Test Motor Speech
1/195
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
196 Terms
What is hypokinetic dysarthria caused by?
any procress that damages basal ganglia causing dysfunction, causes dysfunction to BG's neural connections to other parts of the CNS
what are the speech characteristics of hypokinetic dysarthria?
- harsh vocal quality
- reduced stress
- monoloudness
- imprecise consonants
* may manifest in all levels of speech
Hypokinetic =
less motion
Hypokinetic dysarthria is the only dysarthria with?
- increased rate as a symptom
- mainly one causative factor (Parkinsonism)
What is Parkinsonism?
a collective term for different disorders sharing similar symptoms of:
- resting tremor
- Bradykinesia (slow movement)
- rigidity
- spasticity
- akinesia (delay in initiation of movement )
- postural reflexes
What causes Parkinsonism?
- dysfunction in basal ganglia
- varied causes of reduced dopamine
The basal ganglia depend on a balanced interaction of several neurotransmitters, including:
- dopamine (inhibitory)
- acetylcholine (excitatory)
What are the functions of the basal ganglia?
- regular muscle tone
- regulate movements that support goal-directed movements (arm swing while walking)
- control postural adjustment during skilled movements (writing)
- adjusting movements to the environment
- assist in learning new movements
What are the clinical characteristics?
- tremor at rest
- rigidity "cogwheel"
- Bradykinesia
- Hypokinesia (masked facies, micrographia, festinating gait)
- loss of postural reflexes (unable to make adjustments to tilting/falling, difficulty turning in bed
What is a festinating gait?
small rapid steps resulting from a forward-tilted head and trunk posture
What are the etiologies of hypokinetic dysarthria?
- degenerative disease (idiopathic PD)
- vascular (stroke in BG)
- traumatic (boxing)
- Inflammatory
- Neoplastic
- Toxic
- Metabolic
What is Parkinson's Disease
An idiopathic neurologic disease that affects movement, balance, and coordination due to loss of dopamine in the basal ganglia
* may be unilateral initially
Individuals with parkinsons are
- typically > 50 years in age
- 1/3 may have dementia
- may have depression
PD may be affected caused by these factors:
- environmental influences: rural living, well water, exposure to herbicides, pesticides, and maganese (in iron)
- genetic susceptibility
- combo of the two
What are the medical management options for PD?
- Levadopa or Sinemet: transfers into dopamine
- dopamine agonist (Bromacriptine, Mirpex, Ropinarol) stimulates DP receptors
- anticholinergics (amantadine) to help tremor
- Neurprotective drugs (Eldepryl) thought to slow progression for 2-3 years
What are the medication side effects?
they have an on/off cycle and can have hyperkinetic symptoms
What are the surgical management options?
- globus pallidus target
- thalamus target
- subthalamus target
* all are complicated and invasive, not always helpful. may be an option if medication isn't effective
What are Globus Pallidus Target surgeries?
- done to disrupt inhibitory outflow (overactivity)
* pallidotomy: destroys tissue
* pallidal stimulation: is reversible
What are the Thalalmus target surgeries?
- used primarily for tremor
* thalamotomy
* thalamic stimulation
What is the subthalamus target surgery?
deep brain stimulation
What impact does medical management have on speech/voice?
- magnitude and consistency of speech improvement with drugs is not the same as with limbs (limbs improve, speech may not)
- deep brain stimulation: no concrete research on whether there is improvement or not, swallowing is still being investigated
what are the conditions of Parkinsonism?
- progressive supranuclear palsy (PSP)
- MPTP (street drug) causes same signs/symptoms as PD
- Trauma-induced Parkinsonism - "punch drunk"
- TBI
- Vascular Parkinsonism - stroke in area of BG
- Pick's disease - dementing illness with changes in frontal and temporal lobes
What are the pt complaints/symptoms of hypokinetic dysarthria?
- voice quiet or weak, cannot be heard in noise
- rate too fast
- indistinct words
- lack of emotional tone
- difficulty to get started
- palilalia (disfluent)
What are the perceptual signs of hypokinetic dysarthria?
