LAM- Equine Neurology
1/91
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
92 Terms
Is cortical blindness a clinical sign of fore brain disease?
Yes
Classic signs of brainstem disease
Alterations in consciousness/arousal
Cranial nerve deficits
Vestibular signs
Gait&Posture deficits
What coordinates motor activity
Cerebellum
What is the real teller of cerebellar disease?
Intention head tremor
If body movements are on the left side during a seizure, what side is the lesion?
Right side of cerebral cortex
If cortical blindness in right eye, what side is lesion ?
Left side
Place catheter in horse after seizure when recumbant, why?
Because likely to seize again
Drugs for seizure management?
Benzos
Barbs (phenobarb)
What drug is for short term control to avert or mitigate a seizure?
Benzo
Bolus injection
What would you use to suppress seizures in encephalopathic neonatal foals
midazolam CRI
What is used for longer term control?
Phenobarb
Oral daily dose for recurring seizures
Levetiracetum for long term control?
What are some conditions in neonatal foals causing seizures?
Neonatal encephalopathy
due to perinatal oxygen deprivation
Metabolite/electrolyte disturbances
Bacterial meningitis (rare)
Congenital development defects
Seizures can be heritable in foals in what breed?
Arabian
Arabian foals with seizures typical have them at what age?
before 6 months
avg 2 months
What is treatment for lavender foal syndrome?
Nothing- euthanize
What is a developmental disease of egyptian arabian foals?
Cerebellar abiotrophy
Will not grow out of
Cerebellar abiotrophy foals will develop what and by what age?
generalized cerebellar disease
6 months
What is treatment for cerebellar abiotrophy?
No treatment
With cranial trauma, what is the essential lesion?
Brain edema
Common injuries from horses flipping over backwards?
Petrous temporal and occipital injuries
What are some controversial managments of counteracting brain edema?
Dexmethasone/corticosteroids
IV Dimethyl sulfoxide
Can you use mannitol with intracranial hemorr?
No - but it can be used otherwise to counteract brain edema
What two plants may cause nigropallidal encephalomalacia?
Yellow star thistle
Russian knapweed
Clinical signs of nigropallidal encephalomalacia?
Causes dystonia, can't swallow and no prehension, sardonic grin
Is there treatment for nigropallidal encephalomalacia?
No
Ddx clinically but could be MRI
Locoism is an acquired ___________________________ storage disease caused by consuming _____________ of the genera ________________&________________
polysaccharide
plants
Oxytropis
Astragalus
Signs of locoism?
Generalized ataxia, behavioural changes, intention tremor- similar signs to cerebellar disease
With locoism what may you see in the blood lymphocytes?
Intraplasmic vacuoles
Do horses with locoism recover?
No- permanent neurological deficits
What is the fungal species associated with moldy corn poisoning?
Fusarium verticilloides
What is scientific name of moldy corn disease
Leukoencephalomalacia
Whats the principle toxic agent for mcp?
fumonisin B
What does moldy corn disease cause?
Asymetric liquefactive necrosis of the cerebral hemispheres, cerebellum, brainstem and spinal cord
Clinical signs of Moldy corn poisoning?
Rapidly progressive encephalopathy
incoordination, aimless walk, blindness, head pressing
How do you diagnose moldy corn poisoning?
Clinical signs and the feed
No cure- very fatal
Who are brain abcesses most common in and why?
Young horses from whacking their heads
What is a RARE complication of neonatal sepsis?
meningitis
How do diagnose brain infection?
CSF with increasaes neutrophils and protein
MRI can localize abscess
Diagnosis of brain infection?
Inflammatory leukogram with increased fibrinogen
Management for infection in brain?
Abx- penicillin or sulfas
Anti-inflammatories, NSAIDs, DMSO maybe steroids
Phenobarb for sedations or potential seizures
Whats prognosis for brain infection?
GUARDED to poort
What is most common in north america? EEE or WEE?
EEE
Vector for EEE?
