Restrictive Lung Disease and Respiratory Failure and Mechanical Ventilation
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
What are potential extrinsic causes of restrictive lung disease? Intrinsic?
- Extrinsic Causes (outside of the lungs that effect breathing)
o Pectus deformities
o Kyphoscoliosis
o Ascites/PE
o Neuromuscular disorders
o Obesity
- Interstitial
o Idiopathic pulmonary fibrosis (unknown cause)
o Pneumoconiosis: related to exposure
o Sarcoidosis (immune)
PFT and Testing Results, Pathophys (of both types)
About restrictive disease: less common, have decreased lung expansion
PFTs:
- Reduced FVC and TLC
- Normal to higher FEV1/FVC ratio (because they reduce proportionately) restrictive on PFTs, do DLCO
- DLCO testing:
o Low DLCO (low exchange): interstitial lung disease
o Normal DLCO: extrinsic restrictive disease
Pathophysiology
- Decreased compliance (stretch/expansion) due to rigid lungs
- Extrinsic: altered mechanical function (hypoventilation)
- Interstitial: inflammation of pulmonary parenchyma (alveoli/ gas exchange tissues) leading to deposition of collagen and subsequent fibrosisthickened alveolar septate physical barrier to gas exchange
o Not well perfused areas/ or we perfuse where we cannot exchange well
o Fibrosis decreases lung compliance, reducing inspiratory capacity (the air you can get in)
Obesity Hypoventilation Syndrome
- : awake hypoventilation in an obese individual
o Clinical presentation: obsese pt w/ findings of OSA
§ Loud snoring
§ Daytime hypersomnolence (sleepiness)
§ Fatigue
§ Choking
§ Small oropharynx or a thick neck
o Dx criteria:
§ Clinical presentation
§ BMI over 30 (likely over 45, morbidly obese patients)
§ Pa of CO2 over 45mmHg
§ OSA
§ Exclusion of other causes of alveolar hypoventilation
o Tx:
§ CPAP/BIPAP
§ Wt loss
§ Tracheostomy, palliative care (end stage)
§ Avoid sedatives, alcohol, opioids
o OHS complications: cor pulmonale, hypercapnia/hypoxemia mixed respiratory failure, polycythemia (excess RBCs due to hypoxemia)
Chest Wall Deformities
- scoliosis, kyphosis, pectus deformities
o Diagnostic criteria: clinical exam or imaging, restrictive on spirometry-decreased FVC with normal dlco, reduced FVC
§ Kyphosis: excessive curvature of thoracic spine, head tilted forward (k shape)
§ Scoliosis abnormal curvature in the coronal plane (S shape)
· Reduced chest wall compliance, work of breathing, may experience exertional dyspnea
· Treatment braces or surgery, not everyone needs treatment, or has their breathing affected by this
o Pectus deformities: could have underlying heart, neuro disease!
§ Pectus excavatum: chest wall grows abnormally inward
§ Pectus carinatum is when the chest wall grows abnormally outwards
- Treatment: surgery, braces, PT, must time based on growth plate closure
Define parenchyma, interstitium, pneumonitits, pneumoconiosis
Parenchyma: functional elements, site of gas exchange, alveoli
Interstitium: supportive tissue/everything else in the lungs that doesn't do gas exchange (framework)
Pneumonitis: inflammation of alveolar walls, pneumonia is a type of pneumonitis (and may often look like pneumonia)
Pneumoconiosis: any chronic lung disease caused by inhalation of mineral dust, has inflammation and fibrosis
What is ILS? What is effected? Pathophys?