- monopitch
- reduced stress
- monoloudness
- inappropriate silences
- short rushes of speech
- variable rate
- increased rate in segments
- increased rate overall
- reperated phonemes
What are the prosodic characteristics of hypokinetic dysarthria?
- monopitch
- reduced stress
- monoloudness *most common
What are the articulation characteristics of hypokinetic dysarthria?
- imprecise consonants
- repeated phonemes
- palilalia (disfluency)
What are the phonation characteristics of hypokinetic dysarthria?
- harsh/breathy quality
- aphonia
- low pitch
What are the respiraion characteristics of hypokinetic dysarthria?
sometimes noted
- shallow breaths cause short phrases
What are the resonance characteristics of hypokinetic dysarthria?
if present, mild hypernasality
What does the nonspeech exam look like for hypokinetic dysarthria?
- face: unblinking, unsmiling, masked, expressionless at rest, lack of animation
- swallow infrequently, drooling
- tremulousness of jaw and lips during rest or sustained posture
- AMRs slowly initiated and become accelerated
- dysphagia on 40%-8-% (later onset
What are the key evaluation tasks for hypokinetic dysarthria?
- conversational speech and reading: evoke many errors of prosody, detect short rushes
- speech alternate motion rates (AMRs): highlight artic errors
- vowel prolongations: to assess vocal quality
What are behavioral treatments for Parkinsonism?
- behavior and instrumentation-based tasks are an important part of clinical treatment plan
- articulation: rate reduction, stretching, traditional artic tasks
- phonation: pushing and pulling procedure, hard glottal attack; voice amplifiers; instrumental biofeedback; LSVT, SPEAK OUT!
What is Lee Silverman Voice Treatment (LSVT)?
- THINK LOUD
- 5 concepts: 1) focus on voice 2) high effort 3) intensive 4) calibration 5) quantifiation
- daily homework
- 4x week for 4 weeks
What is Speak Out!
- individual and group sessions
- "speak with intent"
- daily homework
- 2-3 week initally, 1-2 group
What are the treatments for respiration?
shallow breaths cause short phrases and decreased loudness
- speak immediately on exhale
- cue for complete inhale
- slow and controlled exhale
- stop phoantion early
- optimal breath group
What treatments are for prosody?
*improve by slowing rate
- intonation profiles
- contrastive stress drills
- chunking utterances into syntactic units
Other treatment options:
- rigid rate control (DAF, pacing board)
- vocal intensity monitors, feedback devices
- vocal amplifiers
- posture
- Intensive programs to help learn new behaviors
What is ataxic dysarthria?
motor speech disorder due to damage to the cerebellum or its neural pathways, resulting in speech errors that are primarily articulatory and prosodic making speech unsteady and slurred
What is the cerebellum?
The cerebellum is the part of the brain associated with voluntary responses.
* ERROR CONTROLLER of movements
it receives "copy" of. mvoement plan/program, then comprares plan vs reality and provides feedback to cortex, then cortex alterns plan
- part of the indirect pathway to LMNs
What does the cerebellum do?
controls speed, muscle tone, and range of muscular movements
- helps coordination of skilled movement
Vermis of cerebellum has what
speech functions
Cerebellum has what type of control of the body?
ipsilateral control
-R Cortex, L Cerebellum, L Side of body (talks through cotrex)
- L Cortex, R Cerebellum, R Side of body
What is ataxia?
results from cerebellar control circuit dysfunction
- causes slowness and inaccuracy im force, range, timing, and direction resulting in difficulty with coordination of movement
What are the signs of cerebellar lesions?
- hypotonia (lack of muscle tone)
- slow voluntary movements
- jerky movements
- wide-based gait
- intention tremor (when making a movement )
- terminal tremor
- truncal titubation (extra movement in trunk area of body)
- dysmetria (inability to judge distance, speed, and force of movements)
Lesions in cerebellum cause
- mild weakness
- tremors
- lack of movement
- muscular incoordination
- impairments of equilibrium (balance)
What causes ataxic dysarthria?
