Anatomy and Physiology Chapter 8: Heart and Blood Vessels
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
Arteries
Thick walled, transport blood away from the heart under high pressure
Capillaries
Exchange solutes and water with cells via interstitial fluid
Most surface area of any blood vessels, spread out so velocity of flow decreases
Veins
Thin walled, return blood to heart
More constricted a vein is, faster the flow
Only veins have valves
Layers of vessel walls
Endothelium: squamous epithelial cells, continuation of heart lining
Smooth muscle with elastic connective tissue
Collagen: anchors vessels to tissue
Aneurysm
Ballooning of artery wall
Arteriole
Smallest arteries, connect to capillaries
Lack of connective tissue and have a smaller smooth muscle layer
Precapillary sphincter
Smooth muscle that controls blood flow into capillaries
Vasolidation
Relaxation of vascular smooth muscle increases capillary flow
Vasoconstriction
Constriction of vascular smooth muscle, decreases flow into capillaries
Lymphatic system
System consisting of the blood and blood vessels, but not RBCs or plasma proteins
Picks up objects too large to diffuse in capillaries
Lymph is transported to veins near the heart, where it rejoins the blood
How does blood return to the heart?
Squeezing of skeletal muscles
Valves that permit only one-way blood flow
Respiratory pump from breathing pressure
Pericardium
Protects and anchors heart
Pericardial cavity
Film of fluid that reduces friction
Heart walls
Epicardium: thin layer of epithelial and connective tissue
Myocardium: thick layer of cardiac muscle, bulk of heart
Contracting part of heart
Endocardium: thin, endothelial layer resting on connective tissue
continuous with the endothelium
Components of the heart
Atria: top of heart
Ventricles: bottom of hear
Septum: separates left and right sides
Types of valves
Atrioventricular valves: prevent backflow between chambers
Semilunar valves: prevent backflow between ventricles and pulmonary arteries/veins