About ILS: more common in elderly, frequently misdiagnosed, can often not locate the cause of disease
- Interstitium is affected, not the parenchyma, damage through the interstitium leads to VQ mismatch and hypoxemia
o Most are associated with alveolar and airway alterations (diffuse parenchymal lung disease)
- Low DLCO due to scarring/fibrosis and thickening between alveoli
Pathophysiology: Triggers a non infectious inflammatory immune response that over time will lead to fibrosis and scarring
Sx and Physical Exam: Interstitial Lung Disease
Sx: shortness of breath, dry cough, fatigue-- symptoms are usually progressive and slow to develop (duration and progression of symptoms gives you a clue as to etiology)
Physical exam: crackles, clubbing, rarely wheezing, signs of rheumatologic disease (rash)
- Spirometry will show restrictive, can be normal or mixed
- DLCO: should be low
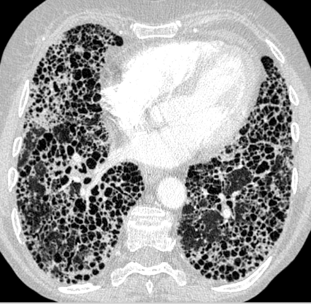
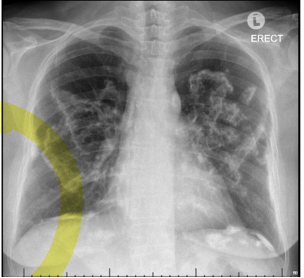
ILS: Lung Disease Imaging and Diagnosis
- Chest X-ray often indistinct can look like a lot of different things, could look like pneumonia, different types of infiltrates could also be normal
- High resolution CT scan: this is the best way to detect ild: will see a reticular pattern, opacities, and honeycombing
Pneumoconiosis
Pneumoconiosis: occupational lung disease due to prolonged exposure to inhaled mineral dust
- Sx: Ranges from asymptomatic to dyspnea crackles clubbing and cyanosis, may often see progressive dyspnea or a nonproductive cough
- Diagnosis: based on exposure history, PFT's and CT findings
- treatment: supportive, smoking cessation, oxygen therapy as needed
- If you work up high, disease is down low in lungs… if you work down low, disease is up high in lungs
Asbestosis
a. Of work in old buildings or ships (like up high in an old building) 10+ YEARS
b. Physical exam: crackles
c. Imaging: chest X-ray showing thickened pleura, calcified plaque on diaphragms or lateral chest wall, may have holly leaf sign (looks like beef in the lung)
d. Located in lower lungs
e. Smoking plus asbestosis causes a very high risk of lung cancer then either by itself (consider mesothelioma)
f. Treatment remove exposure, oxygen
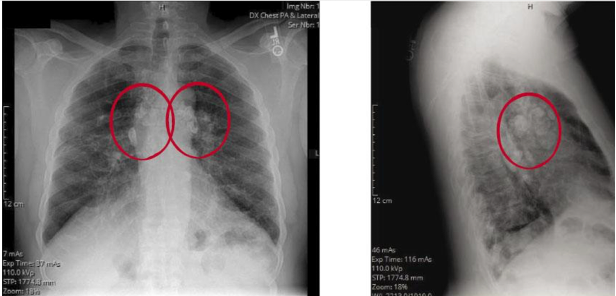
Silicosis
1. Silicosis: the most common occupation related disease in the world
a. Presentation/history: stonecutter sandblasting ceramics, granite PROLONGED EXPOSURE... Persistent dry cough (work DOWN LOW)
b. PE: cough, crackles in upper lobes
c. Dx: CXR small rounded opacities bilaterally and calcified hilar lymphadenopathy bilaterally (eggshell calcification) UPPER LOBES
d. Tx: acutely steroids, chronic: lung transplant
e. Increased risk for TB
Berylliosis
1. erylliosis: high tech electronics, aerospace can result w/ MINIMAL EXPOSURE, DOWN LOW
a. Sx: dry cough, fatigue, SOB
b. Bilateral crackles
c. Diagnosis: CXR infiltrates on UL, hilar adenopathy UPPER LOBES
d. Tx: steroids are highly effective, second line would be methotrexate
Coal workers
black lung
mine workers, in upper lobes of lungs, NO hilar involvement, no increased TB risk – presents after prolonged exposure
Byssinosis
a. Caused by inhalation of organic dust (cotton, flax, hemp dust)
b. Inflammation of the lung, no immune mediation (dust directly damages lungs)
c. Heals well w/ removed exposure (“Monday fever”)
Pneumonitis (alveolar wall inflammation)- 3 types
- Hypersensitivity pneumonitis
o Immune mediated
o Caused by moldy hay, pet birds (farmer’s lung or bird fancier lungs)
o Range of onset
o Consider w/ recurrent pneumonia w/ this type of exposure (clinical DX)
o Remove cause to treat
- Radiation pneumonitis: occurs after radiation, often has sharp delineation
o Early (1-3 months post rad): reversible
o Late (6-12 months post rad): permanent
- Medication-Induced Pneumonitis: nitrofurantoin/Macrobid, amiodarone, chemo, immunosuppressants
Systemic disease-ILD, vasculitis (GPA/EGPA)
Granulomatosis Polyangiitis (GPA) | SAME | Eosinophilic Granulomatosis Polyangiitis (EGPA) |
Older adults, Caucasians Sx: sinusitis, dypsnea, cough, fever, malaise Dx: confirm w/ lung biopsy, granulomatosis w/ polyangiitis Treat w/ steroids or immunosuppression-good recovery, untreated dead in 5 months | Necrotizing Vasculitis: small- medium vessels in lungs effected
ANCA +
Biopsy
| Eosinophilia (blood and tissue biopsy) Sx: does not effect sinuses Found in young people (20-50) Treat w/ steroids |