- degenerative diseases
- vascular diseases
- neoplastic disorders
- trauma
- toxic/metabolic conditions
What is friedreich's ataxia?
a progressive, hereditary disease that affects the spinal cord and cerebellum
What is multiple sclerosis (MS)?
a disorder of gradual destruction of myelin sheaths (brain, spinal cord, optic nerves)
1) myelin is attacked then plaque/scar forms and slows down transmission of electrical impulse that will result in movement
*causes mixed dysarthria (spastic-ataxic)
What is paroxysmal?
sudden brief dysarthria attacks
Lesions from strokes are typically caused by
- aneurysms (rupturing)
- arteriovenous malformations
- cerebellar hemorrhage
- occlusion of vertebrobasilar systems
What is a neoplastic disorder?
- a tumor or growth
- may be inside or outside of cerebellum (putting pressure on it)
- 25% of metastatic brain tumors develop in cerebellum
- cerebellopontine angle tumors - involve multiple cns
Trauma that causes ataxic dysarthria?
- damage to cerebellum during TBI
- damage resulting in anoxia during TBI (superior cerebella peduncles can be damaged if brain rotates on brainstem)
** boxers may sustain cerebellar injuries (punch-drunk)
What are toxic/metabolic conditions?
celebellar degeneration occurs in chronic alcoholics (results of malnutrition of vitamin deficiency) ** like Wernicke's syndrome (chronic
- toxic levels of drugs (anticonvulsants, lithium, valium)
What is normal pressure hydrocephalus?
enlarged ventricles but normal cerebrospinal fluid pressure
*can be treated by shunting in first 6 months
What does speech look like for ataxic dysarthria?
- irregular and transient articulatory breakdowns
- irregular vowels distortions
- excess and equal stress (scanning) - every work is stressed
- excess loudness
- dysprosody * can cause prolonged phonemes (lack of melody due to pitch, quality, strength, and duration)
- irregulars AMRs
Bilateral cerebellar lesions and occuring in the vermis cause
- dysarthria
- errors of force, speed, timing, and range causing difficulty with coordination of movements
*primarily of disorder or articulation and prosody
How is respiration affected in ataxic dysarthria?
- uncoordinated movements in respiratory muscles = contribute to speech deficits
- paradoxical movements rather than in coordination
What are paradoxical movements?
movements of intercostal muscles and diaphragm that occur when muscles work against each other rather than in coordination
Paradoxical movements lead to what
pt having to speak on residual air, which can lead to increased rate of speech, decreased loudness, and harsh vocal quality
What are the phonatory deficits related to ataxic dysarthria?
harsh vocal quality - caused by decreased muscle tone in laryngeal and respiratory structures, preventing full contraction on these muscle groups
- voice tremors
What are the resonance deficits related to ataxic dysarthria?
- hypernasality (seldom)
- hyponasality (intermittent) caused by timing errors between muscles of velum and other muscles of articulation
What are the articulatory deficits related to ataxic dysarthria?
*this is a significant problem
- imprecise consonant production
- distorted vowels
both give the slurred quality due to cerebral damage due to timing, force, range, and direction of movements
- irregular articulatory breakdowns: imprecise consonant and vowel production vary from utterance to utterance
- decomposition of movement: manifestations of cerebellar dysfunctions; movements are distinct and jerky
What are the prosody deficits related to ataxic dysarthria?
- equal and excess stress (scanning)
- prolonged phonemes and prolonged intervals between phonemes - slow movement on both single and repetitive tasks (hypotonia)
- monopitch and monoloudness caused by hypotonia
What are the symptoms of ataxic dysarthria?
- "drunk" speech
- stumbling over words
- biting tongue/cheek when speaking/eating
- speech deteriorates w/ alcohol consumption
- poor respiratory coordination during speech
What are the key evaluation tasks for ataxic dysarthria?
