Neurological Disorders and Motor Control Theories
1/132
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
133 Terms
What are the main causes of Parkinson's disease?
Genetic and environmental factors; the exact cause is unknown.
Which structures in the basal ganglia are involved in Parkinson's disease?
Substantia nigra compacta.
What happens to dopaminergic receptors in Parkinson's disease?
There is a loss of dopaminergic receptors.
How does the activity of the direct and indirect loops change in Parkinson's disease?
There is decreased activity of the direct loop and increased activity of the indirect loop.
What are the cardinal signs of Parkinson's disease?
Rigidity, akinesia, bradykinesia, tremor, and postural instability.
What are some symptoms associated with Huntington's disease?
Dystonia, chorea, impaired voluntary movements, gait and balance issues, speech and swallowing difficulties.
What cognitive impairments are seen in Parkinson's disease?
Slowed thinking and information processing, difficulty with attention, problem solving, planning, short and long-term memory issues, and visuospatial difficulties.
What speech dysfunctions are common in Parkinson's disease?
Low volume, mumbling, and freezing.
What autonomic nervous system symptoms are associated with Parkinson's disease?
Orthostatic hypotension, supine hypertension, constipation, dysphagia, excessive salivation, urinary and sexual dysfunction, and sweating abnormalities.
What is a common first symptom of gastrointestinal involvement in Parkinson's disease?
Constipation.
What are some common medications used to treat Parkinson's disease?
Levodopa, carbidopa, dopamine agonists, MAO-B inhibitors, COMT inhibitors, amantadine, and anticholinergics.
What medications are specifically used for Huntington's disease?
Tetrabenazine (Xenazine), deutetrabenazine (Austedo), haloperidol, olanzapine, and risperidone.
What standardized measures are commonly used for assessing Parkinson's disease?
MOCA, 9-hole peg test, PDQ-8, MDS-UPDRS, Freezing of gait questionnaire, and Parkinson's fatigue scale.
Which standardized measure is specifically used for Huntington's disease?
Unified Huntington's Disease Rating Scale (UHDRS).
What is the primary role of dopamine in normal basal ganglia function?
Dopamine facilitates movement by enhancing excitatory signals that initiate voluntary motor activity.
How do D1 and D2 receptors function in the basal ganglia?
D1 receptors facilitate movement by enhancing excitatory signals; D2 receptors reduce inhibitory output to promote motor activity.
What is the role of the substantia nigra pars compacta (SNc) in dopamine production?
The SNc produces dopamine and sends it to the striatum (caudate nucleus and putamen).
What are some cardiovascular symptoms associated with Huntington's disease?
Orthostatic hypotension, reduced heart rate variability, and resting tachycardia.
What are some urinary symptoms associated with Huntington's disease?
Urgency, frequency, and incontinence.
What are common sweating and temperature regulation issues in Huntington's disease?
Abnormal sweating (hyperhidrosis or anhidrosis) and heat/cold intolerance.
What pupillary response abnormalities can occur in Huntington's disease?
Occasionally sluggish or abnormal pupillary response.
What are the characteristics of nystagmus in peripheral versus central causes?
Peripheral nystagmus is almost always present and typically unidirectional, while central nystagmus is frequently present and may be vertical, unidirectional, or multidirectional.
What symptoms are associated with cochlear nerve dysfunction in peripheral and central cases?
Peripheral symptoms may include ringing in the ears and decreased hearing, whereas central symptoms are uncommon.
What brainstem region signs are indicative of central versus peripheral issues?
Peripheral issues show no signs, while central issues may present with motor or sensory deficits, Babinski's sign, dysarthria, limb ataxia, or hyperreflexia.
How does nausea and vomiting differ between peripheral and central causes?
Peripheral causes typically result in moderate to severe nausea and vomiting, while central causes lead to mild symptoms.
What is oscillopsia and how does it present in peripheral versus central lesions?
Oscillopsia is when objects appear to jiggle even when stationary; it is mild in peripheral lesions and severe in central lesions.
What are the characteristics of cerebellar ataxia?
Cerebellar ataxia includes a wide-based, unsteady gait, dysmetria (overshooting or undershooting), intention tremor, and difficulty with rapid alternating movements (dysdiadochokinesia).
What are the signs of vestibular ataxia?
Vestibular ataxia presents with an unsteady gait, often worsening with head movements, and may include leaning or falling toward the side of the lesion.
What sensory ataxia signs are observed?
Sensory ataxia includes an unsteady gait, especially in the dark or with eyes closed, a positive Romberg sign, and a 'stamping' gait to enhance sensory feedback.
What is the grading and prognosis for glioblastoma?
Glioblastoma is graded IV and has the worst prognosis.
What treatments are available for glioblastoma?
Treatment options for glioblastoma include surgery, radiation, and chemotherapy.
What percentage of pediatric and adult tumors does glioblastoma represent?