Mosquito- so seasonal, year round in warm parts of america
How do you prevent EEE and WEE
Vaccine
Clinical signs of EEE
1-3 weeks incubation
High fever with rapid progressive encephalopathy
How diagnosis confirmed?
IgM capture on Elisa
Prognosis of EEE and WEE?
guarded to poor
Vaccine schedule for EEE and WEE
2 doses 4-6 weeks apart then revaccinate annually
In endemic areas in SE , foal may be started on _____ dose seroes at 3-4 months of age
4
Adults may be immunized semi annually as well
West nile is also a mosquito borne encephalomyelitis virus that affects what part of the brain?
Gray matter primariily in brainstem and spinal cord
Clinical signs of WNV
Generalized weakness, gait deficits, stumbling falling
Muscle fasciculations, blinking and twitching of muzzle
With rabies, encephalopathic signs may take sime time to appear, when they do show, they progress ____________
rapidly
Encephalopathy with rabies is often characterized as?
hyperesthesia, self mutilation, recumbence and death
How do horses sometimes feel about water with rabies?
Hydrophobia
Horses exposed to rabies be re-vaccinated and undergo observation for how many days?
60 days
How long is quarantine for non vaccinated horses?
6 months
Immunization is best prevention!
What type of vaccine is rabies vax?
Killed
How many doses do adults need?
1 single dose followed by yearly booster
When do foals get vaxxed for rabies?
Foals of vaccinated mares get two doses at 6&7 months
When do foals of unvaccinated mares get vaxxed?
3-4 months or as per label
What is the definitive host for equine protozoal myeloencephalitis
opossum
skunk, raccoon, cat, and 9 banded armadillo are intermediate hosts
What is the dead end host for equine protozoal myeloencephalitis?
Horses
It is most common infectious equine CNS disease in the united states
What protozoan parasite cause equine protozoal myeloencephalitis?
Sarcocystis neurona
Where will equine protozoal myeloencephalitis localize most commonly?
Brain stem and spinal cord
Can be anywhere tho
With EPM are lesions local or multifocal?
Can be both!
It can also affect gray and white matter
______________________ signs are typcial and LMN signs are common
asymmetrical
What are the characteristic signs for EPM?
Asymmetrical ataxia and muscle atrophy
Three A's
What do lesions of the cervical intumescense cause with EPM?
asymmetrical flaccid paresis and focal atrophy of fore limb muscles and long tract signs in rear limbs
What do lesions of the lumbar intumescence with EPM cause?
asymmetrical flaccid paresis and focal muscle atrophy of gluteal and thigh muscles
Do you see facial paralysis with EPM?
Yes you can
How do you diagnose EPM?
Rule out other options with CT or MRI
Immunodiagnostic testing
EPM diagnosis is made complicated by what?
High seropositivity
Low prevalence
Major differentials are common
Common differentials for EPM?
CSM
EDM
WNV
EHV1
What is immunodiagnostic testing good for?
S neurona antibodies in serum and CSF
What serum to CSF ratio is stronly supportive of EPM?
Serum to CSF ratio < 100
less than 100 tells us theres a high antibody titre in the csf which is strongly supportive of EPM
What are the treatments for EPM?
Ponazuril (marquis)
Diclazuril
Potentiated sulfas - sulfadiazine/pyrimethamine
With mild cases- what percent have full recovery of EPM?
50% have full recovery
With severe cases of EPM, what % have full recovery?
10-20%
What can Parelaphostrongylus cause?
Verminous myeloencephalitis
What is treatment for Verminous myeloencephalitis?
