Detailed Notes on the Lymphatic and Immune System
Introduction to Lymphatic and Immune Systems
Overview: The lymphatic and immune systems work together to protect the body from pathogens.
Key Concepts:
Lymphatic system consists of vessels, cells, and organs to drain lymph and filter pathogens.
Immune system is composed of cells and soluble factors that destroy or neutralize pathogens.
AIDS and Immune Dysfunction
Historical Context:
In 1981, unusual cases of pneumonia (Pneumocystis jirovecii) and Kaposi’s sarcoma were reported among young adults, indicating immune suppression.
These cases marked the emergence of AIDS caused by HIV.
HIV Overview:
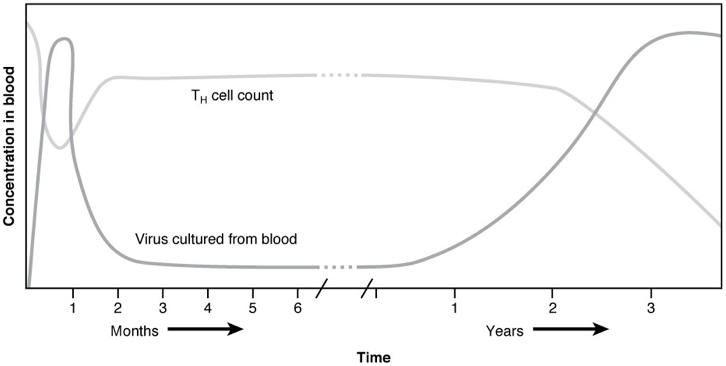
HIV attacks CD4+ T cells, leading to severe immunodeficiency.
Early treatment options were limited, but advancements turned HIV into a manageable condition.
Anatomy of the Lymphatic System
lymph: interstitial fluid that has entered the lymphatic system
Key Components of the Lymphatic System:
Lymphatic Capillaries:
tiny, thin-walled vessels that collect lymph from the interstitial spaces and transport it to larger lymphatic vessels
formed by a layer of endothelial cells
Lymphatic Vessels:
Begin as capillaries, merge into larger vessels, eventually forming ducts.
Flow towards the heart, aided by muscle contractions and one-way valves.
Lymphatic Trunks:
These are large vessels that drain lymph from specific regions of the body, such as the lumbar, bronchomediastinal, subclavian, and jugular trunks.
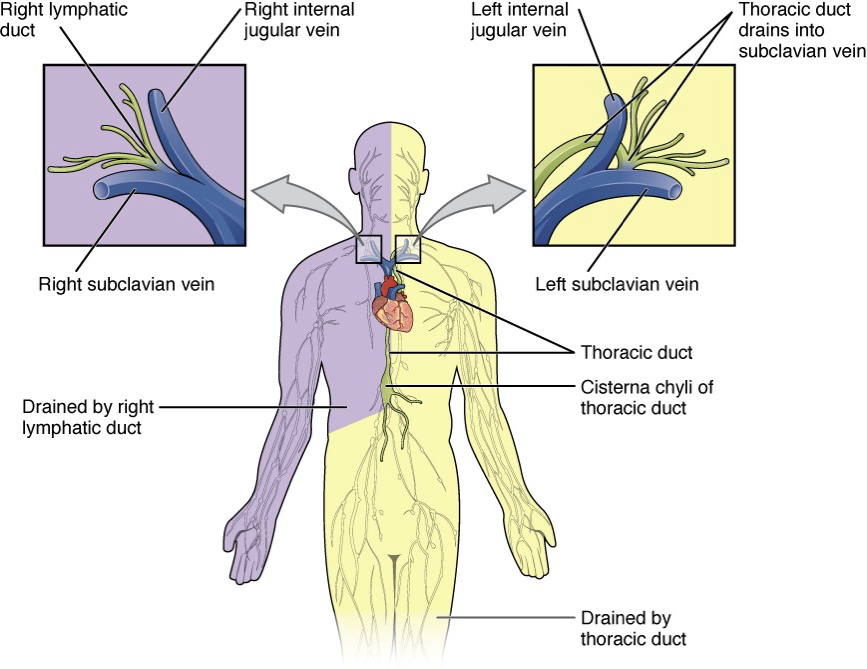
right side of head, thorax, and upper limb are drained by the right lymphatic duct, which empties lymph into the right subclavian vein.