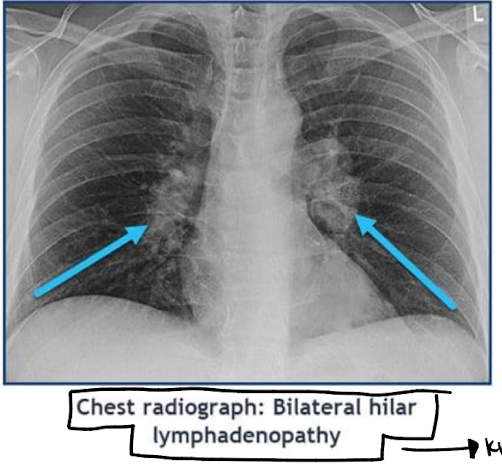
Sarcoidosis Triads
o Heerfordt syndrome: fever, uveitis (uvea of eye), parotitis
o Lofgren syndrome: erythema nodosum, bilateral hilar adenopathy, febrile polyarthralgia’s (joint pain plus fever)
Sarcoidosis: epi, findings
Epidemiology: found in young, African American women
- Disordered immune regulation, chronic, inflammatory, multisystem disease (lungs, skin, eyes)
o Can be asymptomatic
- Findings:
o Bilateral hilar adenopathy (CLASSIC FINDING)
o NON-CASEATING GRANULOMAS (no central necrosis-DIFFERENT FROM TB)
o Lupus pernio (if they have this, they have sarcoidosis): violaceous color on face d/ t granuloma deposition
o Parotitis
o Erythema nodosuom (looks like shin bruising)
Diagnosis and treatment of sarcoidosis
o Labs: elevated ACE (watch for HTN), elevated calcium (calcitriol prod)
§ Both made by granulomas
o Lung biopsy: noncaseating granuloma
o Imaging: bilateral hilar adenopathy
- Tx:
o 75% of people recover without treatment, with treatment we use methotrexate first line over steroids (can use steroids though)- normally opposite
Serial PFTs to see progression and guide, pulmonary fibrosis may cause death - KNOW CXR
General idiopathic interstitial pneumonia
- Can manifest as a nuber of diseases w/ unique features
- CXR will be non-specific, may show fibrosis
- High-resolution CT scan will show honeycombing
- PFTs w/ restrictive pattern, normal to increased FEV1/FVC ratio
- Biopsy, VATS
Idiopathic Pulmonary Fibrosis (specific type of idipathic)
- Most common form
- Risk: male, smoking, wood/metal exposure, post viral, diabetes, gerd
- Slow Set of dyspnea on exertion and a dry cough (over more than six months)
- Dx: dry/Velcro crackles clubbing present in advanced disease
- Honeycombing on CT scan
- Treatment: refer to pulmonology, mainstay of medical therapy is perfenidone or nintedanib (immunosuppressants)
o Supportive care
o Clinical trials
o Lung transplant evaluation if severe
- This is a diagnosis of exclusion because we do not know the cause
Respiratory failure: hypoxemia/hypercapnia, spectrum
Respiratory Failure:
- Can be due to a lung or non lung disorder
- Signs and symptoms will be correlated to underlying disease with hypoxemia or hypercapnia
o Hypoxemia may include cyanosis restlessness confusion anxiety delirium tachypnea bradycardia or tachycardia or hypotension
o Signs of hypercapnia include hypertension tachycardia tachypnea papilledema
- Respiratory failure exists on a spectrum... you want to intubate when they are in respiratory failure or impending cardiopulmonary arrest... before they get to cardio pulmonary arrest
Pathophysiology (2 types) and very general treatment
: hypoventilation, V/Q mismatch, shunting, diffusion abnormality
- Acute hypoxemic respiratory failure
o Low O2/ inadequate oxygen
o Develops over minutes to hours (QUICK)
o pulmonary edema, pneumonia, hem will hemorrhage
- Acute hypercarbic (hypercapnic) respiratory failure
o Developed over days (takes longer)
o Related to drug overdose or obstructive pulmonary disease
- Can also be a combination of the two (mixed)
- Always keep a broad differential (For failure can be caused by any number of things)
- Treatment: in both cases you would give oxygen for treatment
Acute Respiratory Distress Syndrome (ARDS): what is it, timing, sx, pathophys, dx, tx
- Lung injury triggered by a systemic, dysregulated, inflammatory response with acute onset (48-72 hours after event) of respiratory insufficiency with hypoxia and bilateral infiltrates on radiograph
o Trigger/precipitating eventr MVA, sepsis, aspiration
- Etiology: increased permeability of alveolar/capillary membrane leading to pulmonary edema (lungs fill w/ fluid)
- Not cardiogenic!
- Sx:
o Rapid onset of dyspnea (12-72 hours post event)
o RED FROTHY SPUTUM
o Hypoxia that doesn’t respond to oxygen (need ventilation)
- Pathophysiology: 3 stages early exudative, fibroproliferative after 7-10 days, fibrotic (irreversible, obliteration of lung tissue)
- Dx: CXR w/ bilateral infiltrates and air bronchograms (alveoli full of fluid-white)
o Severity scoring w/ degree of hypoxemia
- Tx:
o Supportive
§ PEEP (ventilator setting)
§ Keep hypovolemic but maintain perfusion
§ Low tidal volumes so we do not blow out alveoli
§ ECMO (external oxygenation)
§ Treat underlying disease