Heart circuits
Pulmonary circuit: carries deoxygenated blood from the heart to lungs
Systemic circuit: carries oxygenated blood to limbs
Coronary arteries
Leads to capillaries that supply blood to the heart
Cardiac cycle
Atrial systole: atria contract, filling ventricles
AV open, SV close
Ventricular systole: ventricles contract, blood moves to the pulmonary trunk and aorta
AV close, atria relax and fill with blood
Diastole: aorta and ventricles relax
AV and SV close
Cardiac conduction system
Cardiac cells that initiate/distribute electrical influences
Begins in sinoatrial node (right atrium), initiates heartbeat
The reaches the atrioventricular node, and then reaches the atrioventricular bundle that conducts impulses to the left and right ventricles
Extend into smaller Purkinje fibers that carry the impulse into the myocardium of ventricles
Blood pressue
Force exerted by blood against blood vessel walls,
Generated by heart pumping
Measured with a sphygomanometer, measures the efficiency of the cardiovascular system
Healthy blood pressure is 120/80
Systolic pressure
Pressure in arterial vessels
Happens during ventricular systole
Diastole pressure
Lowest pressure
Happens in ventricular diastole
Hypertension
High bloop pressure, increased strain on cardiovascular system
Isolated systolic hypertension: systolic pressure is high, diastolic pressure is normal
Hypotension
Low blood pressure, reduced oxygen to brain and other organs
Below 90 in the top BP number, below 60 in the bottom
Baroreceptors
Baroreceptors: regulate arterial blood pressure:
Increase in blood pressure stretches baroreceptors
Sensory neurons fire, sending signals to the cardiovascular center of the brain
Heart rate and force of contraction is lessened to reduce blood pressure
Angina
Narrowing of coronary arteries, insufficient heart circulation
Heart attack
death of heart tissue caused by poor oxygen supply
Heart failure