The left side of the body, including the left side of the head, thorax, and the entire lower body, is drained by the thoracic duct, which ultimately empties into the left subclavian vein.
Lymph Nodes:
Primary vs. Secondary Organs:
Primary: Bone marrow and thymus - sites for lymphocyte maturation.
B cell goes through its development in the red bone marrow
T cells start in the bone marrow and developed in the thymus
thymus is found in the space between the sternum and aorta of the heart
Secondary: Lymph nodes, spleen - sites for immune response activation.
Lymph nodes:
Distributed throughout the body; act as filters of debris and pathogens for lymph fluid.
Site of immune cell activation and proliferation.
Spleen:
Largest lymphatic organ; helps filter blood and recycles iron from red blood cells.
Plays a crucial role in immune response by producing lymphocytes and storing platelets.
Lymphoid Nodules:
Small, localized clusters of lymphoid tissue found in various mucosal sites throughout the body; they play a key role in triggering immune responses by trapping pathogens and facilitating the activation of B and T cells.
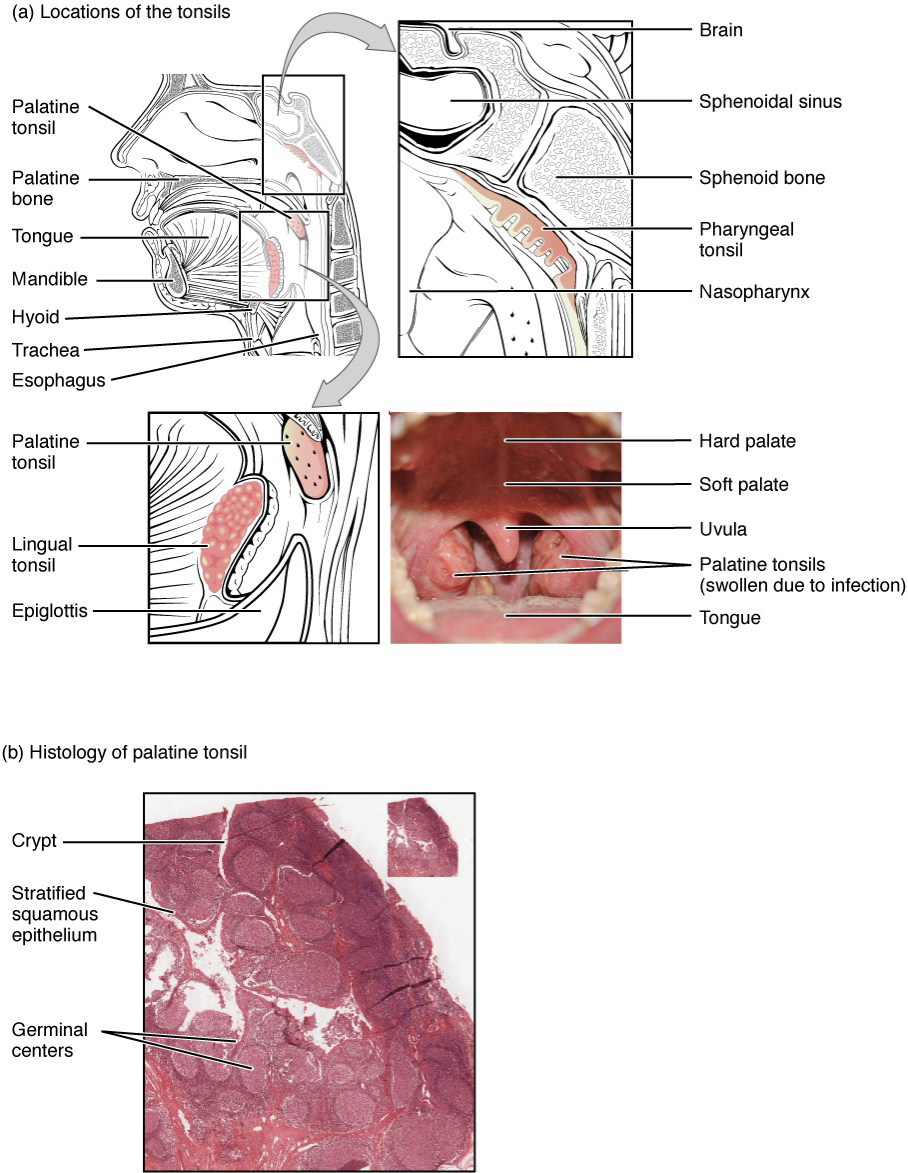
Tonsils: masses of lymphoid tissue located in the throat that help filter out pathogens entering through the mouth and nose, serving as the first line of defense in the immune system.
