Chapter 17: Neurocognitive Disorders (Week 8)
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
Chapter 17: Neurocognitive Disorders
Group of conditions with disruption in:
Thinking
Memory
Processing
Problem-solving
Treatment requires compassionate understanding of both the client and their family.
Types of Cognitive Disorders (DSM-5-TR)
Delirium (short-term, reversible)
Mild Neurocognitive Disorder (may or may not progress)
Major Neurocognitive Disorder (Dementia) (progressive, irreversible)
Subtypes of Major & Mild NCD:
Alzheimer’s Disease (AD): most common, neurodegenerative, gradual impairment of cognitive function
Parkinson’s disease
Huntington’s disease
Key Point
Must distinguish NCD from other mental health disorders.
Example: Depression in older adults can mimic early Alzheimer’s.
Frequently forgetting small things (MD appt? meds taken? car parked where?).
Safety concerns: med adherence, getting lost, driving/parking.
Mild Dementia
Recognition issues (“Have we met?” “I’m lost; need to get home.” “Are you sure I own a car?”).
Safety concerns: wandering, elopement, financial/vulnerability risks.
Moderate Dementia
May forget how to talk, walk, swallow, or even breathe.
Safety concerns: aspiration, immobility, respiratory compromise, total care needs.
Severe Dementia
Restless, babbling, agitation
Games, puzzles, coloring
NO television (too much stimuli)
Hyperactive Delirium
Slow, sleepy, low energy.
Hypoactive Delirium
Delirium vs Dementia Types
Hyperactive: restless, babbling, agitation
Games, puzzles, coloring
NO television (too much stimuli)
Hypoactive: slow, sleepy, low energy.
Mixed
Unclassified
Mild: frequently forgetting small things (MD appt? meds taken? car parked where?).
Safety concerns: med adherence, getting lost, driving/parking.
Moderate: recognition issues (“Have we met?” “I’m lost; need to get home.” “Are you sure I own a car?”).
Safety concerns: wandering, elopement, financial/vulnerability risks.
Severe: may forget how to talk, walk, swallow, or even breathe.
Safety concerns: aspiration, immobility, respiratory compromise, total care needs.
loss of memory
amnesia
loss of skilled movements/gestures DESPITE motor function/intent
apraxia
loss of people/object identification
agnosia
loss of language/swallow
aphasia
Delirium Meds: AFTER ADDRESSING underlying DELERIUM causes
Anxiolytics (e.g., benzos)
Antipsychotics
“4 A’s” of Dementia (Alzheimer’s)
Amnesia: loss of memory
Apraxia: loss of ability to execute skilled movements/gestures despite intact motor function and intent
Agnosia: loss of ability to identify people/objects
Aphasia: slide lists “Loss of ability to swallow” (note: classically aphasia = language impairment; the slide’s phrasing emphasizes functional decline including swallowing problems in severe stages).
Previously anosmia (no longer diagnostic due to covid)
Cognitive Disorders Risk Factors
Delirium:
Physiological changes:
Neurologic (Parkinson’s, Huntington’s)
Metabolic (hepatic/renal failure, fluid & electrolyte imbalance, nutritional deficiencies)
Cardiovascular/respiratory disease
Infections (HIV/AIDS)
Surgery
Substance use/withdrawal
Other:
Older age
Multiple comorbidities
Severe illness, polypharmacy
ICU stays, surgery, aphasia, restraint use, change in environment
Neurocognitive Disorder & Alzheimer’s Disease (AD):
Advanced age
Prior head trauma
Cardiovascular disease
Lifestyle factors
Family history of AD (strong genetic link in early-onset familial AD)
Delirium (8) vs NCD/AD (4) Risk Factors
Neurologic (Parkinson’s, Huntington’s)
Metabolic (hepatic/renal failure, fluid & electrolyte imbalance, nutritional deficiencies)
Infections (HIV/AIDS)
Substance use/withdrawal
ICU stays, surgery, aphasia, restraint use, change in environment
Severe illness
Polypharmacy
Mostly males
Prior head trauma
Lifestyle factors
Family history
Mostly females
Neurologic (Parkinson’s, Huntington’s)
Metabolic (hepatic/renal failure, fluid & electrolyte imbalance, nutritional deficiencies)
Infections (HIV/AIDS)
Substance use/withdrawal
ICU stays, surgery, aphasia, restraint use, change in environment
Severe illness
Polypharmacy
Mostly males
Advanced age
Cardiovascular/respiratory disease
Delirium Risk Factors
Prior head trauma
Lifestyle factors
Family history
Mostly females
Advanced age
Cardiovascular/respiratory disease
NCD/AD Risk Factors
Delirium & NCD/AD Risk Factors
Advanced age
Cardiovascular/respiratory disease
Delirium Risk Factors: PINCH ME
Poorly controlled pain
Infections (e.g., UTI)
Nutrition issues (poor diet, vitamin deficiency)
No cooking skills
Constipation (under-recognized trigger)
Hydration (dehydration)
Medications (prescribed or illicit)
Endocrine (diabetes, thyroid disorder).
