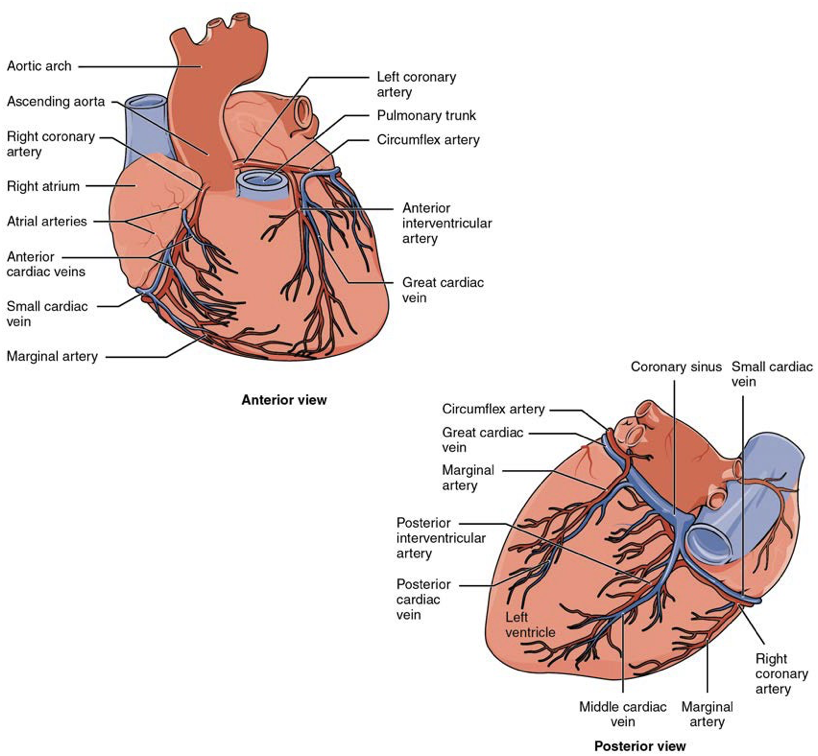
Coronary Ciruculation
Coronary circulation: The system of blood vessels that supply blood to the heart muscle itself, including the coronary arteries and veins, ensuring that the heart receives the necessary oxygen and nutrients to function effectively.
Coronary Arteries: The blood vessels that branch off from the aorta and deliver oxygen-rich blood to the heart muscle, playing a crucial role in sustaining its metabolic demands.
epicardial coronary arteries: The arteries that lie on the surface of the heart, providing oxygenated blood to the epicardium, or outer layer of the heart muscle.
circumflex arteries: The arteries that branch off from the left coronary artery and encircle the heart, supplying blood to the left atrium and the lateral and posterior parts of the left ventricle, thereby supporting overall cardiac function.
anterior interventricular artery: The artery that is a major branch of the left coronary artery, supplying blood to the anterior wall of the left ventricle and the interventricular septum, playing a significant role in the heart's pumping efficiency.
marginal arteries: The small arteries that run along the margin of the heart, providing blood supply to the myocardial tissue, ensuring that the heart muscle remains healthy and capable of effective contraction.
posterior interventricular artery: The artery that branches off from the right coronary artery, supplying blood to the posterior wall of the left and right ventricles, crucial for maintaining the heart's structural integrity and optimal function.
anastomosis: A connection or junction between two or more blood vessels, which allows for collateral circulation and can help maintain blood supply to the heart during blockages or compromised blood flow.
Cardiac Muscle and Electrical Activity
authorhythmicity: The unique property of cardiac muscle cells that allows them to generate electrical impulses independently, enabling the heart to maintain its rhythmic contractions and effectively pump blood throughout the body.
myocardial contractile cells: Specialized cardiac muscle cells responsible for the contraction of the heart, ensuring that blood is effectively ejected from the chambers during each heartbeat.
myocardial conducting cells: Specialized cardiac cells that are primarily involved in the conduction of electrical impulses, coordinating the timing of contractions to ensure the heart beats in a synchronized manner.
Cardiac Muscle Structure
striated appearance
intercalated discs: Unique structures that connect individual cardiac muscle cells, allowing for synchronized contraction by enabling rapid transmission of electrical signals between cells.