Mucosa-associated lymphoid tissue: A type of lymphoid tissue found in mucosal surfaces, such as the gut and respiratory tract, it plays a crucial role in protecting against pathogens by producing immune responses and maintaining homeostasis within these regions.
Functions of the Lymphatic System
Fluid Balance: Drains excess interstitial fluid back into circulation; approximately 20 liters filtered daily.
Transport of Fats: Transports dietary lipids from intestines, forming chyle.
Immune Function: Lymph nodes are critical for filtering pathogens and activating immune responses.
Immune Response Phases
Barrier Defenses:
skin and mucous membranes act as the first line of defense by preventing pathogens from entering the body
Epidermal surface of skin: protects with its keratinized cells
Sweat and sebaceous glands: protect with low pH and washing acton
Salivary glands in oral cavity: protect with lysozyme
Gastrointestinal tracts of stomach: protects with low pH
Mucosal epithelium of mucosal surfaces: protects with nonkeratinized epithelial cells
Mucosal tissues: protect by preventing pathogens from growing on mucosal surfaces
Innate Immune Response:
Immediate, nonspecific defense mechanisms; includes physical barriers like skin and inflammation.
Components include:
Phagocytic cells (e.g., macrophages, neutrophils).
macrophages do phagocytosis in body cavities/organs
neutrophils do phagocytosis in blood
monocytes precursor macrophages/dendritic cells in blood
Cytokines and chemokines for signaling and recruiting immune cells.
cytokines: signaling molecule that allows cells to communicate over short distances
chemokine: soluble chemical mediator which functions to attract cells from longer distances
NK cells respond to chemical signals and express the fas ligand; NK cells release perforins and granzymes
fas ligand: molecule that helps kill infected cell
perforin: protein that forma pores in the membrane of infected cells
granzyme: protein-digesting enzyme that enters through perforin pores and triggers apoptosis
pattern recognition receptor: molecules that detect pathogens and activate immune responses by recognizing specific pathogen-associated molecular patterns (PAMPs).
early induced proteins
interferons: proteins produced by host cells in response to viral infections, which help to inhibit viral replication and modulate the immune response.
opsonization: the process by which pathogens are marked for destruction by antibodies or complement proteins, enhancing phagocytosis and facilitating the clearance of infections.