Cognitive Disorders Expected Findings
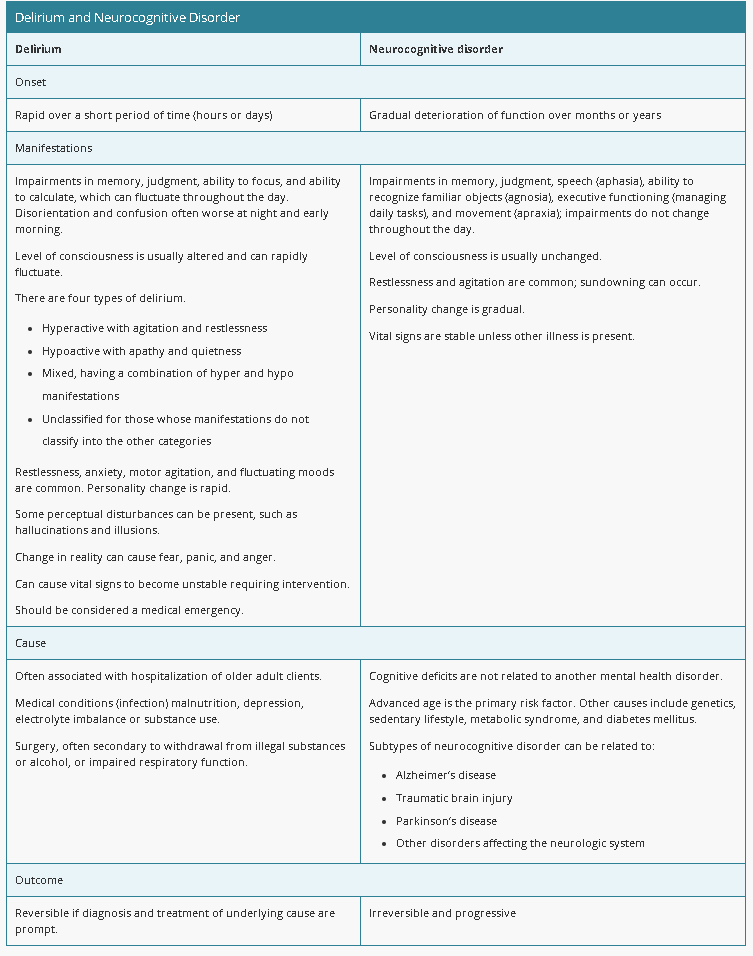
Delirium & NCD share similarities but differ in onset/course.
Clients with NCD may also develop delirium.
Delirium vs NCD/AD Findings
Rapid (hours–days)
LOC can rapidly fluctuate (SUNDOWNING)
Morning - Coherent
Noon-Night - Confused
4 Types (hyper = restless, hypo = quiet, mixed, unclassified)
Rapid personality change
Unstable vital signs
May involve perceptual disturbances
Reversible if diagnosis/treatment prompt
Medical emergency
Gradual deterioration (months–years)
LOC usually unchanged or gradual
3 Days - Coherent
4 Days - Confused
Gradual personality change
Stable vital signs
Common: Restlessness, agitation, sundowning
Irreversible and progressive
Gradual deterioration (months–years)
LOC usually unchanged or gradual
3 Days - Coherent
4 Days - Confused
Gradual personality change
Stable vital signs
Common: Restlessness, agitation, sundowning
Irreversible and progressive
NCD/AD Findings
Rapid (hours–days)
LOC can rapidly fluctuate (SUNDOWNING)
Morning - Coherent
Noon-Night - Confused
4 Types (hyper = restless, hypo = quiet, mixed, unclassified)
Rapid personality change
Unstable vital signs
May involve perceptual disturbances
Reversible if diagnosis/treatment prompt
Medical emergency
Delirium Findings
Fluctuating Course
More coherent in the morning, confusion/hallucinations in afternoon (“sundowning”)
Can help differentiate from dementia’s more consistent/enduring confusion.
