3.3 MSK considerations for the Elderly
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
What are some factors that change biologically with age
discs
ligaments
joint capsules
articular cartilage
muscle
bone density
What are the disc impairments
decreased water in nucleus
increased fibroses of annulus
What do the disc impairments lead to
flatter less resilient disc
Why do the discs have decreased water in the nucleus
dehydration
What are some pathologic changes due to aging
neurologic disease
arthritis
cardiopulm complications
postural hypotension
What can bone on bone diseases lead to
potential bone spurring
What can cause the bone on bone disease
changes in spinal curvature
What does impingement cause
numbness
tingling
loss of light touch sensation
long term effects of impingement
parathesis or paralysis
Once impingement leads to weakness, what treatments are available
may have to consider surgery
What can impingements do changes in posture lead to
balance issues (changed COG)
What may help with postural changes effect on fall frequency
assistive devices
Typical posture for elderly populations
head forward
thoracic kyphosis
lumbar lordosis
hip flexion
knee flexion
What issues can head forward posture lead to
cervical pain
What issues can increased thoracic kyphosis posture lead to
respiration/thoracic wall movement
scapular resting position (weakening in postural mm)
common postural changes
hip flex
knee flex
valgus/varus
decreased/increased lumbar lordosis
loss of height
What can decreased lumbar lordosis lead to
arthritis
What can increased lumbar lordosis lead to
weakened abs
What is an intervention for postural changes
extension (back bends, cervical retraction, chest puffing, prone on elbows, scapular retraction)
age related changes to strength
Decreased number and size of muscle fibers (strength)
decreased rapid muscle force exertion (power)
age related changes to pain
decreased ability to localize pain
decreased production/use of enkephalin
decreased report of pain due to social pressures
age related changes to hypokinesis
more sedentary lifestyle (sitting in flexed posture in recliner)
What type of muscle fibers are present in elderly
decreased Type 2, increased type 1
CV strength impairments
inefficiently leads to poor nutrient exchange
neuromuscular junction strength impairments
contract inefficiently
Other strength impairments
pathology (Parkinson’s/strike)
MSK strength impairments
swelling, joint distension
What is joint distension
enlargement of the joints causing difficulty in completing activities
Interventions for strength
increase activity levels
modalities and anti-inflammatory medication
How can exercise be beneficial
increases blood flow to the mm
improve nerve conduction velocity (reaction times)
What should be included in the exercise process
warm up/cool down
functional activities
circuit training
strength training with focus on spinal alignment
isometric recommendations for strengthening
near max effort
6-10 sec holds
5-10 reps
10 sec rest
3xday, 5 weeks max
isotonic recommendations for strengthening
determine 1RM
exercise 60-800% 1RM
3 sets of 8-10 reps
1-2 min rest
3xweek, 8 weeks min
What can lead to flexibility impairments
decrease in elastin and collagen
tendons and ligs become more rigid
less responsive to length changes
hypokinesis
flexibility interventions
slow, prolonged stretching
maintain/gain functional range
encourage frequent activity
How often should a pt change stretching positions
every 15-20 mins
Pain considerations
rate pain
point to exance location of pain
Effective pain management techniques
TENS
visual imagery (go to your place/where do you wanna get back to)
relaxation
coordination with MD for medications
Pain education
purpose of pain mgmt
scheduling in consideration of therapy sessions (timing of dose)
important of communicating with healthcare team about pain
importance of activity in pain mgmt
NIH definition of osteoporosis