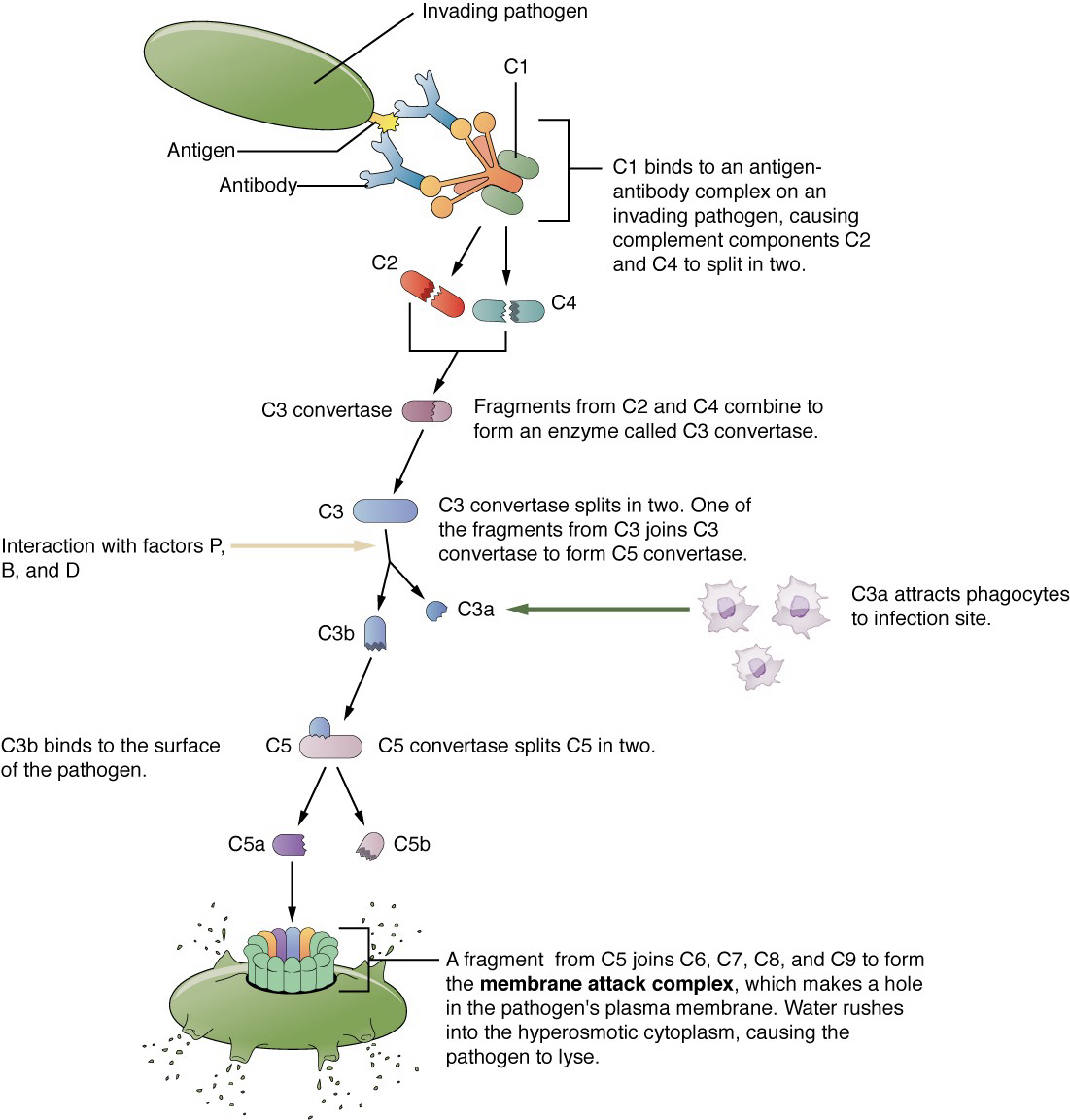
complement system: a complex network of proteins that enhances the ability of antibodies and phagocytic cells to clear pathogens from an organism, promoting inflammation and directly attacking pathogen membranes.
Bind to the cell membrane of the pathogen that activates it, labeling it for phagocytosis (opsonization)
Diffuse away from the pathogen and act as chemotactic agents to attract phagocytic cells to the site of inflammation
Form damaging pores in the plasma membrane of the pathogen
Inflammatory Response
Acute inflammation: short-term inflammation
Chronic inflammation: ongoing inflammation
Steps:
Tissue Injury; injured cells stimulate the release of mast cell granules and inflammatory mediators (histamine, leukotriene, prostaglandins).
Vasodilation; inflammatory mediators like histamine increase the diameters of local capillaries, allowing an increase in blood flow to the site of inflammation
Increased Vascular Permeability; inflammatory mediators increase permeability of local vasculature which causes leakage of fluid into interstitial space, resulting in swelling (edema)
Recruitment of Phagocytes; Leukotrienes attract neutrophils and other phagocytic cells to the site of injury, where they begin the process of engulfing and digesting pathogens and debris
Adaptive Immune Response:
Delayed but specific response led by lymphocytes (B cells and T cells).