inefficiency and weak pumping of blood
Congestive: buildup of interstitial fluid
Embolism
Blockage of blood vessels
Can be pulmonary, cerebral, or cardiac
Stroke
Interruption in blood supply to the brain
Normal resting HR
Between 60 and 100 BPM
Below is bradycardia
Higher is tachycardia
Over 170 BPM is atrial fibrillation, risk of stroke
Cardiac output formula
Heart rate*stroke volume
Sympathetic nervous system effect on heart
High blood pressure and heart rate, uses epinephrine and norepinephrine
Parasympathetic nervous system effect on heart
Lower blood pressure and heart rate, uses acetylcholine
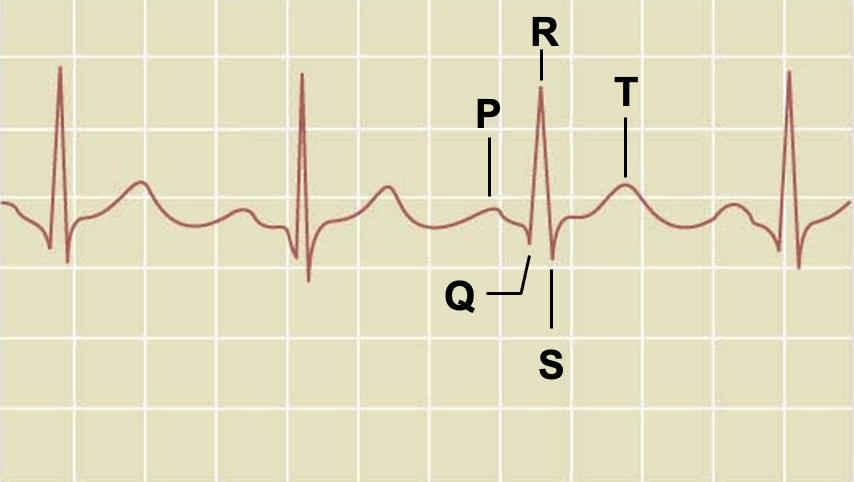
Label ECG
P wave: impulse across atria (Atrial contraction)
QRS complex: spread of impulse, including all the way down to Purkinje fibers, depolarization during ventricular contraction
5: ventricular relaxation, repolarization
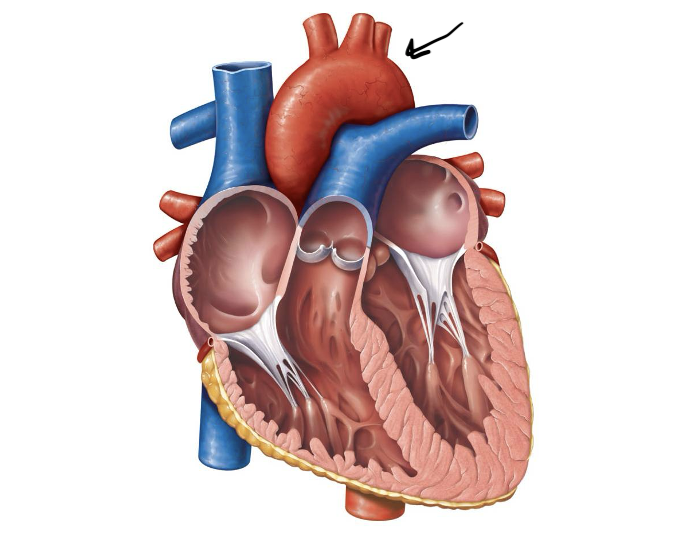
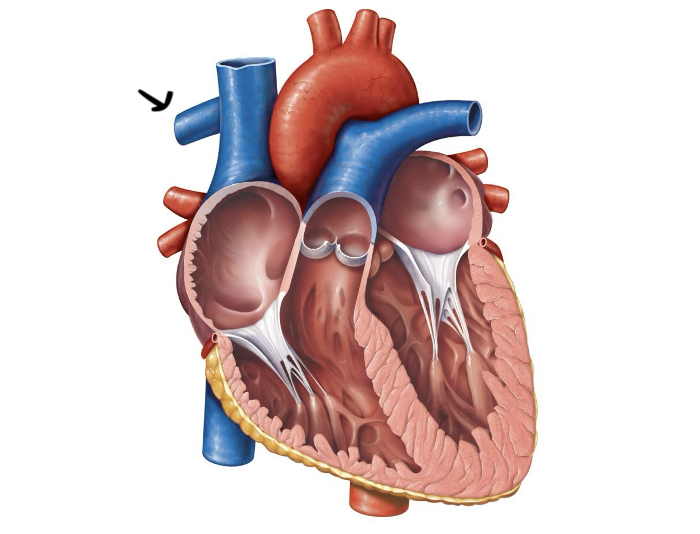
Label and function