Glioblastoma accounts for 20% of pediatric tumors and 50% of adult tumors.
What is the grading and prognosis for astrocytoma?
Astrocytoma is graded II and has a moderate prognosis.
What treatments are available for astrocytoma?
Treatment options for astrocytoma include surgery, radiation, and chemotherapy.
What percentage of pediatric and adult tumors does astrocytoma represent?
Astrocytoma accounts for 21% of pediatric tumors and 10% of adult tumors.
What is the grading and prognosis for meningioma?
Meningioma is graded I and has the best prognosis.
What treatments are available for meningioma?
Treatment options for meningioma include observation, surgery, and radiation.
What percentage of pediatric and adult tumors does meningioma represent?
Meningioma accounts for 5% of pediatric tumors and 17% of adult tumors.
What is the grading and treatment for schwannoma/neuroma?
Schwannoma/neuroma is graded I-II and is treated with surgery (removal of the nerve).
What percentage of pediatric and adult tumors does schwannoma/neuroma represent?
Schwannoma/neuroma accounts for 1% of pediatric tumors and 2% of adult tumors.
What are the symptoms associated with an ACA stroke?
Symptoms include paresis of the contralateral foot and leg, mental impairment (perseveration, confusion, amnesia), sensory impairments primarily in the lower extremity, and problems with imitation and bimanual tasks.
What are the symptoms associated with an MCA stroke?
Symptoms include paresis of the contralateral face, arm, and leg (with the leg being least affected), sensory impairment over the contralateral face, arm, and leg, motor speech disorder or Broca's aphasia (left CVA), Wernicke's or receptive aphasia (left CVA), perceptual problems, and homonymous hemianopia.
What are the symptoms associated with a PCA stroke?
Symptoms include contralateral homonymous hemianopia, prosopagnosia, thalamic syndrome (sensory impairments, spontaneous pain, dysthesias), involuntary movements (choreoathetosis, intention tremor, hemiballismus), and contralateral hemiplegia.
What are the warning signs of a stroke?
Warning signs include sudden weakness or numbness of the face, arm, or leg, sudden dimness or loss of vision in one eye, sudden difficulty speaking or understanding speech, sudden seizure, and unexplained dizziness or falls.
What are the main causes of infarction in strokes?
The main causes of infarction include cerebrovascular disease (50% of strokes), lipohyalinosis, and cerebral embolism.
What are the characteristics of nystagmus in peripheral versus central dysfunction?
Peripheral nystagmus is almost always present and typically unidirectional, while central nystagmus is frequently present and may be vertical, unidirectional, or multidirectional.
What brainstem region signs differentiate peripheral from central dysfunction?
Peripheral dysfunction shows no signs, while central dysfunction may present with motor or sensory deficits, Babinski's sign, dysarthria, limb ataxia, or hyperreflexia.
How do nausea and vomiting symptoms differ between peripheral and central dysfunction?
Peripheral dysfunction typically causes moderate to severe nausea and vomiting, while central dysfunction causes mild symptoms.
What is oscillopsia and how does it differ in peripheral versus central dysfunction?
Oscillopsia is the perception that objects jiggle even when stationary; it is mild in peripheral dysfunction unless the lesion is bilateral, and severe in central dysfunction.
Describe the characteristics of ataxia in cerebellar, vestibular, and sensory dysfunctions.
Cerebellar ataxia includes wide-based, unsteady gait, dysmetria, and difficulty with rapid alternating movements. Vestibular ataxia leads to unsteady gait, often worse with head movements, while sensory ataxia results in unsteady gait, especially in the dark, with a positive Romberg sign.
What is the grading and prognosis of glioblastoma?
Glioblastoma is graded IV, indicating the worst prognosis, and treatment typically involves surgery, radiation, and chemotherapy.
What is the grading and treatment for astrocytoma?
Astrocytoma is graded II, with treatment options including surgery, radiation, and chemotherapy.
What is the prognosis and treatment approach for meningioma?
Meningioma is graded I, indicating the best prognosis, with treatment options including observation, surgery, and radiation.
What are the main symptoms of an ACA stroke?
Symptoms include paresis of the contralateral foot and leg, mental impairment (perseveration, confusion, amnesia), sensory impairments primarily in the lower extremity, and problems with imitation and bimanual tasks.
What are the key symptoms of PCA stroke?
Symptoms include contralateral homonymous hemianopia, prosopagnosia, thalamic syndrome (sensory impairments, spontaneous pain, dysthesias), involuntary movements (choreoathetosis, intention tremor, hemiballismus), and contralateral hemiplegia.
What are the characteristics of intracerebral hemorrhage?
Intracerebral hemorrhage has a 40% 30-day mortality rate, with primary causes being hypertension and is most common in the basal ganglia or thalamus.
What is the most common cause of subarachnoid hemorrhage?
The most common cause of subarachnoid hemorrhage is arteriovenous malformation.
What are the main causes of infarction leading to stroke?