Delirium - Think fast turnaround, clear during day, confused at night
Dementia (NCD) - Think slow turnaround, 3 days of clarity, 4 days of confusion
Cognitive Disorders Defense Mechanisms
Denial: Client/family refuse to believe memory loss is happening, even when obvious.
Confabulation: Client makes up stories about events they don’t remember (unconscious attempt to protect self-esteem, not intentional lying).
Perseveration: Client repeats phrases/behaviors instead of answering questions (protects self-esteem when memory fails).
Cognitive Disorders Diagnostic Procedures
No specific test → definitive diagnosis only at autopsy
Testing done to rule out other pathologies:
Chest/head x-rays
EEG (electroencephalography)
ECG (electrocardiography)
Liver function studies
Thyroid function tests
Neuroimaging (CT, PET)
Urinalysis
Blood electrolytes
Folate & vitamin B12 levels
Vision & hearing tests
Lumbar puncture
Cognitive Disorders Screening & Assessment Tools
For Delirium
Confusion Assessment Method (CAM)
Neelon-Champagne (NEECHAM) Confusion Scale
For Dementia/Neurocognitive Disorders
Functional Dementia Scale (self-care, memory loss, mood, danger to self/others)
Brief Interview for Mental Status (BIMS) – long-term care settings
Mini-Mental Status Examination (MMSE)
Functional Assessment Screening Tool (FAST)
Global Deterioration Scale
Blessed Dementia Scale (uses info from family/secondary source)
A nurse is performing an admission assessment for a client who has delirium related to an acute urinary tract infection. Which of the following findings should the nurse expect?
Select all that apply.
a
History of gradual memory loss
b
Family report of personality changes
c
Hallucinations
d
Unaltered level of consciousness
e
Restlessness
b Family report of personality changes
c Hallucinations
e Restlessness
The client who has delirium can experience memory loss with sudden rather than gradual onset.
The client who has delirium is expected to have an altered level of consciousness that can rapidly fluctuate.
Cognitive Disorders Nursing Care
Prevention/management: minimize risk factors, promote early detection (timely recognition = essential).
Nurse self-awareness: manage frustration, anger, or fear when caring for progressive decline.
Focus: protect from injury while promoting dignity and quality of life.
Safe/Therapeutic Environment
Assess risk for falls/wandering.
Place client near nurses’ station.
Provide low-level visual/auditory stimuli.
Well-lit environment, minimize contrasts/shadows.
Room with windows for time orientation.
Identification bracelet; use monitors/bed alarms PRN.
Restraints = last resort.
Cautious PRN meds for agitation/anxiety.
Lower bed, assess risk for injury.
Cognitive Support
Use memory aids: clocks, calendars, photos, memorabilia, familiar objects.
Reorient as needed.
Maintain consistent routine and caregivers.
Remove mirrors (reduce fear/agitation).
Encourage daily physical activity.
Ensure bathroom has adequate lighting at night.
Physical Needs
Monitor neurologic status.
Identify physiologic disturbances contributing to delirium.
Assess skin integrity (risk: poor nutrition, immobility, incontinence).
Monitor vital signs (tachycardia, BP changes, diaphoresis, dilated pupils may indicate delirium).
Promote sleep and comfort (nonverbal indicators matter).
Provide eyeglasses/hearing aids if needed.
Ensure food/fluid intake.
Monitor lab results (electrolyte imbalances can cause delirium).
Communication
Calm, reassuring tone.
Positive phrasing (do not argue or question hallucinations/delusions).
Reinforce reality, orientation to time/place/person.
Introduce self with each contact.
Eye contact; short, simple sentences; one item of info at a time.
Encourage reminiscing about happy/familiar events.
Break instructions into short segments.