- speech AMR tasks: will be slower than normal, difficulty maintaining steady rhythm with repetition / severe cases: speed up abruptly then unexpectedly slow down
- reading, conversational speech, and repeating sentences containing numerous multisyllabic words
- measures of intelligibility - functional assessment
What does management of ataxic dysarthria look like?
focus: improving motor control and coordination
- cerebellar implants to help with gross motor skills not with speech
- rate and prosody modification to improve intelligibility and naturalness
How do you treat respiration impairments in ataxic dysarthria?
* you do not need to address strengthening respiration
concentrate on controlling airflow more accurately during speech as uncoordinated movements of respiratory muscles cause speech on residual air, affecting prosody and phonation
What tasks can be done to work on respiration?
tasks to improve breath control during speech
- slow and controlled exhalation
- speak immediately on exhalation
- stop phonation early (before running out of air)
- optimal breath group (teach how many syllables or words can be said during full inhalation)
How do you treat prosody deficits in ataxic dysarthria?
problems involve rate, stress, intonation
work on slowing rate, improving intelligibility, and incorporating more typical stress and intonation into utterances for more natural quality
What does rate look like with ataxic dysarthria?
slow and irregular rate, may attempt to speak at too rapid for speech capabilities
What are some rate control tasks?
- reciting syllables to a metronome
- finger or hand tapping (pacing board)
- cue reading material
What are some stress and intonation exercises?
- contrastive stress drills
- pitch range exercises
- chunking utterances into syntactic units
How do you treat articulation deficits in ataxic dysarthria?
- improve slowed rate
- improve production of phonemes
- articulation tasks
What are articulation tasks?