anthelmintics and supportive care, but prognosis is GUARDED
Vestibular disease
functions to
maintain posture, muscle tone and equilibrium
orientation of head with respect to eyes, trunk, limbs
special proprioception
clinical signs
head tilt
drifting or listing to one side
resting nystagmus
can be
central, involving the medulla, pons and or cerebellum
peripheral involving the vestibular branch of CN8; peripheral vestibular disease is common in horses
Peripheral vestibular disease
components of the vestibular branch of CN8 are ‘
the receptor organ in the middle ear (hair cells in endolymph)
the vestibular ganglion
the afferent axons projecting into the brainstem
these structures are located within and near the petrous temporal bone
the signs of disequilibrium are ipsilateral to the lesion
head tilt, leaning, drifting, falling, rolling
resting horizontal nystagmus, fast phase is away form the side of the lesion; sometimes rotary
Peripheral vestibular disease and facial nerve paralysis
common disease in horses
occurs with traumatic, infectious, inflammatory, or degenerative conditions of petrous temporal bone and or nearby structures (tympanic bullae / inner ear)
examples are petrosal impact/fractures, temporohyoid osteo-arthorpathy (THO), maybe otitis media-interna
there is a close anatomic relationship of CNs 7 and 8 such that dz in this area may result in vestibular signs, facial nerve paralysis or both