Limit choices when dressing/eating.
Reduce decision-making/abstract thinking demands (avoid frustration).
Avoid confrontation.
Approach slowly, from the front; use client’s name.
Encourage family visits as appropriate.
Delirium Medications (AA)
Use caution with PRN meds for agitation/anxiety
Always evaluate if medications are causing or worsening
Medications may be underlying cause → monitor for reactions.
Management:
Treat underlying disorder.
Antipsychotics or antianxiety meds may be prescribed.
Cholinesterase Inhibitors Actions / Use
Inhibits acetylcholine breakdown → Increases acetylcholine
Improves memory, thinking, learning
Slows cognitive decline
Mild to moderate Alzheimer’s disease (AD).
Cholinesterase Inhibitors Complications / Contraindications
GI: Nausea, vomiting, diarrhea → monitor closely, promote adequate fluid intake, titrate dose.
Bradycardia, syncope → orthostatic hypotension
Teach family to monitor pulse at home.
Screen for underlying heart disease.
Bronchoconstriction
Contraindication: GI Bleeding
Use cautiously with: Asthma, obstructive pulmonary disorders (bronchoconstriction risk)
the NVD uses CHOLesky factorization to prevent SYNCOPE/FAINTING in ASTHMA patients with SLOW HEART and PULMONARY prosthetics
the NVD uses CHOLesky factorization to prevent SYNCOPE/FAINTING in ASTHMA patients with SLOW HEART and PULMONARY prosthetics
Cholinesterase Inhibitors Complications / Contraindications
GI: Nausea, vomiting, diarrhea → monitor closely, promote adequate fluid intake, titrate dose.
Bradycardia, syncope → orthostatic hypotension
Teach family to monitor pulse at home.
Screen for underlying heart disease.
Bronchoconstriction
Contraindication: GI Bleeding
Use cautiously with: Asthma, obstructive pulmonary disorders (bronchoconstriction risk)
Cholinesterase Inhibitors Interactions / Admin
NSAIDs (e.g., aspirin): ↑ GI bleeding risk → monitor NSAID use and GI symptoms.
Antihistamines, tricyclic antidepressants, conventional antipsychotics, anticholinergics: ↓ therapeutic effects
Start low dose → gradually increase until therapeutic or adverse effects appear.
Educate client/family about adverse effects.
Taper medication when discontinuing to avoid rapid progression.
Monitor swallowing ability (available in tablets, oral solutions, orally disintegrating tablet for donepezil).
Administration:
Donepezil: once daily at bedtime (long half-life).
Others: usually twice daily.
Rivastigmine: oral form or patch (apply daily; take with food to ↓ GI upset).
Cholinesterase Inhibitors Meds: she DONNED an indian iron CHOLI from the RIVer GALA MINE
Donepezil
Rivastigmine
Galantamine
When should Donepezil be taken?
At night due to long half-life
N-methyl-D-aspartate (NMDA)
An excitatory glutamate receptor
Requires glutamate binding and calcium ion charges
Involved in learning, memory, and other vital functions.
Overactivation of receptors can lead to cell damage and is linked to neurological disorders, particularly in Alzheimer’s patients.
NMDA Receptor Antagonist Action / Use
Blocks calcium entry and glutamate activation into nerve cells
Slows brain-cell death (neuroprotection)
Moderate to severe Alzheimer’s disease (AD).
Mild to moderate vascular dementia
NMDA Receptor Antagonist Complications / Contraindications
Dizziness, headache, confusion, constipation.
Pregnancy/breastfeeding, epilepsy/seizure disorder, severe hepatic/renal impairment.
Main Contraindication: Renal failure
CONSTIPATED CHADs NEVER MAKE DUMPS AVAILABLE due to KIDNEY FAILURE
CONSTIPATED CHADs NEVER MAKE DUMPS AVAILABLE due to KIDNEY FAILURE
NMDA Receptor Antagonist Complications
Dizziness, headache, confusion, constipation.
Pregnancy/breastfeeding, epilepsy/seizure disorder, severe hepatic/renal impairment.
Main Contraindication: Renal failure
NMDA Receptor Antagonist Interactions / Admin
May be used with a cholinesterase inhibitor.
Give with or without food.
Report any worsening confusion, dizziness, or headache to the provider.