Memory creation for faster response upon re-exposure to pathogens
Adaptive Immune Response: T Lymphocytes
Primary Disease and Immunological Memory
primary adaptive response: immune systems first exposure to a pathogen
primary disease: symptoms of first infection, relatively severe
secondary adaptive response: re-exposure to the same pathogen with a stronger and faster primary response
immunological memory: the ability of the immune system to remember previous encounters with pathogens, allowing for a quicker and more effective response upon subsequent exposures.
the adaptive immune response can distinguish between self antigens from foreign antigens
T Cell-Mediated Immune Responses
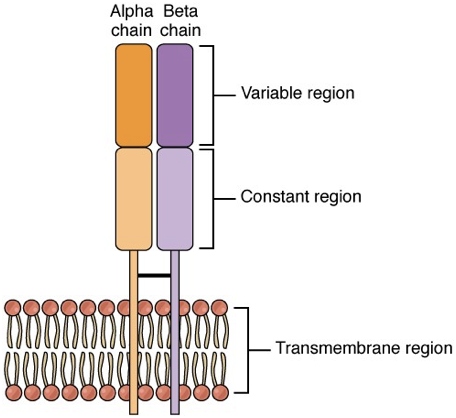
T lymphocytes recognize antigens by two chain protein receptors (alpha-beta T cell receptors)
the chains consist of the variable region domain and the constant region domain
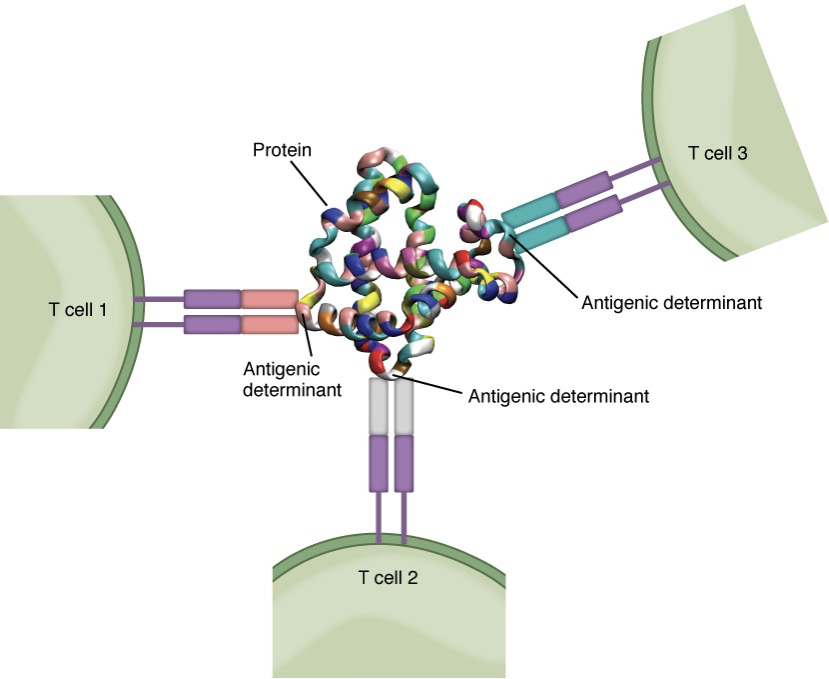
Antigens
antigenic determinant: a small region in an antigen where a receptor can bind
Antigen Processing: the method by which antigen-presenting cells (APCs) degrade antigens into peptide fragments, which are then presented on major histocompatibility complex (MHC) molecules for recognition by T cells.
major histocompatibility complex: a set of cell surface proteins essential for the acquired immune system to recognize foreign molecules. These proteins play a critical role in presenting antigenic peptides to T cells, enabling the immune response.