trauma and THO are common cause of each / both
polyneuritis equi and LSA are add causes of FNP
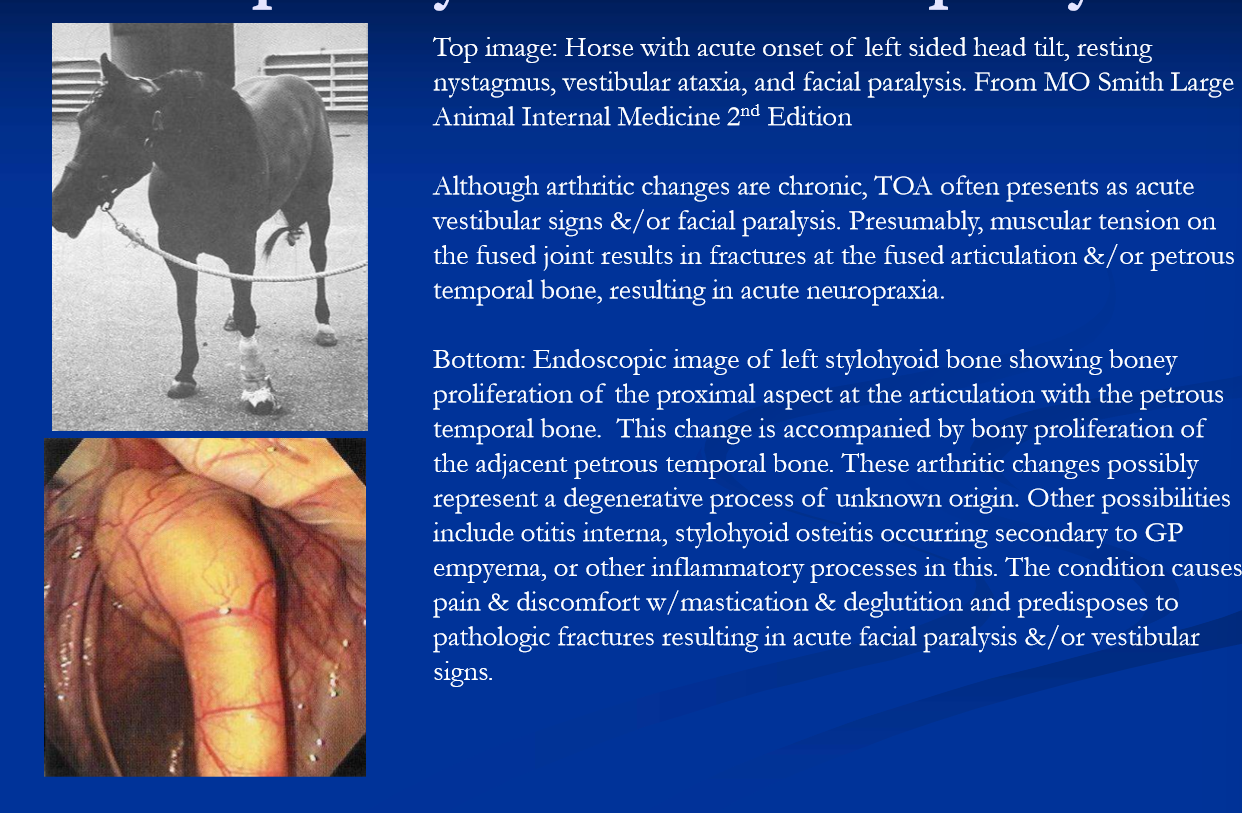
Temporohyoid oestoarthropathy
bony proliferation, enlargement and sclerosis of the temporohyoid articulation and adjacent bone
periosteal reaction involving stylohyoid bone, petrous temporal bone and tympanic bulla
end result is fusion of the temporohyoid articulation, stenosis of external ear canal, obliteration of tympanic bulla
cause is incompletely understood; possibilities include:
chronic changes initiated by otitis media, maybe GP disease
cribbing
or maybe a primary degenerative process
progressive bony changes and ultimate fusion of the joint results in
signs of discomfort such as difficulty with mastication, rubbing the head on the affected side, head-shaking
**spontaenous fracture of the petrous temporal bone
due to tension on the fused articulation from muscle contractions of the tongue, pharynx and neck
fx results in acute vestibular ataxia and or facial paralysis
signs and lesions are most often unilateral ,although up to 20% have bilateral bony changes
management of THO
Acute vestibular signs ± facial paralysis is treated with anti-inflammatory drugs and antibiotics
antibiotics are indicated due to potential for bacterial translocation into the brain case; also if active otitis or osteomyelitis is suspected