Heart Conduction System
The conduction system of the heart is composed of specialized cardiac conducting cells that regulate heart rhythm through electrical impulses.
Key components include:
SA Node: Also known as the pacemaker of the heart, it initiates (sinus rhythm) heartbeats by generating electrical signals that spread through the atria.
impulses spread through internodal pathways to atrioventricular node and myocardial contractile cells
Bachmann’s Bundle: A specialized bundle of cardiac fibers that facilitates electrical conduction from the left atrium to the right atrium, ensuring synchronized contraction of both atria.
AV Node: Acts as a relay station, temporarily delaying the electrical impulse to ensure adequate time for atrial contraction before ventricular contraction.
Bundles: These include the bundle of His and bundle branches, which transmit impulses down into the ventricles.
Purkinje Fibers: These fibers ensure rapid transmission of impulses across the ventricles, enabling synchronized contraction for efficient blood ejection.
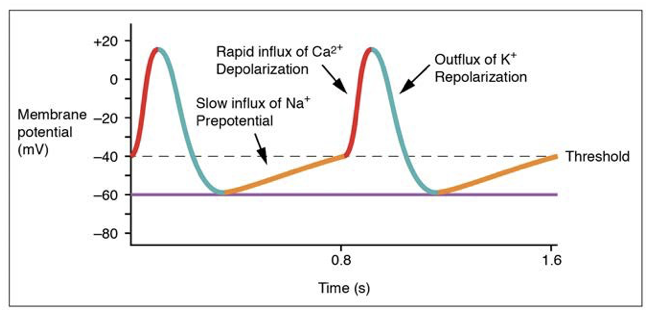
Membrane Potential and Ion Movement in Cardiac Conductive Cells
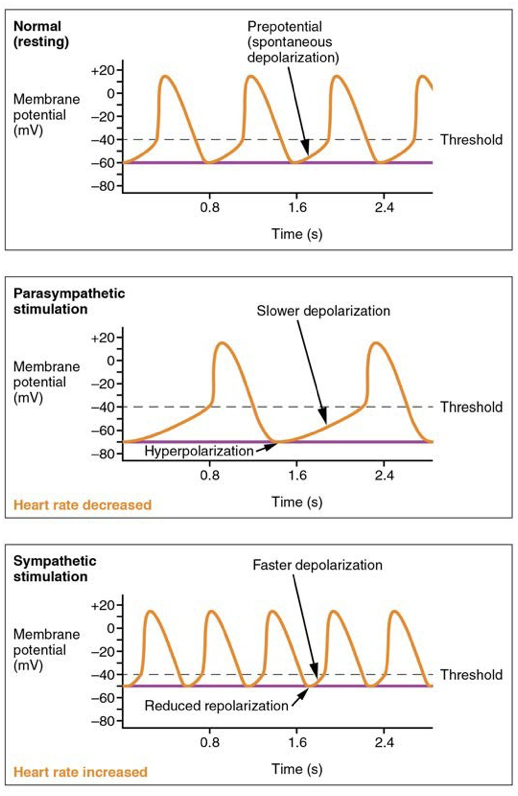
The membrane potential in cardiac conductive cells is primarily influenced by the movement of ions such as sodium (Na+), potassium (K+), and calcium (Ca2+), which create the electrical gradients necessary for initiating and propagating action potentials.
spontaneous depolarization process occurs in pacemaker cells, where the gradual influx of sodium ions leads to a threshold that triggers an action potential, setting the rhythm of the heartbeat.
Membrane Potential and Ion Movement in Cardiac Contractile Cells
In these cells, the action potential is characterized by a rapid depolarization due to the influx of sodium ions, followed by a plateau phase maintained by calcium ion influx, which is crucial for muscle contraction. This process of depolarization is then followed by repolarization, primarily due to the outflow of potassium ions, restoring the resting membrane potential and preparing the cells for the next contraction cycle.
Cardiac Muscle Metabolism
Cardiac muscle relies primarily on aerobic metabolism to generate ATP, utilizing fatty acids and glucose as fuel sources to sustain its high energy demands. This metabolic strategy ensures that the heart can maintain a consistent supply of energy, even during prolonged periods of activity.