MHC class I: Stimulates cytotoxic T cell immune response
MHC class II
Macrophage: Stimulates phagocytosis and presentation at primary infection site
Dendritic: Brings antigens to regional lymph nodes
B cell: Stimulates antibody secretion by B cells
antigen presentation: association of antigen fragments with an MHC molecule, resulting in the recognition of an antigen by a T cell
T Cell Development
T cell tolerance: process of eliminating T cells that might attack cells of one’s own body
positive selection: the process by which developing T cells that recognize self-MHC molecules are allowed to survive, ensuring that they can effectively respond to antigens while avoiding autoimmunity.
negative selection: the process by which developing T cells that bind too strongly to self-antigens are induced to undergo apoptosis, thereby preventing potential autoimmunity and ensuring the self-tolerance of the immune system.
Clonal Selection and Expansion
clone: group of lymphocytes that share the same antigen receptor
polyclonal response: a response involving multiple clones of lymphocytes that recognize different epitopes on the same antigen, ensuring a robust and diverse defense against pathogens.
clonal expansion: the rapid proliferation of T cells in response to a specific antigen, allowing for an increased number of T cells that can effectively target and eliminate pathogens.
clonal selection: the process by which specific T cells are chosen for proliferation and differentiation in response to the recognition of a specific antigen, thereby ensuring a robust adaptive immune response aimed at eliminating the identified pathogen.
Cellular Basis of Immunological Memory
memory T cells: specialized T cells that persist long-term after an initial infection
effector T cells: short-lived T cells that are activated during an immune response and are responsible for carrying out the immediate effects of the immune response, including the destruction of infected or cancerous cells.
Adaptive Immune Response: B Lymphocytes
immunoglobulin: a type of antibody produced by B cells that plays a crucial role in identifying and neutralizing pathogens such as bacteria and viruses.
B Cell Differentiation and Activation
central tolerance: the process by which immature B cells are tested for self-reactivity in the bone marrow, allowing only those that do not react to the body’s own tissues to mature and enter circulation.
clonal deletion: a process by which autoreactive B cells are eliminated during development to prevent autoimmune diseases and ensure self-tolerance.
clonal anergy: a mechanism in which autoreactive B cells are rendered functionally inactive without being eliminated, allowing them to persist in a non-responsive state without triggering an immune response.
peripheral tolerance: the mechanisms that maintain self-tolerance in mature B cells operating outside the bone marrow, preventing them from responding to self-antigens in the periphery to mitigate the risk of autoimmunity.
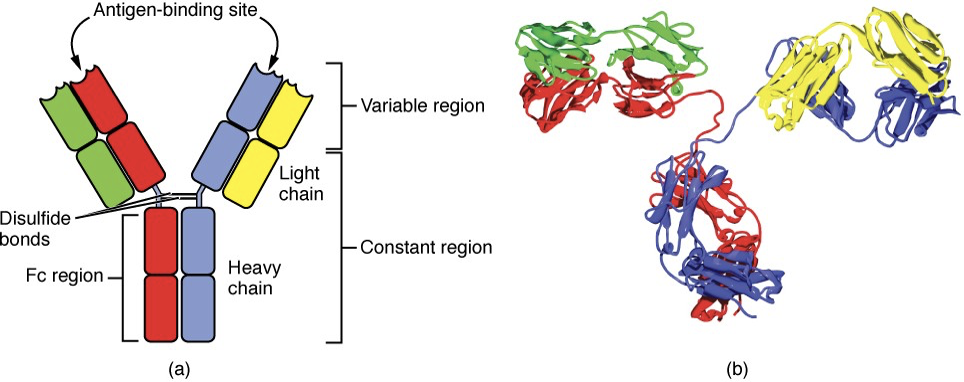
Antibody Structure
heavy chain: a large polypeptide chain that forms the primary structural foundation of an antibody, consisting of one variable region that binds to antigens and three constant regions that determine the antibody's class (IgG, IgM, IgA, IgE, IgD).
light chain: a smaller polypeptide chain that pairs with the heavy chain in an antibody structure, contributing one variable region for antigen binding and one constant region, with two types present (kappa and lambda) that help define the antibody's specificity and functionality.