Aorta, pumps blood to the rest of the body after leaving heart
Area where blood flows the fastest
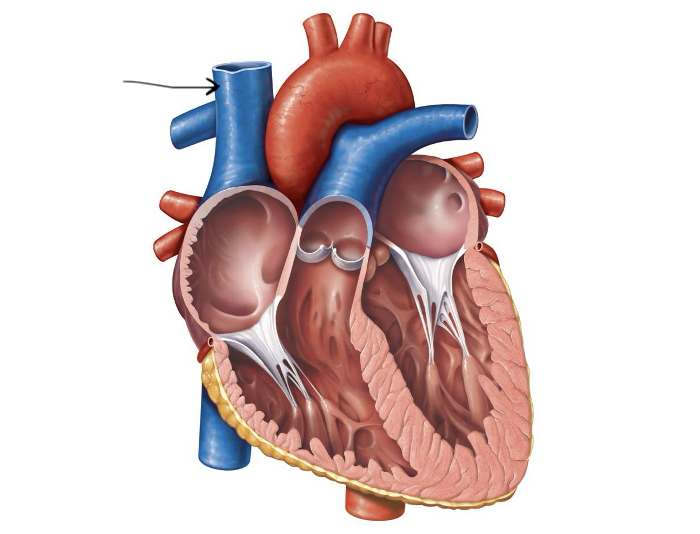
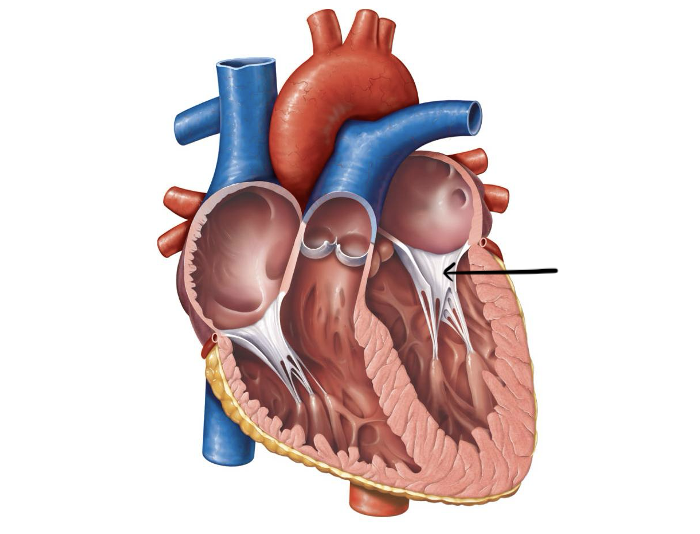
Label and function
Superior vena cava, brings in deoxygenated blood from above the heart
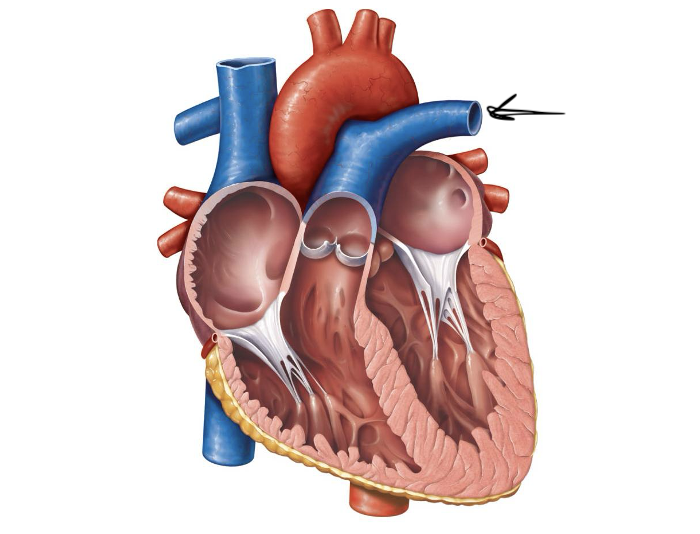
Label and function
Left pulmonary artery, sends deoxygenated blood to the left lung
Label and function
Right pulmonary artery, sends deoxygenated blood to the right lung
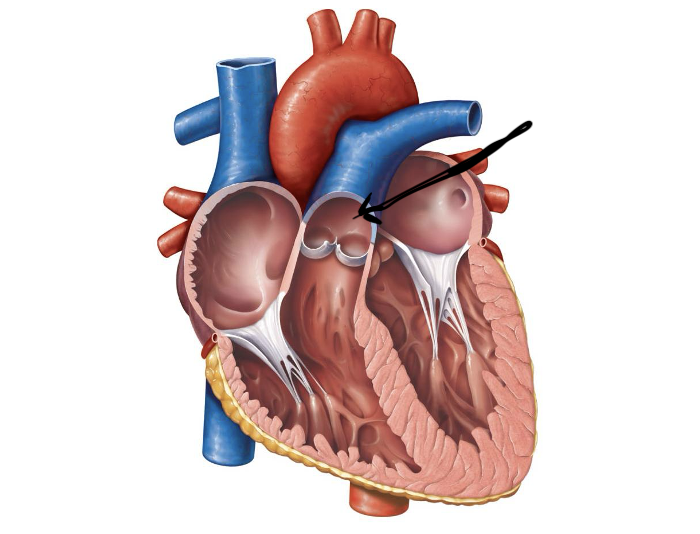
Label and function
Pulmonary trunk, branches into the pulmonary arteries
Label and function
Pulmonary veins, bring oxygenated blood back from the veins to the heart
Label and function
Left atrium, receives oxygenated blood and pumps it into the left atrium
Label and function
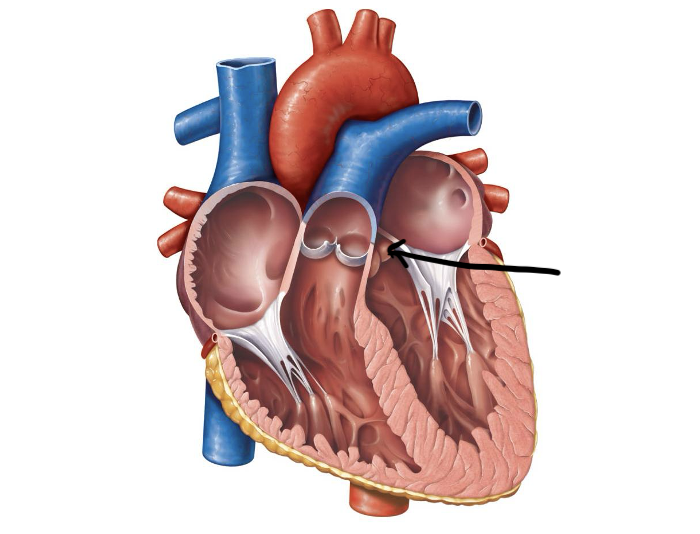
Aortic semilunar valve, prevents backflow from the aorta to the left ventricle
Label and function
Pulmonary semilunar valve, prevents backflow from the pulmonary artery into the left ventricle