Encourage safe ambulation if dizziness occurs, and assess for changes in bowel habits
Antacids and other drugs that increase urine pH can elevate drug levels, increasing toxicity risk.
NMDA Receptor Antagonist Meds: MASTURBATION (euphemism) does not clear my bowels when I can NEVER MAKE DUMPS AVAILABLE
Memantime
MASTURBATION (euphemism) does not clear my bowels when I can NEVER MAKE DUMPS AVAILABLE
NMDA Receptor Antagonist Meds
Memantime
NCD/AD Medications: SRA members with DEMENTIA need a CNA for gun control
Cholinesterase Inhibitors
Examples: Donepezil, Rivastigmine, Galantamine
Action: ↑ acetylcholine by inhibiting breakdown → improves self-care ability, slows cognitive decline in mild–moderate Alzheimer’s.
Adverse Effects
GI: Nausea, vomiting, diarrhea → monitor closely, promote adequate fluid intake, titrate dose.
Bradycardia, syncope → teach family to monitor pulse at home.
Screen for underlying heart disease.
Contraindications/Precautions
Use cautiously with:
Asthma, obstructive pulmonary disorders (bronchoconstriction risk).
Interactions
NSAIDs (e.g., aspirin): ↑ GI bleeding risk → monitor NSAID use and GI symptoms.
Antihistamines, tricyclic antidepressants, conventional antipsychotics: ↓ therapeutic effects of donepezil → avoid cholinergic-blocking drugs.
Nursing Administration
Start low dose → gradually increase until therapeutic or adverse effects appear.
Educate client/family about adverse effects.
Taper medication when discontinuing to avoid rapid progression.
Monitor swallowing ability (available in tablets, oral solutions, orally disintegrating tablet for donepezil).
Administration:
Donepezil: once daily at bedtime (long half-life).
Other cholinesterase inhibitors: usually twice daily.
Rivastigmine: oral form or patch (apply daily; take with food to ↓ GI upset).
NMDA Receptor Antagonist
Memantine
Blocks calcium entry into nerve cells → slows brain-cell death.
Approved for moderate to severe Alzheimer’s disease (AD).
Nursing Actions
May be used with a cholinesterase inhibitor.
Give with or without food.
Monitor adverse effects: dizziness, headache, confusion, constipation.
Other Medications
SSRIs: for depression.
Antianxiety meds: for agitation.
Antipsychotics: for hallucinations/delusions (last resort; many adverse effects).
SRA members with DEMENTIA need a CNA for gun control
NCD/AD Medications
SSRIs: for depression.
Antianxiety meds: for agitation.
Cholinesterase Inhibitors
NMDA Receptor Antagonist
Antipsychotics: for hallucinations/delusions (last resort; many adverse effects).
Cholinesterase Inhibitors
Examples: Donepezil, Rivastigmine, Galantamine
Action: ↑ acetylcholine by inhibiting breakdown → improves self-care ability, slows cognitive decline in mild–moderate Alzheimer’s.
Adverse Effects
GI: Nausea, vomiting, diarrhea → monitor closely, promote adequate fluid intake, titrate dose.
Bradycardia, syncope → teach family to monitor pulse at home.
Screen for underlying heart disease.
Contraindications/Precautions
Use cautiously with:
Asthma, obstructive pulmonary disorders (bronchoconstriction risk).
Interactions
NSAIDs (e.g., aspirin): ↑ GI bleeding risk → monitor NSAID use and GI symptoms.
Antihistamines, tricyclic antidepressants, conventional antipsychotics: ↓ therapeutic effects of donepezil → avoid cholinergic-blocking drugs.
Nursing Administration
Start low dose → gradually increase until therapeutic or adverse effects appear.
Educate client/family about adverse effects.
Taper medication when discontinuing to avoid rapid progression.
Monitor swallowing ability (available in tablets, oral solutions, orally disintegrating tablet for donepezil).
Administration:
Donepezil: once daily at bedtime (long half-life).
Other cholinesterase inhibitors: usually twice daily.
Rivastigmine: oral form or patch (apply daily; take with food to ↓ GI upset).
NMDA Receptor Antagonist
Memantine
Blocks calcium entry into nerve cells → slows brain-cell death.
