MICB 211 Chapter 12 Notes
Bacterial Pathogenesis and Virulence
Pathogenicity
-bacterium’s ability to cause disease
qualitative
Pathogen
bacterium that is capable of harming a healthy host
may cause harm to healthy host → doesn’t always cause harm
Healthy Host
host whose defence mechanisms are not compromised
Compromised Host
host whose immune defence system is weakened
Opportunistic Pathogen
bacterium that harms a compromised host
Virulence
-measure of the pathogenicity of a microorganism
quantitative
-expressed as the cell number that will elicit a pathogenic response in the host within a given time period
ex: infection with a relatively small number of highly virulent bacteria will kill a certain number of mice whereas an infection with much more of less virulent bacteria is required to kill the same number of mice
-extent of virulence is correlated with ability of pathogen to multiply within the host
may be affected by
route of entry
general health/susceptibility of the host
Virulent Organism
causes disease in most individuals with whom it comes in contact with
Avirulent Organism
rarely causes disease in humans
-virulence of microorganisms is attributable to the fact that they possess virulence factors
allow it to enter and colonize in the host, resist immune defences of host and cause damage in the hose
Bacterial Infections
-classified into
primary infection
secondary infection'
subclinical infection
nosocomial infection
-classified into extent of host involvement
influenced by invasiveness of organism
ie. ability of organism to invade beyond the original site of entry into host’s body
Primary Infection
-initial, acute infection
Secondary Infection
-second/later infection caused by an opportunistic organism after a primary infection has weakened the host defences
Subclinical Infection
-host has no apparent symptoms
Nosocomial Infection
-acquired as a consequence of hospitalization or process of receiving health care
-infection was not present before entering health care facility
Local Infection
restricted to a relatively small area of the body
non-invasive organisms usually cause these infections
Systemic (Generalized) Infection
infection that is spread throughout the body
invasive organisms cause these infections
Focal Infection
begins in restricted area then spreads throughout the body
-host susceptibility influences outcome during infection
interaction between microorganisms and host is affected by virulence of microorganisms and anti-bacterial defences of the host
-susceptibility to infection is increased if anti-bacterial defences of host are compromised
bacteria with low virulence may cause disease in compromised host
-host may be more susceptible to infection if there are factors that compromise immune defences
underlying disease or infection
AIDS, cancer, inherited immunodeficiencies
stress
poor nutrition
lack of essential vitamins/minerals
age
underdeveloped immune defenses of newborn and infant
degeneration of immune response for old people
immunosuppressive therapy
drugs used in treatment of certain cancers
maintenance of transplanted organs
genetics of host’s defence system
individuals in population respond differently to infection