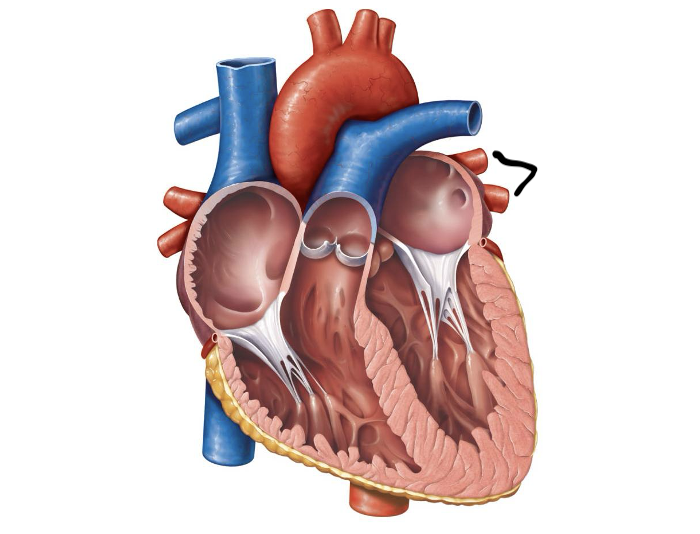
Label and function
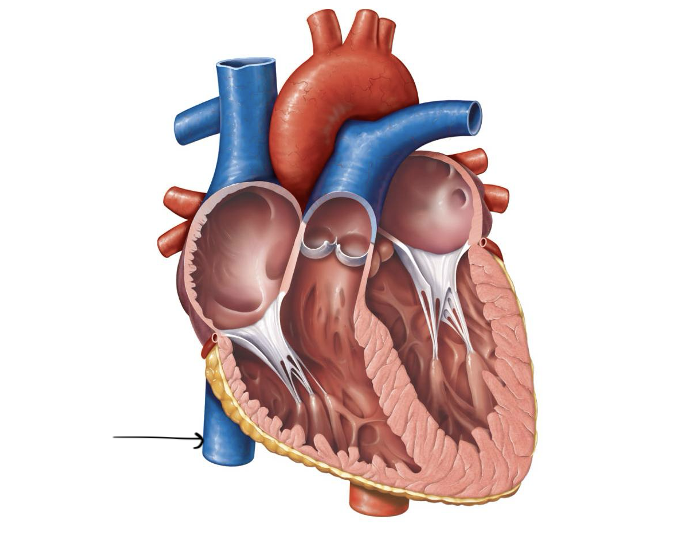
Inferior vena cava, brings in blood from below the heart
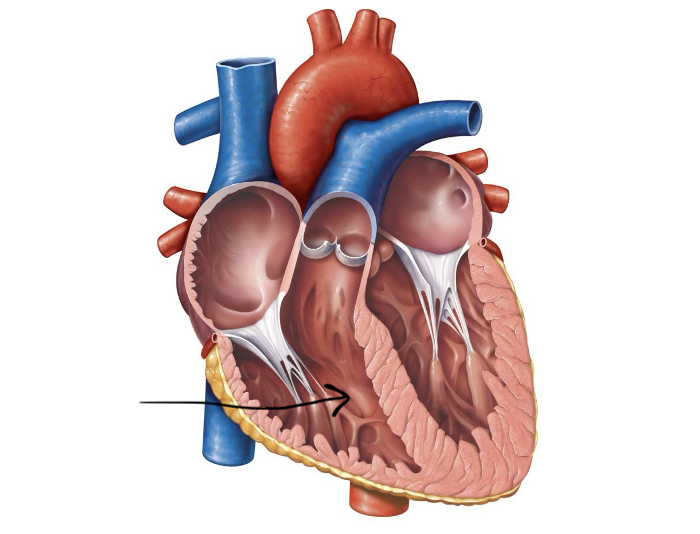
Label and function
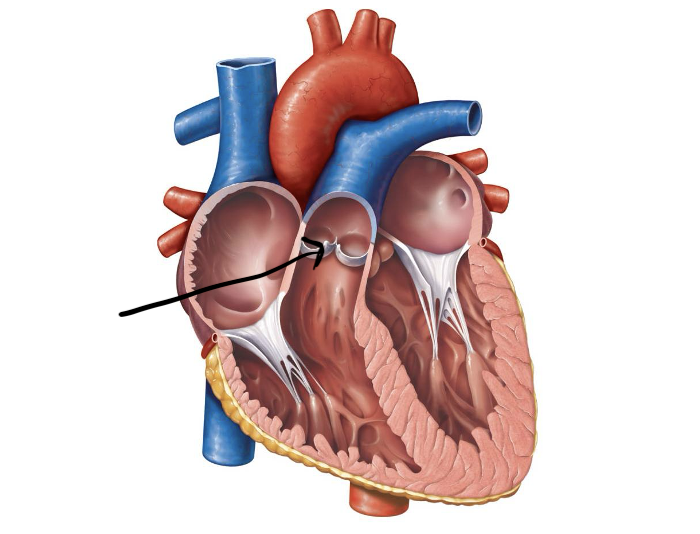
Right atrioventricular valve, prevents blood from flowing back into the right atrium
Label and function
Left atrioventricular valve, prevents blood from flowing back into the left atrium
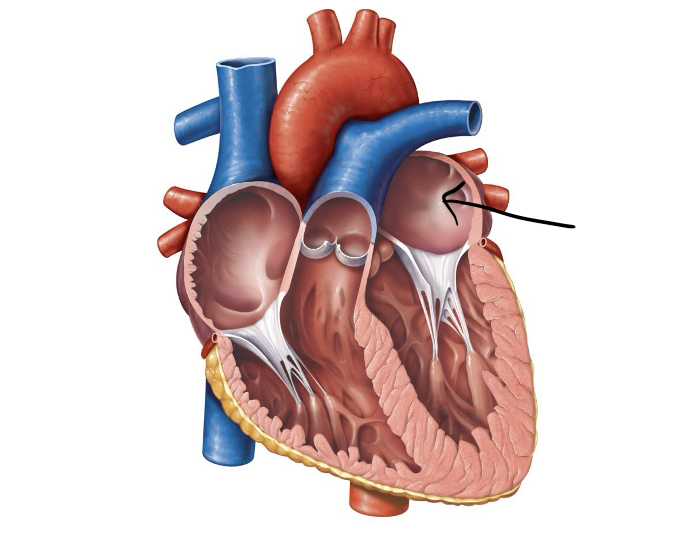
Label and function
Left ventricle, pumps oxygenated blood into the aorta
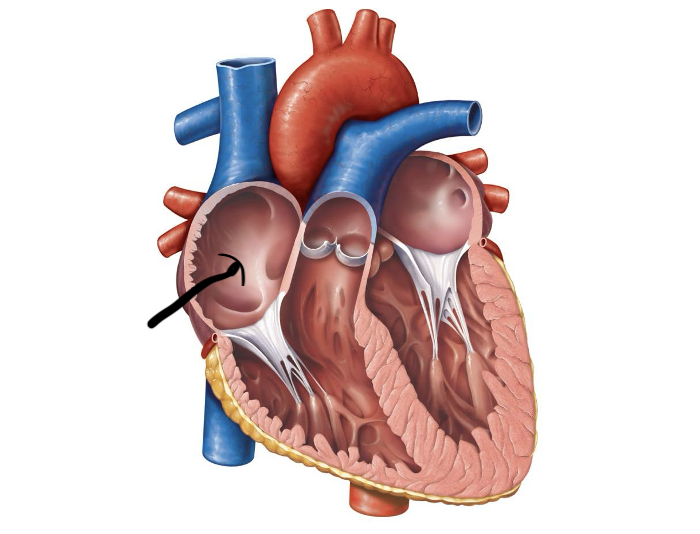
Label and function
Right atrium, pumps deoxygenated blood into the right ventricle
Label and function
Right ventricle, pumps blood into the pulmonary trunk
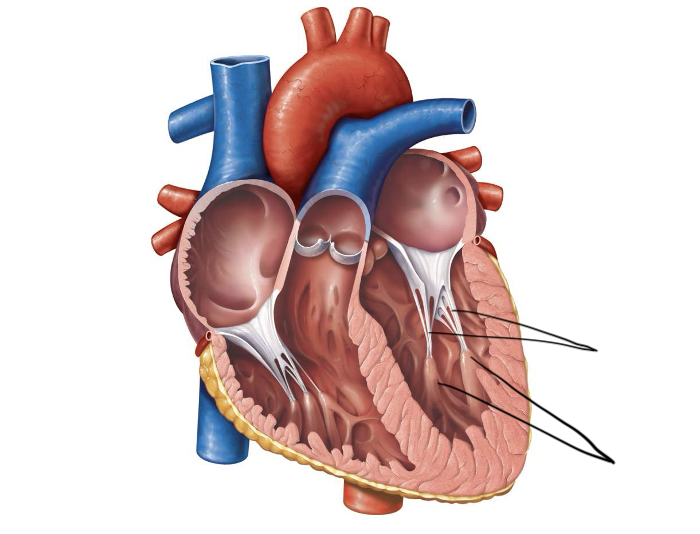
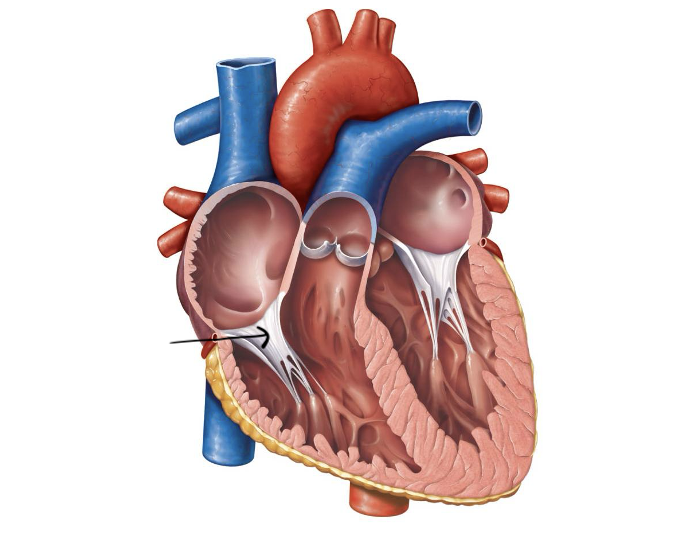
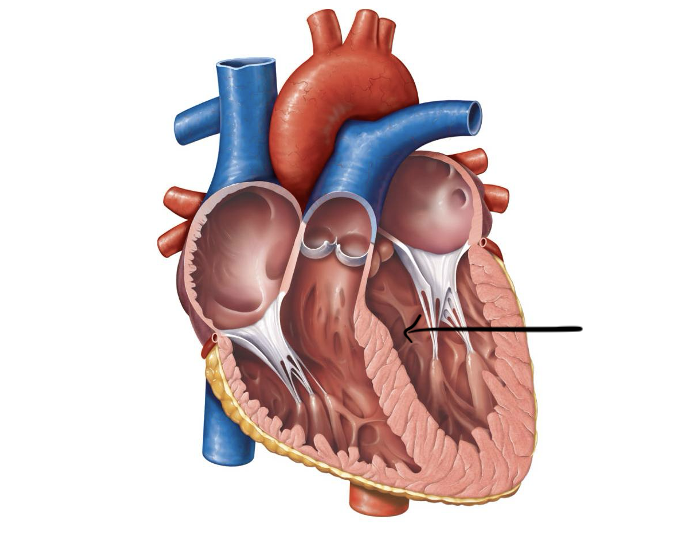
Label and function
Chordae tendineae and papillary muscles, help maintain valve functions