Inflammatory Heart Disease
Inflammatory Heart Disease Notes
Learning Objectives
Identify the layers of the heart.
Understand the different etiologies and risk factors for:
Pericarditis
Myocarditis
Endocarditis
Differentiate clinical findings in:
Pericarditis
Myocarditis
Endocarditis
Anticipate diagnostic tests for evaluating inflammatory heart disorders.
Plan nursing interventions and care for patients with inflammatory heart disease.
Understand the consequences of untreated inflammatory heart disease.
Identify patient education points for health promotion related to infectious heart diseases.
Layers of the Heart ( ๑‾̀◡‾́)σ"
Pericardium (outermost layer of heart):
Fibrous pericardium (outermost layer)
Serous pericardium (parietal layer)
Serous visceral (epicardium, on the heart muscle itself)
Myocardium (middle): Thick muscle layer with cardiac fibers.
Endocardium (innermost layer): Inner endothelial lining. Makes up heart chambers and valves themselves.
Acute Pericarditis (๏ᆺ๏υ)
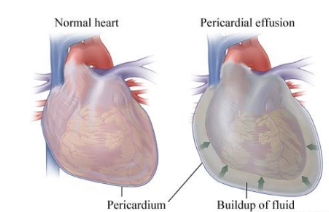
Definition: Inflammation of the pericardial sac/Inflammation outside the heart.
Heart gets compressed and cannot pump. Less cardiac output = less oxygen out.
Etiology:
Idiopathic: Unknown cause.
Infectious: Viral, bacterial, fungal, parasitic.
Noninfectious: Acute myocardial infarction (AMI) (leads to inflammation cascade triggers immune system), renal failure, certain cancers, trauma, radiation, myxedema (severe hypothyroidism/swelling/thickening of skin), dissecting aortic aneurysm.
Autoimmune (hypersensitivity type III): Dressler’s syndrome (pericarditis after heart injury with fluid buildup in peri sac), post-pericardiotomy syndrome (surgery complication), rheumatic fever (related to strep throat infection), RA.
Think “HAIR”
H: Heart attack → noninfectious
A: Autoimmune Disorders → RA, SLE (lupus), scleroderma (hardening of skin), Dressler’s syndrome, rheumatic fever.
I: Infection → Viral (HIV), bacterial (strep, staph), fungal (candida), parasitic.
R: Renal Failure → Uremia (high BUN) → noninfectious
Pathophysiology
Acute inflammatory response leads to:
Influx of neutrophils.
Fluid leakage into the pericardial sac.
Increased vascularity (vessel size) and fibrin deposition on the epicardium (decreases movement of heart).
Acute Phase: Occurs within 24-48 hours after MI.
Subacute Phase: Occurs weeks to months later (e.g., Dressler syndrome).
Chronic Phase: Lasts over 6 months; leads to friction and adhesions affecting heart movement.
Clinical Manifestations
Severe chest pain that worsens with deep inspiration or lying flat, relieved by sitting up and leaning forward (tripod).
Referred pain to shoulders/back.
Fever (infectious etiology), tachypnea, dyspnea, anxiety.
Pericardial friction rub (hallmark finding): Scratchy, grating, high pitched sound heard best at the left lower sternal border.
Request pt hold their breath and listen to determine if pleural friction or pericarditis because heart will still beat.
Diagnostic Testing
ECG: Global ST segment elevation.
Echocardiogram: To assess effusion or tamponade.
Imaging: CXR, CT or MRI for visualization of the pericardial sac.
Lab Work: CBC (RBC, WBC), CRP (Inflammatory markers → CRP normal <1), Sed Rate, Troponin (released with cardiac cell death).
Pericardiocentesis: Fluid analysis (diagnostic and treatment).
Complications
Pericardial Effusion: Excess fluid leading to muffled heart sounds, potentially compressing the heart.
Hiccups → phrenic nerve compression
Hoarseness from laryngeal nerve compression
Lungs - cough, SOB, increased RR
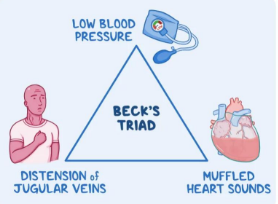
*Cardiac Tamponade: Reduced diastolic filling & cardiac output and pulsus paradoxus (SBP decreases w/inspiration), requiring urgent pericardiocentesis. Happens when there is a 1000ml in peri sac. MEDICAL EMERGENCY.
Beck’s Triad: Low blood pressure, muffled heart sounds, JVD.
Interprofessional Care
Medications: Antibiotics (if infectious), NSAIDs (unless related to MI), corticosteroids (decrease inflammation → long-term use decreases immune function), colchicine (helps inhibit neutrophils→ decreases inflammation and fluid).
Supportive: Oxygen, bed rest (perform turns, ROM, nutritious meals), positioning (tripod).
Uremic Pericarditis: Needs dialysis (renal failure).
Surgical Interventions:
Pericardiocentesis → fluid drainage
Pericardial “window.” → remove portion of pericardial sac and fluid spills into pleural cavity → reabsorbs into body
Indications: Cardiac tamponade, purulent pericarditis drainage, malignancy.
Potential Complications:
Dysrhythmias from sudden drainage
Pneumothorax
Chronic Constrictive Pericarditis
Definition: Fibrosis (thick) and rigidity of the pericardium, leading to decreased elasticity, restrictive ventricular filling (diastole) → reduced cardiac output.