- intelligibility drills
- phonetic placement
- exaggerating consonants (over articulating)
- minimal contrast drills
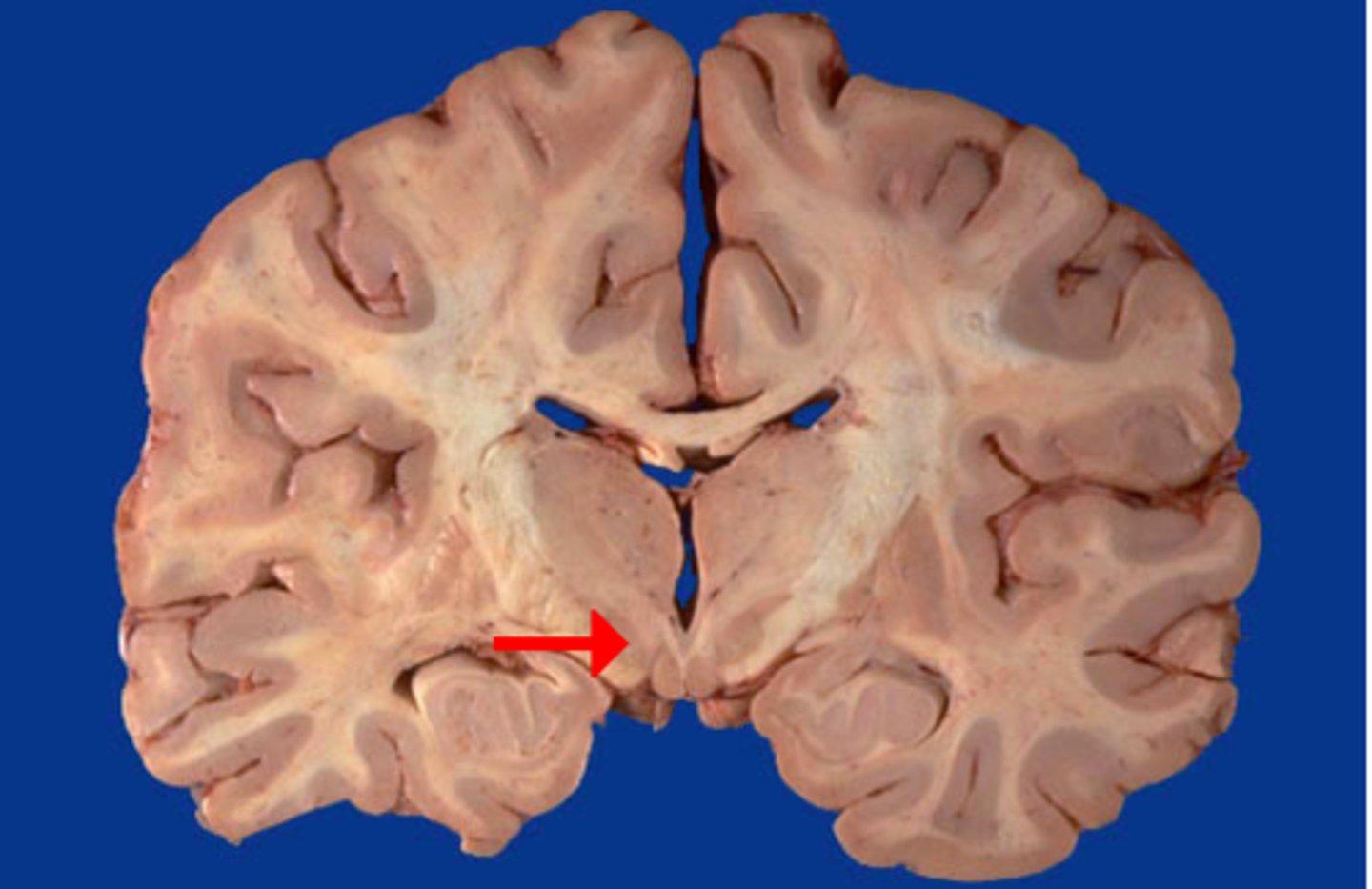
What causes spastic dysarthria?
bilateral upper motor neuron damage
Spinal motor neurons innervate what?
limbs
If spinal motor neurons have unilateral innervation that are _____________ to the body
contralateral
Cranial motor neurons have what kind of innervation
bilateral
What are the exceptions to bilaterally innervated CNs?
CN VII to muscles of lower face; XII weak ipsilateral innervation
LMN pathways receive input from where?
UMN pathways (pyramidal and extrapyramidal)
Pyramidal pathways consist of what?
corticobulbar (brain to brainstem) and corticospinal (cortex to spinal nerves) tracts that arise from the motor cortex
Most corticobulbar tracts travel through what?
corna radiata and internal capsule
* damage here lead to a large deficit
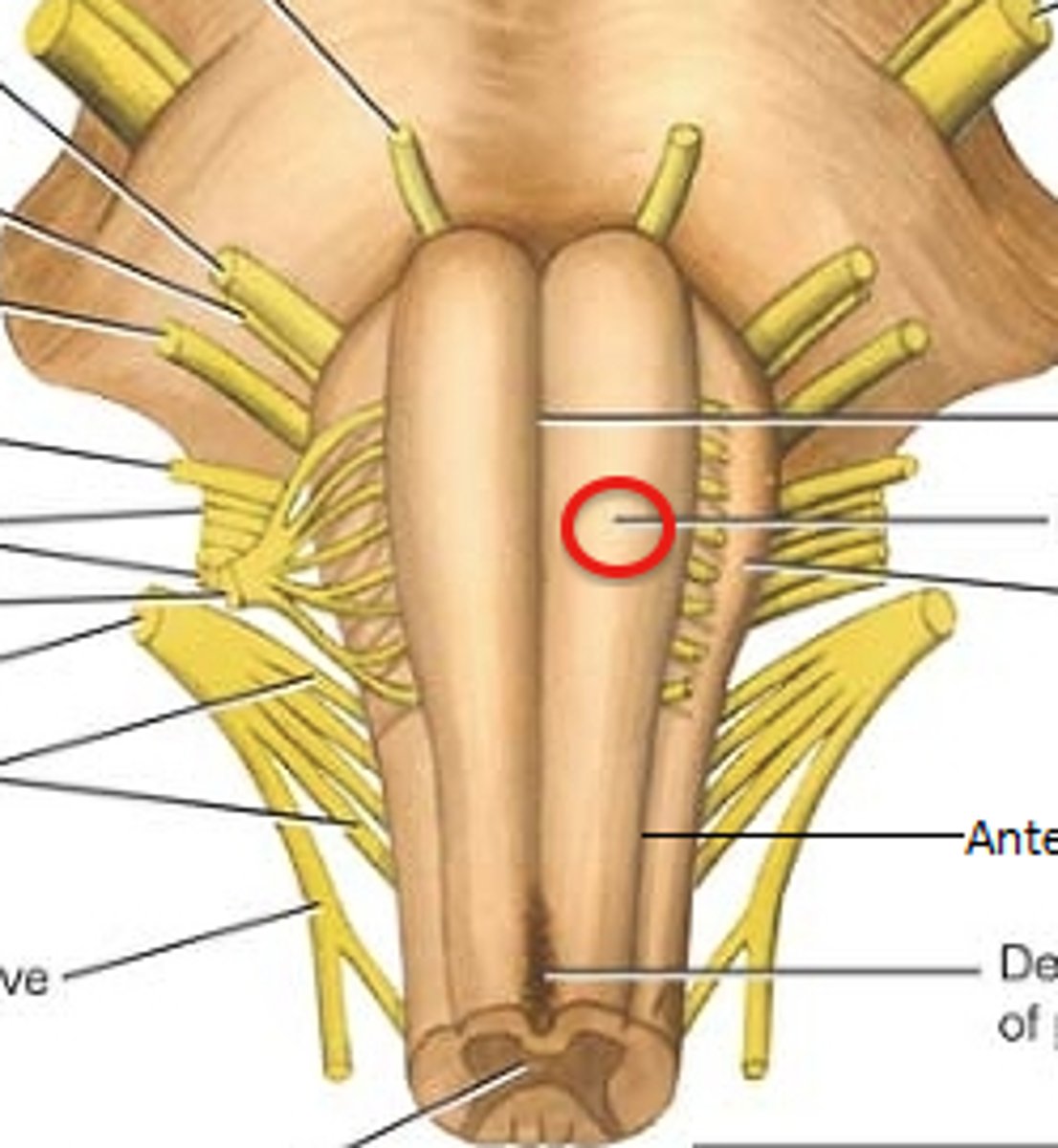
What do UMN (pyramidal pathways) facilitates what?