Approved for moderate to severe Alzheimer’s disease (AD).
Nursing Actions
May be used with a cholinesterase inhibitor.
Give with or without food.
Monitor adverse effects: dizziness, headache, confusion, constipation.
A nurse is caring for a client who has early stage Alzheimer’s disease and a new prescription for donepezil. The nurse should include which of the following statements when teaching the client about the medication?
a
“You should avoid taking over-the-counter acetaminophen while on donepezil.”
b
“You should take this medication before going to bed at the end of the day.”
c
“You will be screened for underlying kidney disease prior to starting donepezil.”
d
“You will be screened for underlying kidney disease prior to starting donepezil.”
b “You should take this medication before going to bed at the end of the day.”
Donepezil should be taken at the end of the day or before bed due to tis long half-life
Tell the client to avoid NSAIDs, rather than acetaminophen, due to risk for gastrointestinal bleeding.
Clients should be screened for underlying heart and pulmonary disease, rather than kidney disease, prior to treatment.
Cognitive Disorders Alternative/Complementary Therapies
Alternative/Complementary Therapies
Some vitamins/herbals under investigation.
Currently no evidence they are effective.
Client Education Care After Discharge
Educate family/caregivers about illness, care methods, home adaptations.
Ensure safe home environment.
Key Questions to Ask
Will client wander if doors left unlocked?
Can client remember address and name?
Does client harm others when allowed to wander?
Home Safety Measures
Remove scatter rugs.
Door locks that are not easily opened.
Lock/tune water heater thermostat to safe level.
Good lighting, especially on stairs.
Install stair handrails, mark step edges with colored tape.
Place mattresses on floor (prevent falls).
Remove clutter, keep walkways clear.
Secure electrical cords.
Store cleaning supplies in locked cupboards.
Install grab bars in bathrooms.
Allow safe pacing/wandering.
Support for Caregivers
Encourage seeking legal counsel for advanced directives, guardianship, or durable power of attorney for health care.
Determine teaching needs of client & family as cognitive decline progresses.
Review available resources:
Long-term care options.
Home care/community resources (can help client remain at home vs. facility).
Provide support for caregivers:
Ask for help from friends/family.
Use respite care and support groups.
Encourage caregivers to practice self-care and take things one day at a time.
A nurse in a long-term care facility is caring for a client who has major neurocognitive disorder and attempts to wander out of the building. The client states, “I have to get home.” Which of the following statements should the nurse make?
a
“You have forgotten that this is your home.”
b
“You cannot go outside without a staff member.”
c
“Why would you want to leave? Aren’t you happy with your care?”
d
“I am your nurse. Let’s walk together to your room.”
d “I am your nurse. Let’s walk together to your room.”
When the nurse recognizes the client is attempting to wander out of the building, the nurse should introduce oneself with each new interaction and to promote reality in a calm, reassuring manner.
A home health nurse is making a visit to a client who has Alzheimer’s Disease to assess the home for safety. Which of the following suggestions should the nurse make to decrease the client’s risk for injury?
a
Install extra locks at the top of exit doors.
b
Place rugs over electrical cords.
c
Put cleaning supplies on the top of a shelf.
d
Place the client’s mattress on the floor.
e
Install light fixtures above stairs.
a Install extra locks at the top of exit doors.
d Place the client’s mattress on the floor.
e Install light fixtures above stairs.
When taking action, the nurse should suggest the following to decrease the client’s risk for injury in the home placing door locks up high where they are difficult to reach can prevent exiting the home and wandering outside, placing the client’s mattress on the floor to reduce the risk for falls out of the bed Instruct the family to ensure there is adequate lighting around the stairs to reduce the risk for falls.
Cleaning supplies should be placed in locked cupboards. Marking the supplies with colored tape does not prevent the client’s access to hazardous materials.
A nurse is making a home visit to a client who is in the late stage of Alzheimer’s Disease. The client’s partner, who is the primary caregiver, wishes to discuss concerns about the client’s nutrition and the stress of providing care. Which of the following actions should the nurse take?
a
Verify that a current power of attorney document is on file.
b
Instruct the client’s partner to offer finger foods to increase oral intake.
c
Provide information on resources for respite care.
d
Schedule the client for placement of an enteral feeding tube.
c Provide information on resources for respite care.