Cardiac Cycle
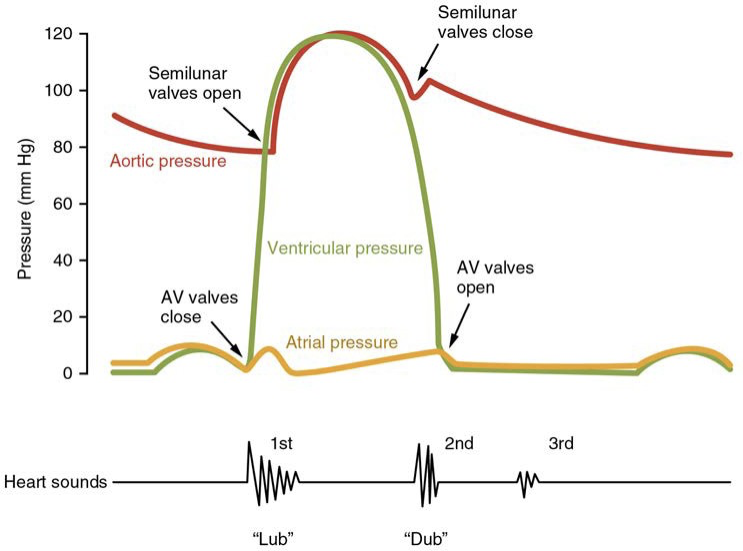
cardiac cycle: The sequence of events during which the heart undergoes contraction and relaxation, consisting of systole (contraction phase) and diastole (relaxation phase), ultimately responsible for pumping blood throughout the body.
Phases of Cardiac Cycle
Atrial Diastole: During relaxation, the atria fill with blood returning from the body and lungs, readying for the next contraction.
Atrial Systole: Atria contract, pushing blood into the ventricles, completing their filling.
Ventricular Systole: Ventricles contract, ejecting blood into the pulmonary trunk and aorta; this phase is critical for circulation to the lungs and body.
initial phase is isovolumic contraction, where the ventricles begin to contract, but the volume of blood within them remains unchanged as the atrioventricular valves close, preventing backflow into the atria.
second phase is ventircular ejection phase , where the pressure in the ventricles exceeds that in the arteries, forcing the semilunar valves open and allowing blood to flow out of the heart.
Ventricular Diastole: Ventricles relax and begin filling with blood again.
early phase is the isovolumic ventricular relaxation phase where the ventricles continue to relax, causing a decrease in pressure, and the semilunar valves close to prevent backflow from the arteries
after that ventricular diastole occurs
Heart Sounds: The cardiac cycle produces characteristic sounds: S1 (lub) occurs due to the closure of atrioventricular valves while S2 (dub) results from the closure of semilunar valves, crucial for determining heart health.
S3 (ventricular gallop) is an additional heart sound that may be heard in certain conditions, often associated with heart failure or volume overload, indicating rapid ventricular filling.
S4 (atrial gallop) is another heart sound, typically heard in conditions where the heart is working harder to fill the ventricles, such as in cases of hypertension or aortic stenosis, and indicates a stiff or hypertrophied ventricle.
S7 is the combined sound of S3 and S4
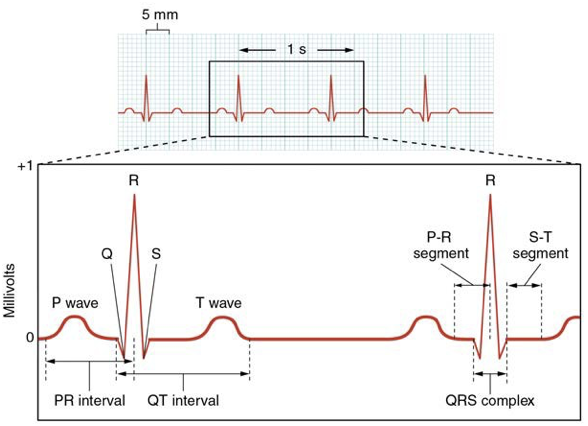
Electrocardiogram (ECG)
An ECG records the heart's electrical activity over time, providing vital information about the heart's rhythm and health. Major components include:
P Wave: Reflects atrial depolarization, signaling the onset of atrial contraction.