genetic diseases can affect susceptibility to infection
ex: cystic fibrosis, lung infection
some individuals more resistant/susceptible to infections than others
Infecting the Host
Mode of Infection
bacterium has to come in contact with host’s body
bacterium has to adhere to (and transiently colonize) or invade the host
bacterium has to multiply
bacterium has to evade the host’s innate immune defense system
-for bacterium to cause disease → must
possess chemical/molecular mechanisms that damages the host
trigger a chronic inflammatory response
-invasive organisms may cause systemic infections
infection can be disseminated throughout the body
*bacteremia → presence of bacteria in blood
Koch’s Postulates
-Robert Koch established a set of postulates that allow one to determine whether a relationship exists between a particular organism and disease
-proved a causative relationship between most bacterial pathogens and their respective diseases
certain bacterial pathogens can’t be cultivated in vitro
sometimes there are no animal models for a specific disease
Molecular Version of Koch’s Postulates
gene(s)/factor should be present in pathogenic strains of the organism and absent from non-pathogenic strains
molecular disruption (eg. deletion of genes) should reduce the virulence of bacterial strains and introducing the cloned gene(s) into an avirulent strain should render the strain virulent
gene(s) must be expressed at some point during the infectious process in experimentally infected animals
antibody raised against the virulence factor should offer some protection against infection in an experimentally infected animal
Regulation of Genes Encoding Virulence Factors
Virulence Factors
disease-causing genes described in molecular version of Koch’s postulates
possession of virulence factors is what allows pathogenic bacteria to infect normal people and cause disease
-a particular bacterium may live in many different environments
may need to regulate the expression of components needed for survival in varying conditions
-bacteria may turn on these different components which include virulence factors only when needed
Environmental Factors
temperature
nutrients
oxygen
pH inside the cell
iron availability
osmolarity
-common processes regulated at the genetic level includes metabolism, response to environmental stresses and conditions, and cell division
-many virulent bacteria have global regulatory systems to regulate virulence factors
these systems are co-ordinately regulated by a two-complement system that comprises a sensor protein and a regulator protein
common system for signal transduction
-sensor (kinase) protein detects changes in environment that indicate that the bacterium is residing inside a human host and then phosphorylates the response regulator protein
-phosphorylated regulator protein then transcriptionally activates or represses the virulence factors by binding to a DNA sequence in the regulatory regions of each of the operons for these virulence factors
Virulence Factors: Mechanism of Pathogenic Bacteria
Bacterial Adherence
-first host barrier for many invading pathogens is usually a mucosal surface
gut or respiratory tract