with facial paralysis* the eye on the affected side should be protected with topical antibiotic ointments or tarsoraphy
surgical intervention can prevent the fracture*
disarticulation of the hyoid apparatus on the affected side via ceratohyoidectomy
otitis media-interna
presumably it can cause acute vestibular signs ± facial palsy in horses
diagnosis can be challenging
definitive dx with tympanocentesis, cytology and culture
imaging: rads / CT / MRI
antibiotic treatment should resolve mild/early cases
extension of infection beyond the inner ear can lead to osteoyelitis of the calivarium
extension of infection centrally which leads to subdural abscess and or meningitis and severe CNS signs
also secondary pathologic fx can result in hematoma/hemorrhage into the brain case and acute vestibular signs
both have guarded prognosis
for less severe cases, aggressive antibiotic and anti-inflammatory tx are indicated and may resolve the signs
CN IX and X: pharyngeal and laryngeal paresis / paralysis
signs/complications include dysphagia, choke, upper respiratory obstruciton, aspiration, DDSP; feed in nostrils is a clinical sign of dysphagia
causes
guttural pouch disease mycosis
GP and laryngela surgies
idiopathic left laryngeal hemiplegia
laryngeal hemiplegia also occurs with injuries to recurrnet laryngeal nerve; can occur on either side