QRS Complex: Represents ventricular depolarization, indicating that the ventricles are preparing to contract.
T Wave: Indicates ventricular repolarization during relaxation.
The segments of the ECG relate directly to the mechanical events of the heart cycle, making it a crucial diagnostic tool for detecting arrhythmias and other heart conditions.
Cardiac Physiology
Cardiac Output (CO)
Cardiac Output is a vital measure of heart function, calculated using the formula: CO = Heart Rate (HR) × Stroke Volume (SV).
heart rate: beats per minute
stroke volume: amount of blood pumped in each ventricle
ejection fraction (EF): the percentage of blood that is pumped out of the ventricles with each heartbeat, indicating the efficiency of heart contractions.
A normal CO is approximately 5.25 L/min in a resting adult, although this can increase significantly during physical activity to meet the metabolic demands of the body, especially in athletes.
a normal HR is typically 75 but can be between 60 to 100 beats per minute, depending on various factors such as age, fitness level, hormones, and overall health.
a normal SV is typically around 70 mL per beat, which can also vary based on the individual's size, health status, and level of exercise.
cardiac reserve: measures the residual capacity of the heart to pump blood
Heart Rate
Maximum HR range from 200-220 bpm
Nervous control over HR is centralized within the two paired cardiovascular center of the medulla oblongata
cardioaccelerator regions stimulate the heart to increase its rate through the release of norepinephrine
cardioinhibitory regions help to lower the heart rate via the parasympathetic influence of acetylcholine.
autonomic tone refers to the balance between the sympathetic and parasympathetic nervous systems, which modulates heart rate and vascular tone, ensuring appropriate responses to various physiological demands.
cardiac plexus: a complex network of nerves that innervates the heart and regulates its function by coordinating the activity of the sympathetic and parasympathetic nervous systems.
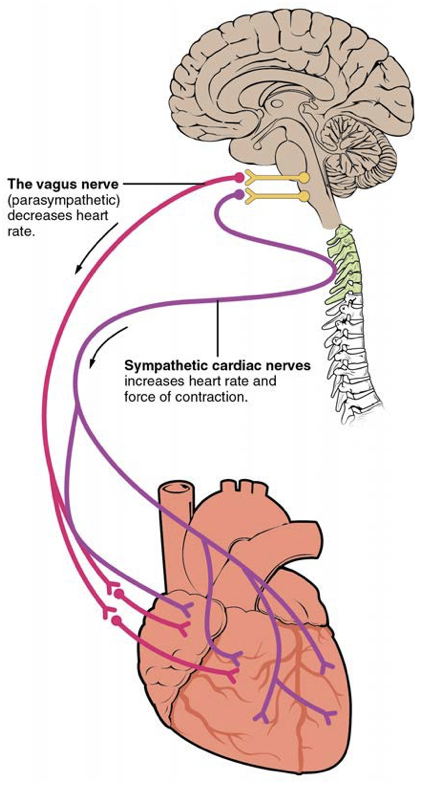
Cardiac reflexes: automatic responses triggered by changes in blood pressure or blood chemistry, which help maintain homeostasis by adjusting heart rate and blood vessel diameter.
baroreceptor reflex: a mechanism that helps regulate blood pressure by detecting changes in arterial pressure via baroreceptors located in the aorta and carotid arteries, leading to adjustments in heart rate and vascular resistance.
atrial reflex: a response initiated by stretch receptors in the atria that triggers an increase in heart rate when atrial pressure rises, thus aiding in the regulation of blood volume and pressure.
Factors Affecting Heart Rate and Contractility
Heart rate and contractility are influenced by various factors, including the autonomic nervous system and hormonal changes within the body.
Positive inotropic factors (like norepinephrine and epinephrine) enhance the strength of contractions, while negative inotropic factors (such as parasympathetic stimulation) can decrease contractility, impacting overall cardiac performance.