a systemic, skeletal disease characterized by low bone mass and micro architectural deterioration of bone tissue, with constant increase in bone fragility and susceptibility to fracture
What test is taken to determine osteoporosis
BMD or DEXA
WHO definition of osteopenia
BMD between 1 and 2.5 SDs below adult peak mean without evidence of fractures
WHO definition of osteoporpsis
BMD at least 2.5 SDs below adult peak mean without evidence of fractures
WHO definition of severe osteoporosis
BMD more than 2.5 SDs below adult peak mean with history of 1 or more fractures
Compare men and women bone density levels
men’s are always higher and have greater increase in 20s
women drop drastically with menopause
men progressively decrease
risk factors for osteoporosis
sex
age
race
family history
tobacco
lifetime exposure to estrogen
meds
calcium deficiency
sedentary lifestyle
alcoholism
depression
Medication treatments for osteoporosis
Hormone replacement therapy (estrogen)
selective estrogen receptor modulators
biphosphonates
calcitonin
What is calcitonin
hormone that regulates bone metabolism
What are the effects of calcitonin
reduced bone resorption and may slow bone loss
What are the effects of biphosphonates (Fosamax; Didronel; Actonel)
inhibit bone breakdown/bind permanently to to bone surfaces
limit osteoblast activity
What is selective estrogen receptor modulators
synthetic drugs mimic estrogen’s beneficial effects on bone density
What are the effects of selective estrogen receptor modulators (Raloxifene)
block the effect of estrogen on breast and uterine tissue
What are the effects of hormone replacement therapy (estrogen)
side effects and increase the risk of breast / uterine cancer
Essential exercise for osteoporosis
postural alignment
high impact strengthening
WB exercises
How are extension exercises beneficial to osteoporosis
reduce the incident of spine fx reoccurrence
How are high impact exercises beneficial to osteoporosis
better at increasing BMD than low impact activities
stronger m=stronger bones
How are WB exercises beneficial to osteoporosis
retains more bone mineral than NWB
What are the effects of swimming on BMD
none
What are the effects of walking on BMD
protect against further loss
What are the effects of weight training on BMD
increase
What are the effects of running on BMD
increase
What occurs when spinal compression fxs arise from osteoporosis
pain management
safe transitional movements
orthosis
What are the orthoses typically used for spinal compression fxs due to osteoporosis
lumbosacral corset, jewett brace
What are the common fx associated with osteoporosis
hip and vertebral bodies
When would semirigid braces be used when spinal conpression fxs are present
when the spinal canal is involved
What is a Kyphoplasty
a balloon catheter is inserted into a thoracic vertebral body, then filled with cement to regain normal size
What is a vertebroplasty
a balloon catheter is inserted into a lumbar vertebral body, then filled with cement to regain normal size
What is the point of a kyphoplasty/vertebroplasty
help relieve pain
PT interventions in the acute phase following a compression fx
pain mgmt with modalities
bedrest (possibly)
TherEx
PT interventions in the sub-acute phase following a compression fx
walking program
TherEx
What TherEx treatments are focused on in the acute phase following a compression fx
addressing postural awareness
What TherEx treatments are focused on in the Sub- acute phase following a compression fx
strengthen abs/back ext/scapular retractors
What type of activity do we want to avoid during the Sub-acute phase following a compression fx
lifting >10 lbs
flexion
precautions to PT interventions post compression fx
MD guidelines
Exercise tolerance
What is the activity pyramid for people over 60
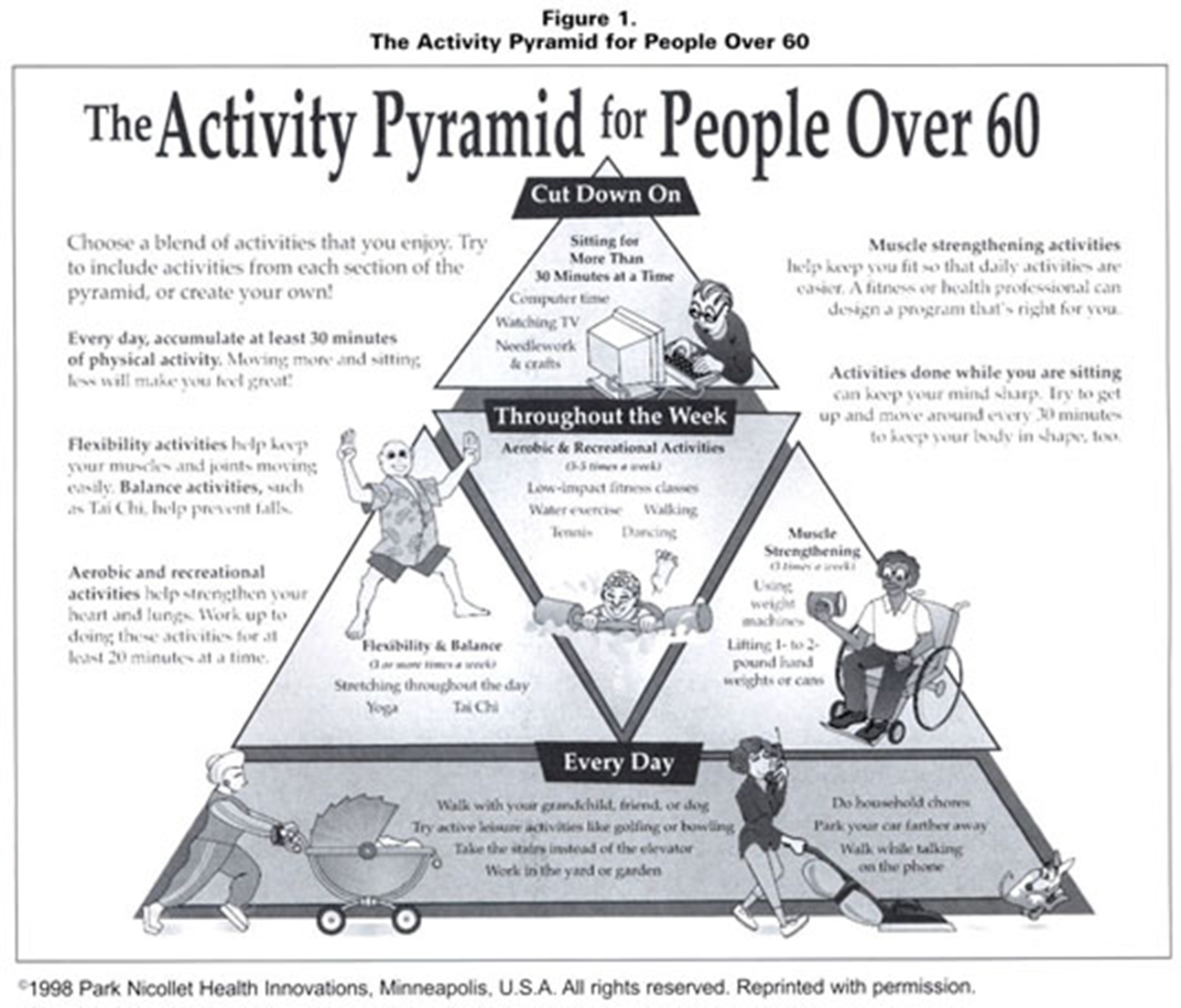
What are the key education points to give elderly pts
sit as little as possible
2-3xwk, do yard/house work and strengthening
3-5xwk do aerobic activity and swim/golf/tennis
every day, walk more at home/take stairs/park further from store