-most successful pathogens have evolved specific mechanisms to adhere to host tissue
-simple attachment is mediated through a receptor on the host cell surface (glycoproteins, glycolipids) and an adhesion (pili, capsule) on the surface of the bacterial cell
-these mechanisms benefit the pathogen by facilitating colonization, preventing the removal of the bacterium by non-specific host defence systems and by localizing the bacterium to the appropriate tissue
-specificity of interaction between host and bacterium is
host-specific
tissue-type specific
-pili allows bacteria to mediate adherence to host cells
pili have a range of different functions
motility
conjugation
host cell adherence
-host responds to adherent organisms through
production of antibodies against bacterial surfaces
upregulation of production of antimicrobial peptides by epithelial cells
phagocytosis of the adherent organisms
shedding/destruction of epithelial cells that become colonized with bacteria
Capsules
-many pathogens have evolved surface components that prevent attachment and engulfment of macrophages and other host cellular immune responses to avoid phagocytosis
aided by
membrane bound proteins
slimy polysaccharide capsules
lipopolysaccharides (Gram(-)) only
these factors prevent the deposition of antibodies and complement on bacterial surface
avoiding complement-mediated killing and reducing phagocytosis
Toxins
-microbial products that can damage the host
-capable of causing disease, independent of the bacterium
ex. pathogenic bacteria can be killed in a patient but disease may persist due to continued action of toxin
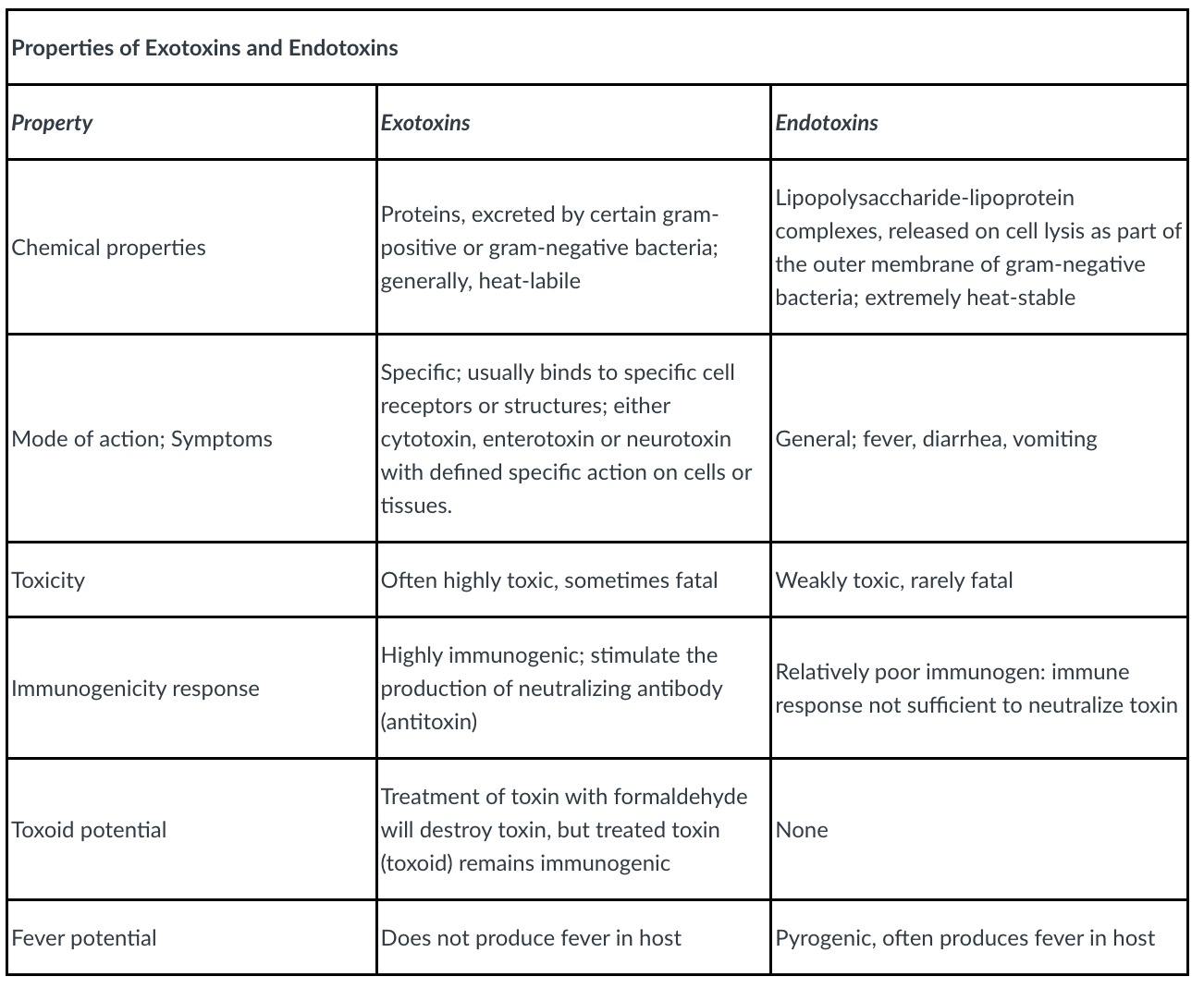
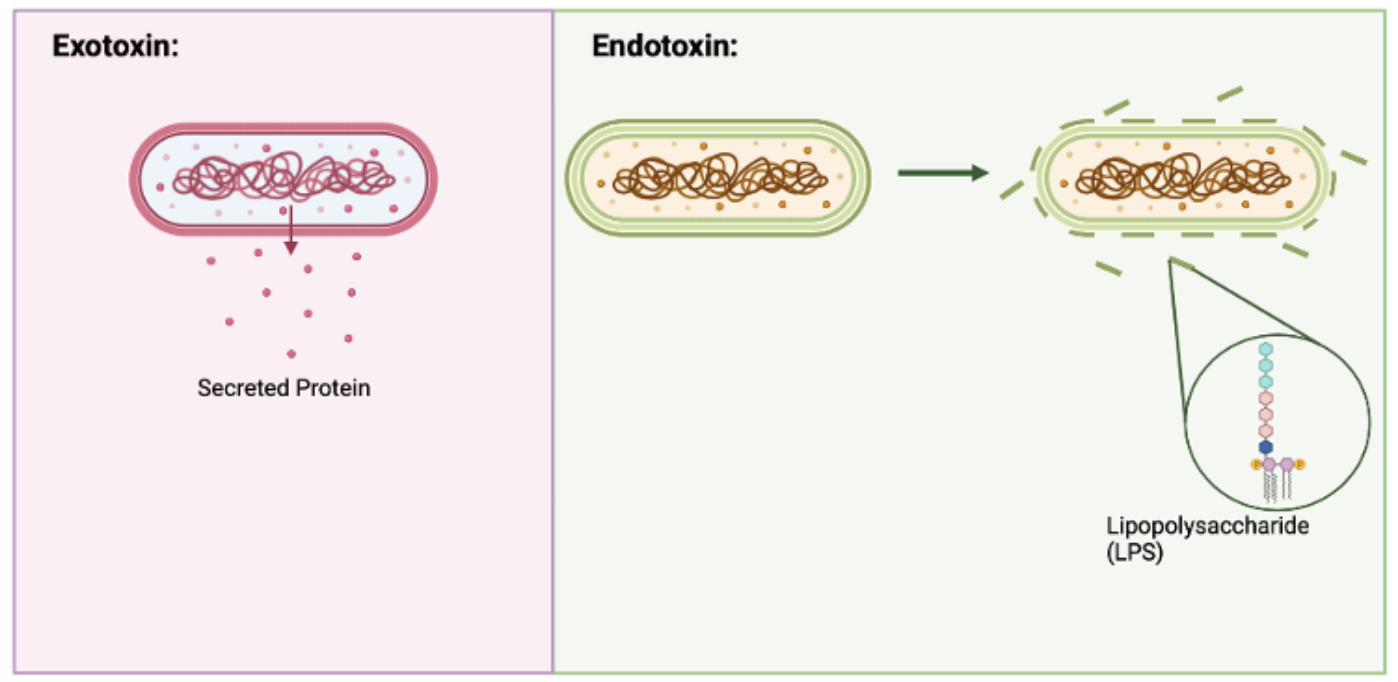
Exotoxins
-secreted proteins made by both Gram (+) and Gram (-) bacteria
-toxins may enter blood circulation and spread to parts of body and cause damage far from site of bacterial colonization
-3 main categories
cytolytic toxins
enzymatically attack the cell constituents causing cell lysis
neurotoxins
interfere with nerve cell function
enterotoxins
affect cells lining the GI tract
causes massive fluid secretion (diarrhea)
-potent molecules
small dose can have a significant effect on host
-proteins
-usually heat labile
-immunogenic
stimulates immune system to produce neutralizing antibodies
-vaccination against toxin-mediated diseases can be done by immunization with toxoids
Toxoids
toxins that have been treated with heat or chemicals to make them non-toxic to patient
still capable of stimulating production of neutralizing antibodies
Endotoxins
-released only when bacteria die or are digested by phagocytic cells
-non-protein molecules that are heat stable
-generally associated with LPS (gram (-))
-activates macrophages causing release of inflammatory cytokines
-low doses (< 1 mg) → patient might experience fever, aches, pains
-higher doses → damage to circulatory system and shock
Endotoxin Shock
fluids leak out of blood vessels, blood coagulates, blood pressure drops, organs fail and death may result
treatment includes supportive therapy
no antibiotics (aggravates LPS/endotoxin release)
no vaccine since endotoxins are non-protein molecules (not immunogenic)