bilateral laryngela paresisi paralysis occurs with
lead poisoning; causes generalized polyneuritis in horses; laryngeal / pharyngeal signs clinically prominent; abnormal phonition often sites as early / characteristic sign
botulism: early signs are weak tongue and masticatory efforts difficuly swallowing (dysphagia) may present as choke
bilateral laryngela pralysis with pyrodizadine tox/hep encephaloaphty
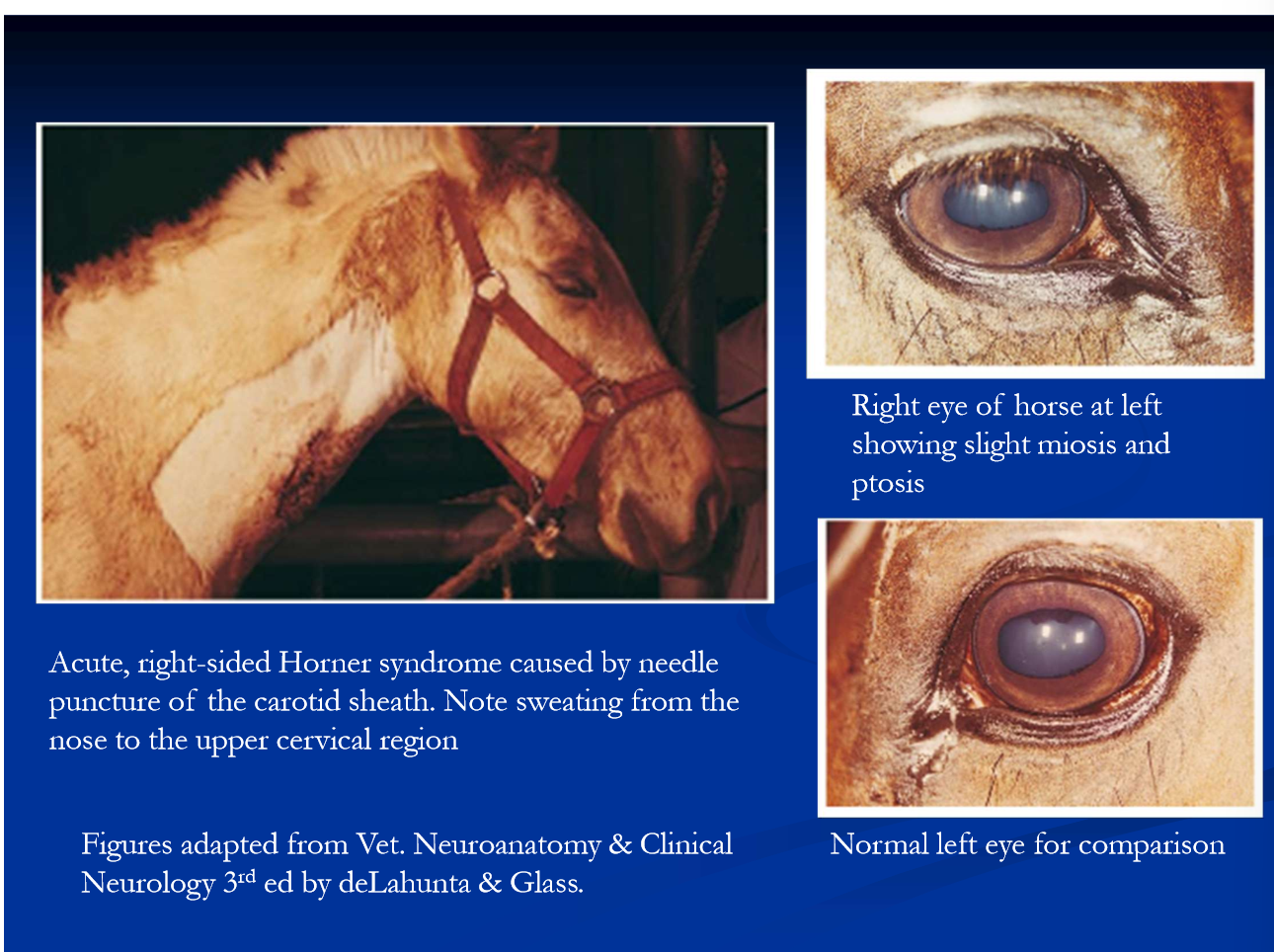
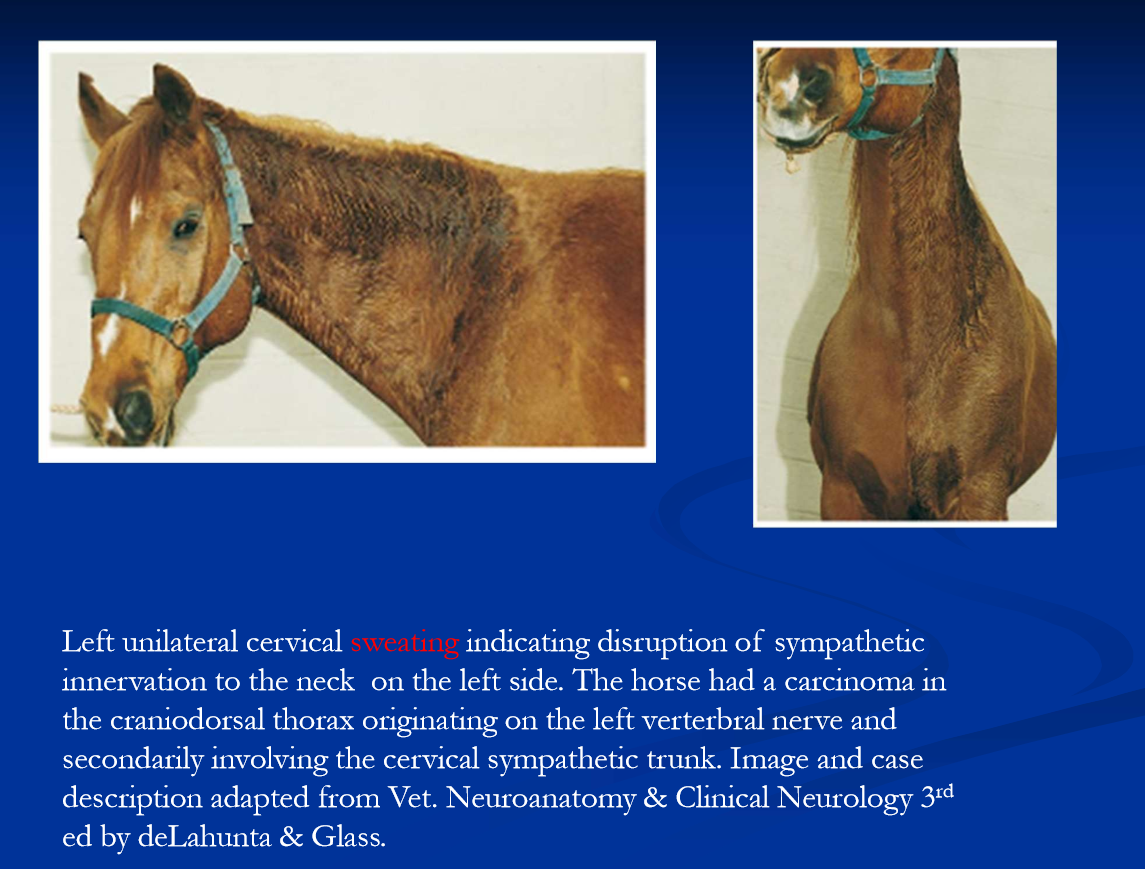
Horner syndrome in horses
signs are ptosis, enophthalmus, 3rd eyelid prolapse, miosis
facial sweating in horses
focal sweating occurs with any local sympathic injury in horses
the pattern of sweating is helpful in localizations
some causes of horner syndrome in horses include
cranial trauma
GP disease
cervical injuries ex injection site injury***
spinal cord disease or injury at T2
brachial plexus / nerve root disease or injury (avulsion)
thoracic trauma or mass
Neuropathic head shaking
hyperesthesia caused by neuropathy of ophthalmic branch of CN V (sensory trigeminal neuropathy)
head shaking is induced by exposure to light and other environmental stimuli
may also show sneezing, snorting, nose rubbing
many have seasonal pattern
dx supported when headshaking is improved with dark environment, blindfold and or UV mask
other causes of headshaking are ruled out
management