antibody molecules have two heavy chains and two light chains
Fc region of antibody is formed by the two heavy chains together
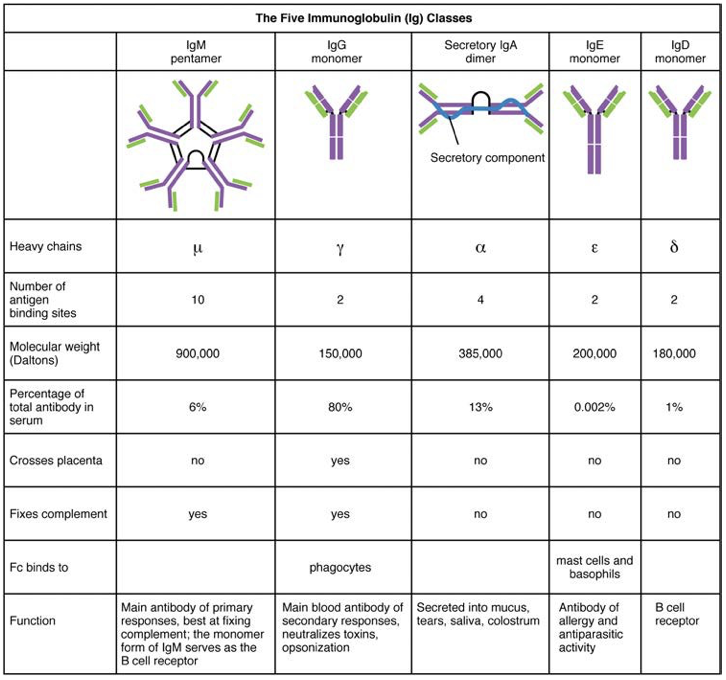
Classes of Antibodies
IgD: B cell receptor
IgM: main antibody in primary response; consists of five, four chain structures
IgG: main blood antibody of secondary responses
IgA: secreted into mucous, tears, saliva, colostrum
IgE: allergy and anti-parasitic antibody
Immunities
active immunity: the immunity that develops as a result of exposure to antigens, either through infection or vaccination, and involves the production of antibodies by the immune system.
passive immunity: the type of immunity that is acquired through the transfer of antibodies from another organism, providing immediate but temporary protection against infections.
T Cell-Dependent/Independent Antigens
T Cell-Dependent Antigens: These antigens require the assistance of T helper cells for the activation of B cells, leading to the production of antibodies. This process is crucial for generating a strong and long-lasting immune response.
T Cell-Independent Antigens: In contrast, these antigens can activate B cells without T cell help, typically triggering a quicker, but less robust antibody response. This type of response is often seen with certain polysaccharide antigens.
Lymphocyte Functionality
B Lymphocytes:
B Cells:
Originate in red bone marrow, capable of antibody production.
Upon activation, differentiate into plasma cells, producing antibodies that target specific antigens.
Memory B Cells:
Develop after initial infection, confer long-lasting immunity.
T Lymphocytes:
T Cells:
Mature in the thymus, critical for cell-mediated immunity.
Types include:
Helper T Cells (Th): Aid B cells and macrophages.
Th1 cells: secrete cytokines that regulate immunological activity and development of variety of cells, such as macrophages
Th2 cells: secrete cytokine that act on B cells
Cytotoxic T Cells (Tc): Directly kill infected cells by inducing apoptosis.
Regulatory T Cells (Treg): Modulate immune responses to prevent overactivity.
Activation: T cells require antigen presentation via MHC molecules.
Plasma Cells:
Produce antibodies that specifically target antigens, playing a crucial role in the humoral immune response
NK Cells:
Play a vital role in the innate immune response by identifying and destroying virus-infected cells and tumor cells without prior sensitization.
Immune Response Against Pathogens
seroconversion: reciprocal the relationship between virus levels in the blood and antibody levels
Mucosal Immune Response
IgA and IgM in mucus and bind to pathogens and neutralize them
neutralization: the process by which antibodies, specifically IgA and IgM, prevent pathogens from infecting host cells by blocking their ability to attach to and enter the cells.