movement; activation leads to movement (discrete and skilled movements)
What do UMN (pyramidal pathway) lesions cause?
- weakness
- loss of skilled movements
- decreased tone
UMN (extrapyramidal pathways) have contributions from premotor areas and make connections with
- basal ganglia
- cerebellum
- other areas (not speech related)
Extrapyramidal pathways are
inhibitory (take away some movement) - regulate reflexes for maintaining posture and tone
What is the babinski sign?
tickle foot, toe goes up. not normal after age 2
*indicates UMN damage
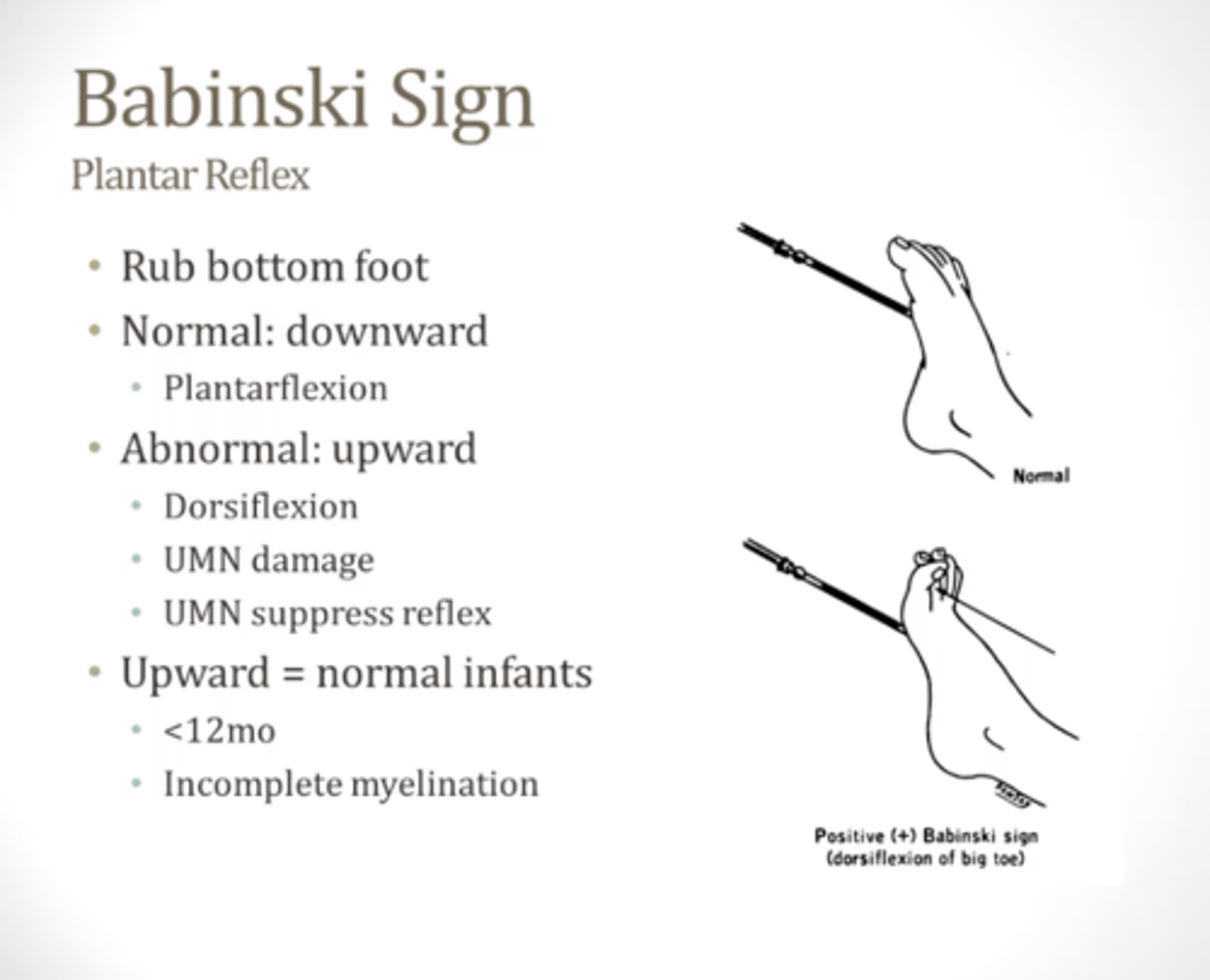
What is spasticity?
a hallmark sign of UMN damage
- hyperactive reflexes (clonus)
- increased tone
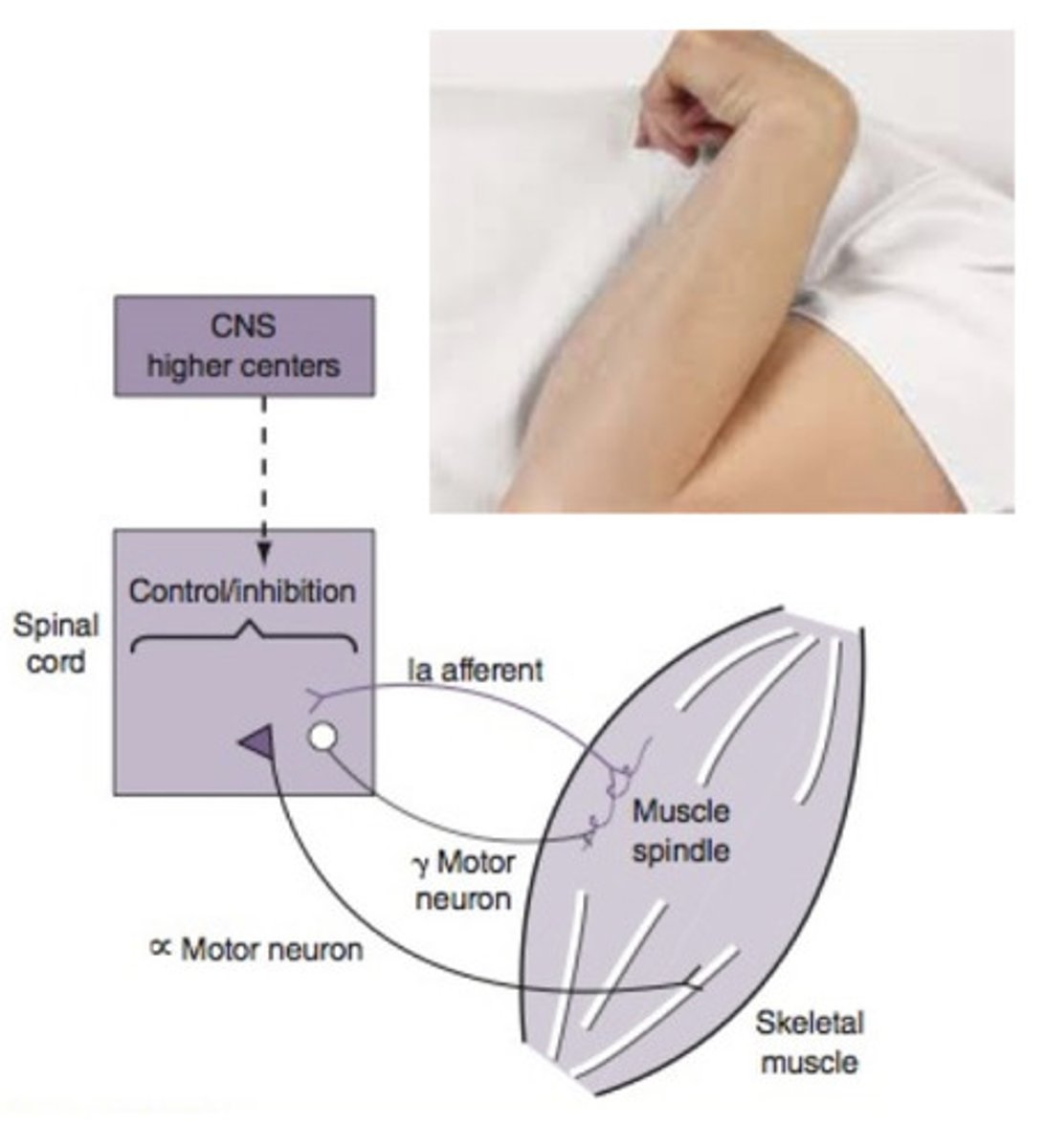
Damage/lesions in UMN leads to what
loss of inhibition
LMN are more excitable due to what?
the lack of UMN inhibition and responds more to smaller inputs
* results in too much electrical signal which can be see as spasticity
Damage in both the pyramidal and extrapyramidal damage (in UMN) results in what?
- paralysis/paresis
- loss of skilled movement
- spasticity
- increased reflexes
- pathological reflexes (reflexes that should've been outgrown)
- no atrophy
Pyramidal track damage results generally in...
paralysis/paresis and loss of skilled movement
Extrapyramidal track damage results in ...
"positive" signs (spasticity, increased or pathological reflexes) ***disinhibition
What is the UMN innervation for the trigeminal nerve?
bilateral
What is the UMN innervation for the facial nerve
bilateral (predominantly contralateral)
What is the UMN innervation for the glossopharyngeal nerve?
bilateral
What is the UMN innervation for the vagus (all branches) nerve?
bilateral
What is the UMN innervation for the hypoglossal nerve?
contralateral > bilateral
How does UMN damage impact LMN?
LMN still works but gets impaired input from UMN
Clinical characteristics of spastic dysarthria?
spasticity, weakness, reduced ROM, slowness of movement