Abnormal Heart Conditions
Several conditions can lead to abnormal heart rates, such as bradycardia (slow heart rate) and tachycardia (fast heart rate), which may result from physiological adaptations or pathological conditions.
tachycardia can be caused by hyponatremia (low sodium levels) and hypernatremia (high sodium levels)
bradycardia can be caused by hyponatremia
Pathological conditions can include heart defects, arrhythmias (irregular heartbeats), and myocardial infarction (heart attack), all requiring careful monitoring and management.
arrhythmias can be caused by hyponatremia and hypokalemia (low potassium levels)
Hyperkalemia (high potassium levels) causes the heart to fail by becoming weak and flaccid
Acidosis is a condition that can also lead to arrhythmias, as it affects the heart's electrical system by altering the potassium and calcium balance needed for proper cardiac function.
is a condition characterized by an increase in blood pH, which can also disrupt normal heart rhythms by affecting ion transport and leading to imbalances in electrolytes.
Stroke Volume
Preload (EDV): This is the volume of blood in the ventricles at the end of diastole, which influences the amount of stretch in the cardiac muscle and ultimately affects the stroke volume.
filling time: The duration of diastole during which the ventricles fill with blood significantly impacts preload and consequently affects stroke volume.
Frank-Starling mechanism: This physiological principle describes how an increase in preload (the amount of blood filling the ventricles) leads to an increase in stroke volume, as the heart muscle fibers stretch and contract more forcefully.
Contractility: This refers to the intrinsic ability of cardiac muscle fibers to contract, independent of preload and afterload, and is influenced by factors such as calcium availability and sympathetic stimulation, ultimately contributing to the efficiency and effectiveness of the heart's pumping action.
Positive inotropic factors: These are substances or conditions that increase contractility, enhancing the heart's ability to pump blood more effectively. Examples include catecholamines, increasing calcium ion concentrations, and certain medications designed to strengthen cardiac output.
Negative inotropic factors: These are agents that decrease contractility, leading to reduced cardiac output. Common examples include beta-blockers, certain calcium channel blockers, and high levels of hydrogen ions or acidosis, which can impair the heart's ability to effectively contract.
Afterload: This term refers to the resistance the heart must overcome to eject blood during systole, primarily influenced by arterial blood pressure and vascular resistance, and plays a crucial role in determining the workload placed on the heart.
Heart Development
The heart's development begins at approximately 18-19 days gestation, establishing itself as the first functional organ in the human body and begins pumping blood at day 21/22.
It forms from mesodermal tissue and differentiates into distinct regions and structures during embryonic development, critical for ensuring proper circulation at birth.
Heart Bulge: The initial structure that forms the heart, which subsequently develops into the four chambers that are essential for efficient blood circulation.
Cardiogenic Area: The region of mesodermal tissue that gives rise to the heart and major vessels, indicating the early stages of cardiac development.
Cardiogenic Cords: The structures that develop from the cardiogenic area, which further differentiate to form the primary heart tube, playing a crucial role in the formation of the heart's anatomy.
Endocardial Tubes: The paired structures that develop from the cardiogenic cords, which eventually fuse to form the heart tube and contribute to the formation of the heart's inner lining.
Primitive Heart Tube: The initial structure formed during early heart development, which serves as the precursor to the fully developed heart, showcasing the basic organization and arrangement of cardiac chambers.
truncus arteriosus: The early embryonic structure that will eventually split into the pulmonary trunk and aorta, playing a critical role in establishing the separation of systemic and pulmonary circulation.
bulbus cordis: The region of the primitive heart tube that developed into the right ventricle
primitive ventircle: The portion of the early heart that contributes to the formation of the left ventricle
primitive atrium: The chamber of the early heart that gives rise to both the left and right atria
sinus venosus: deveoples into the posterior right atrium, SA node, and coronary sinus
Summary of Key Concepts
Autorhythmicity: The heart possesses the intrinsic ability to generate its rhythm, a fundamental feature facilitated by the pacemaker cells in the SA node.
The critical importance of blood circulation lies in its role in supplying oxygen and nutrients required by tissues, while concurrently facilitating waste removal.
The interrelationship between the heart's structure and function underscores its efficiency in performing its essential pumping action.
A comprehensive understanding of heart anatomy and physiology is vital for medical professionals to effectively diagnose and manage cardiovascular diseases, establishing a foundation for advancements in cardiology and patient care.