Etiology: Tuberculosis, heart surgery, radiation therapy, idiopathic.
Clinical Manifestations: Symptoms resemble right-sided heart failure and Cor Pulmonale (dyspnea on exertion, edema, ascites, JVD), fatigue.
Treatment: Pericardiectomy (remove pericarditis) and diuretics (decreases preload/diastolic filling)
Acute Myocarditis (ᗒᗣᗕ)՞
Definition: Inflammation of the myocardium (thick muscle layer with nerves).
Contains all cardiac fibers and nerves like bundle of His and Purkinjie fibers.
Etiology: Infectious (viral, bacterial, fungal), noninfectious (radiation, drugs), or idiopathic.
Generally related to bacterial etiology.
Pathophysiology of Myocarditis
Causative agents invade and damage myocytes -> trigger an immune response → cytokines release → autoimmune inflammation (body attacks self) → necrosis.
Clinical Manifestations of Myocarditis
Early symptoms: Fever, fatigue, myalgia/muscle aches, pharyngitis (especially if damage to nerves), lymphadenopathy (enlarged lymph nodes).
Cardiac signs (if present) can appear 7-10 days after infection
Leads to pericarditis → pleuritic chest pain (increases with inspiration), pericardial rub.
Pericardial effusion.
Late signs may include heart failure symptoms: S3, crackles/rhonchi, peripheral edema, JVD.
Diagnostic Testing for Myocarditis
ECG: ST segment changes, dysrhythmias, conduction abnormalities (inflammation of myocardium fibers and nerves).
Echocardiogram: Assess effusion or tamponade.
Lab tests: CBC, troponin (will be elevated similar to a heart attack due to necrosis from autoimmune reaction to myocytes), and viral titers.
Endomyocardial Biopsy
Complications of Myocarditis
Decreased cardiac output; severe heart failure (related to dilated cardiomyopathy) or sudden cardiac death (dysrhythmias related to conduction abnormalities, HF → EJ will drop due to dilated CMP).
Severe HF management may require advanced support such as intra-aortic balloon pumps or heart transplant.
Medications: Ace, beta, diuretics to manage HF s/s
digoxin, anticoagulants, causative treatment aka antivirals or immunosuppressive)
Infective Endocarditis (IE) =^● ⋏ ●^=
Definition: Infection of the endocardium affecting cardiac valves.
Etiology: Bacterial, viral, or fungal.
Two Main Classifications: Acute (rapid manifestations of valvular dysfunction) of subacute (preexisting valve disease with clinical course → stenosis)
Risk Factors for Endocarditis
Previous instances of IE, IV drug abuse, age-related changes, prosthetic valves, invasive procedures (pacemaker, dialysis, central lines, surgery), dental surgery.
Pathophysiology of Endocarditis
Three Stages:
Bacteremia (bacterial invasion)
Adhesion: Damage to endothelium supports the attachment of infective organisms.
Vegetation: Fibrin, leukocytes, platelets, and microbes stick to the valve or endocardium.
Left-sided can move to brain (altered LOC), kidneys (oliguria or anguiria), spleen (left upper quadrant pain and immune function decreases), extremities (pallor).
Right-sided can cause a PE
Clinical Manifestations of Endocarditis
Nonspecific symptoms (acute → weakness, malaise, fatigue) and signs involving multiple organ systems. Subacute involves back pain, abdominal discomfort, anorexia. Vascular manifestations include splinter hemorrhages, petechiae. New or changing systolic murmur.
Diagnostic Testing in Endocarditis
Blood cultures twice from different sites, ESR, CRP, echocardiography (US of heart), and Duke criteria to establish diagnosis (major = pos blood culture, pos IE organism, new vegetation).
Health history, recent dental surgery, ask if they’ve had infective endocarditis
Complications of Endocarditis
Systemic embolization of vegetations, heart valve damage, myocardial invasion leading to heart failure, and potential for sepsis.
Non-specific: Fever, malaise, fatigue.
Interprofessional Care for Endocarditis
Prophylaxis with antibiotics for susceptible patients, tailored based on blood culture results. Long-term IV antibiotics may be necessary. Follow-up diagnostics and supportive care are crucial.
Supportive Care: Treating signs and symptoms (ex. Fever → give antipyretics, hypotensive → fluids (unless HF symptoms), rest)
Valve Replacement: The bacterium must go away first.
Trend ESR and CRP
Rheumatic Heart Disease ᕙ(⇀‸↼‶)ᕗ
Subtype of Endocarditis
Rheumatic fever can affect all heart layers
Delayed complication following a stream throat infection → rheumatic fever → rheumatic heart disease.
Body develops autoimmune response to strep bacteria
Education: Don’t share utensils, take full course of antibiotic
Early recognition: Get treated if sore throat and witness white patches on throat
Clinical Manifestations of Rheumatic Heart Disease
Features include arthritis, carditis/pancarditis (heart murmur, HF, pericarditis), and other systemic symptoms such as erythema and involuntary movement.
Diagnostic Studies for Rheumatic Heart Disease
Physical examination, lab work, echocardiogram for valvular dysfunction, and ECG.
Nursing Care: Includes administration of prophylactic antibiotics for those with prior RF (q3-4 weeks IM injection until symptoms subside) wand anti-inflammatories to manage symptoms and prevent complications.