Defense against Bacteria and Fungi
macrophage oxidative metabolism: The process through which macrophages utilize reactive oxygen species to destroy engulfed pathogens, enhancing their ability to kill bacteria and fungi effectively.
Defense against Parasites
eosinophil activation: The response of eosinophils, a type of white blood cell, during parasite infections, which leads to the release of toxic granules that can damage or eliminate parasitic organisms.
Defense against Viruses
NK cells, interferons, and cytotoxic T cells are used against viruses
Pathogen Recognition and Response
Phagocytosis: Mechanism for engulfing and destroying pathogens (macrophages, neutrophils).
Complement System: Activation leads to pathogen lysis and recruitment of immune cells.
Signaling Molecules: Cytokines enhance communication among immune cells and promote inflammation.
Inflammation and Healing
Inflammation Process: Characterized by redness, heat, swelling, and pain.
Initiated by recognition of tissue damage or pathogens.
Facilitates phagocyte recruitment and promotes healing.
Diseases
Severe Combined Immunodeficiency Disease (SCID): A rare genetic disorder characterized by a severely compromised immune system, leading to increased vulnerability to infections. B and T cells are affected
Hypersensitivity (allergy and inflammatory) Reactions:
Type I: Immediate allergic responses (e.g., anaphylaxis).
Type II/III: Cytotoxic and immune complex-mediated damage.
Type IV: Delayed responses mediated by T cells.
Celiac Disease: An autoimmune disorder characterized by a severe reaction to gluten, leading to damage in the small intestine.
Diabetes Mellitus Type I: An autoimmune disorder where the immune system attacks insulin-producing beta cells in the pancreas, resulting in high blood sugar levels and requiring lifelong insulin therapy.
Graves’ Disease: An autoimmune disorder that results in hyperthyroidism due to the immune system attacking the thyroid gland, often causing symptoms such as weight loss, rapid heartbeat, and excessive sweating.
Hashimoto’s Thyroiditis: An autoimmune disorder where the immune system attacks the thyroid gland, leading to hypothyroidism, fatigue, weight gain, and sensitivity to cold.
Lupus Erythematosus: An autoimmune disease characterized by the immune system mistakenly attacking healthy tissue, resulting in a range of symptoms including fatigue, joint pain, skin rashes, and systemic complications affecting organs such as the heart and kidneys.
Myasthenia Gravis: An autoimmune disorder that affects communication between nerves and muscles, leading to symptoms such as muscle weakness, fatigue, and difficulty in breathing or controlling facial expressions.
Rheumatoid Arthiritis: An autoimmune disorder that primarily affects joints, causing inflammation, pain, and stiffness, which can lead to joint damage and loss of function over time.
Immune Responses Against Cancer
Tissue typing: A process used to determine the compatibility of tissue for transplantation by analyzing the unique genetic markers on the surface of cells, which is crucial for the success of organ transplants and preventing rejection.
MHC polygeny: The existence of multiple genes that encode for Major Histocompatibility Complex (MHC) molecules, which enhances the diversity of the immune response and the ability of the body to present a variety of antigens to T cells.
MHC polymorphism: the variation in MHC genes among individuals in a population, contributing to differences in immune responses and influencing susceptibility to diseases, including how effectively the immune system can recognize and respond to tumor antigens.
graft-versus-host-disease: A condition that occurs when immune cells from a transplanted tissue attack the recipient's body, often seen in bone marrow transplants, where donor T cells recognize the host's tissues as foreign.
erythroblastosis fetalis: A hemolytic disease in newborns, caused by the incompatibility between the blood types of the mother and fetus, leading to the destruction of fetal red blood cells by maternal antibodies.
Tumor Immunology: The role of the immune system in recognizing and targeting cancer cells.
Cancer Immunotherapy: Boosting immune response against tumors using vaccines and immune checkpoint inhibitors.
Conclusion
Understanding the roles and interactions of components within the lymphatic and immune systems is essential for diagnosing and treating immunological disorders, infections, cancer, and conditions resulting from immune dysregulation.