mechanical distractors example nose nets
drug treatments include cyrproheptadine and carbamazepin
many cases are progressive and debilitating resulting in loss of use and or humane euthanasia
cauda equine neuritis / polyneuritis equi
chronic, progressive granuloamtous inflammation causing fibrosis and adhesions of peripheral nerve roots
classically affects the nerves of the cauda equina resulting in cauda equina syndrome
less commonly, cranial nerves and other spinal nerve are affected
the cause is unknown believed to be an immune-mediated process
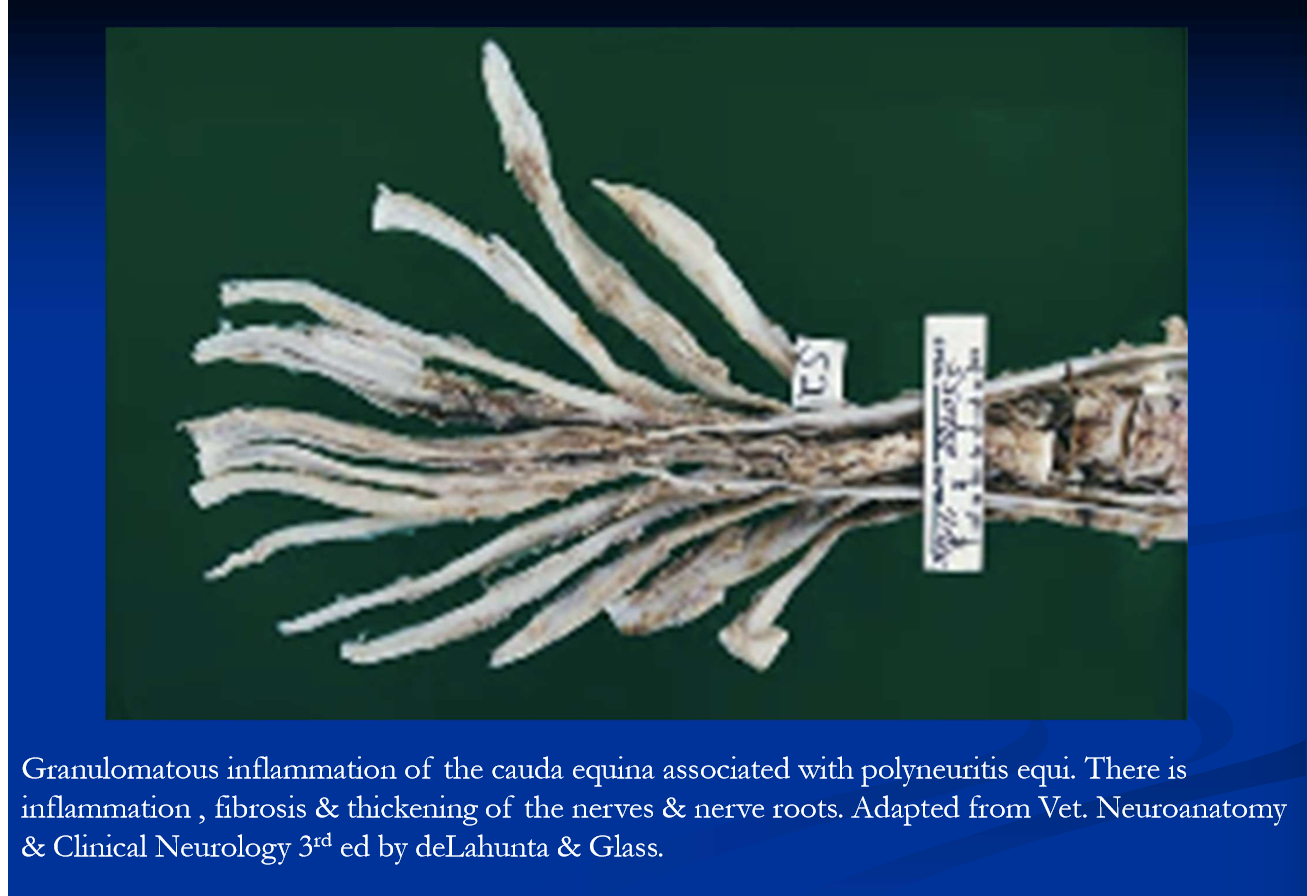
Polyneuritis equi
initial signs inlcude hyperesthesia around the rump and tail-head manifested as tail rubbing; m/b mild dysuria
over weeks to months there is progressive development of a cauda equine sydnrome
flaccid bladder with overflow incontinence and urine scalding, fecal rentention, atrophy and paralysis of tail head muscles, perineal anesthesia, penile prolpase and anesthesia, hyperesthesia peripheral to perinuem
some show atrophy of hind quarters and mild hind limb ataxia
cranial n deficits when present are typically unilateral
there is no specific treatment
corticosteroids and other immunosuppressive drugs may have a temporary benefit
can be temporarily managed with urinary bladder catherization and manual rectal emptying as needed and nursing care
humane euthanasia is the usual course