The main causes of infarction include cerebrovascular disease (50% of strokes), lipohyalinosis, and cerebral embolism, with a 15% 30-day mortality rate.
What are the functions of the frontal lobe?
The frontal lobe includes the prefrontal association cortex, primary motor cortex, supplementary motor areas, motor planning areas, and premotor area.
What are the functions of the temporal lobe?
The temporal lobe is responsible for auditory association and primary auditory functions.
What are the functions of the parietal lobe?
The parietal lobe includes the primary somatosensory area, sensory association area, and parietotemporal association area.
What are the functions of the occipital lobe?
The occipital lobe includes the primary visual area and visual association area.
What is the primary function of the insula?
The insula is primarily responsible for vestibular functions.
What is the primary cause of Guillain-Barré syndrome (GBS)?
GBS is primarily an immune-mediated disorder associated with bacterial and viral infections, surgery, and vaccination.
What are some potential causes of peripheral neuropathy?
Potential causes include diabetes, nutritional deficiencies, infections (e.g., HIV), inflammation, toxins, hereditary conditions (e.g., Charcot-Marie-Tooth disease), and trauma.
What is post-polio syndrome?
Post-polio syndrome is related to the initial disorder of the motor neuron cell body affected by poliovirus.
What are the primary types of nerve lesions associated with ALS?
Lesions to spinal nerve roots in the PNS, peripheral nerves (motor, sensory, autonomic), myelin sheath, axons, and cranial nerves.
What ongoing condition occurs due to muscle denervation in ALS?
Ongoing muscle denervation leads to the evolution of original motor neuron dysfunction after the poliovirus affects the alpha motor neuron.
What is the role of reinnervation in muscle in ALS?
PPS (Post-Polio Syndrome) reinnervation in muscle cannot maintain muscle fiber innervation.
What happens to motor neurons in ALS?
There is degeneration of motor neurons and attrition of oversprouting motor neurons.
What are the consequences of UMN cell loss in ALS?
Loss of UMN cells occurs in the motor cortex, including loss of Betz cells from Brodmann area 4, frontotemporal cortex, hippocampus, thalamus, and substantia nigra.
What types of sensory impairments are commonly reported in ALS?
Common sensory impairments include pain, atrophy, myalgias, joint pain, numbness, tingling, and burning/shooting pain.
How do motor impairments manifest in individuals with ALS?
Motor impairments include difficulty with balance and coordination, symmetrical muscle weakness starting in the lower extremities, bilateral facial weakness, oculomotor weakness, swallowing difficulties, and respiratory muscle weakness.
What are the differences in motor impairments between UMN and LMN in ALS?
LMN involvement leads to asymmetric weakness, extensor muscle weakness, facial muscle weakness, and early morning cramping, while UMN involvement results in loss of inhibition, lack of dexterity, spasticity, and weakness in specific muscle groups.
What reflexes and tone changes are observed in ALS?
Reflex changes include hyperreflexia, areflexia, hypotonia, and spasticity, noted in 50% of individuals.
What cognitive impairments are associated with ALS?
Cognitive impairments can include difficulties with attention, concentration, memory, word finding, visual attention, working memory, cognitive flexibility, problem solving, and emotional lability.
What is the typical course of ALS disease progression?
The disease is slowly progressive with stable periods lasting 3-10 years, but progression is typically rapid.
How does the progression of ALS symptoms occur?
Progression occurs from distal to proximal, while recovery occurs from proximal to distal.
What are the early symptoms of ALS?
Early symptoms include muscle weakness or stiffness.
What is the average survival rate for individuals with ALS?
The average survival rate is approximately 3 years, but it varies for each individual.
What is the nature of recovery in ALS?
Recovery can be gradual or rapid, and some forms of ALS can be treated while others may lead to permanent damage.
What are some common non-motor symptoms experienced by ALS patients?
Patients may experience emotional outbursts, pathological laughing or crying.
What types of muscle weakness are observed in ALS?
Progression of weakness, wasting, and paralysis of the muscles of the limbs, trunk, and those that control vital functions.
What is the impact of ALS on cognitive function?
While there are no cognitive deficits noted in some cases, others may experience significant cognitive impairments.
What is the relationship between muscle deterioration and aging in ALS?
Strength deterioration in ALS is faster than normal aging.
What are the common assistive devices used by individuals with ALS?
Most individuals with ALS use assistive devices such as crutches and wheelchairs.
What is the significance of autonomic motor signs in ALS?
Autonomic motor signs include bladder and bowel dysfunction.
What sensory symptoms are less commonly reported in ALS?
Less commonly reported sensory symptoms include numbness, tingling, and pain.
What is the primary control mechanism in reflex motor control theories?
Sensory inputs control motor outputs.
What does open loop control demonstrate in motor control theories?
It shows that motor outputs can occur without sensory feedback.
What is a clinical implication of reflex motor control theories?
Use reflexes to facilitate movement.
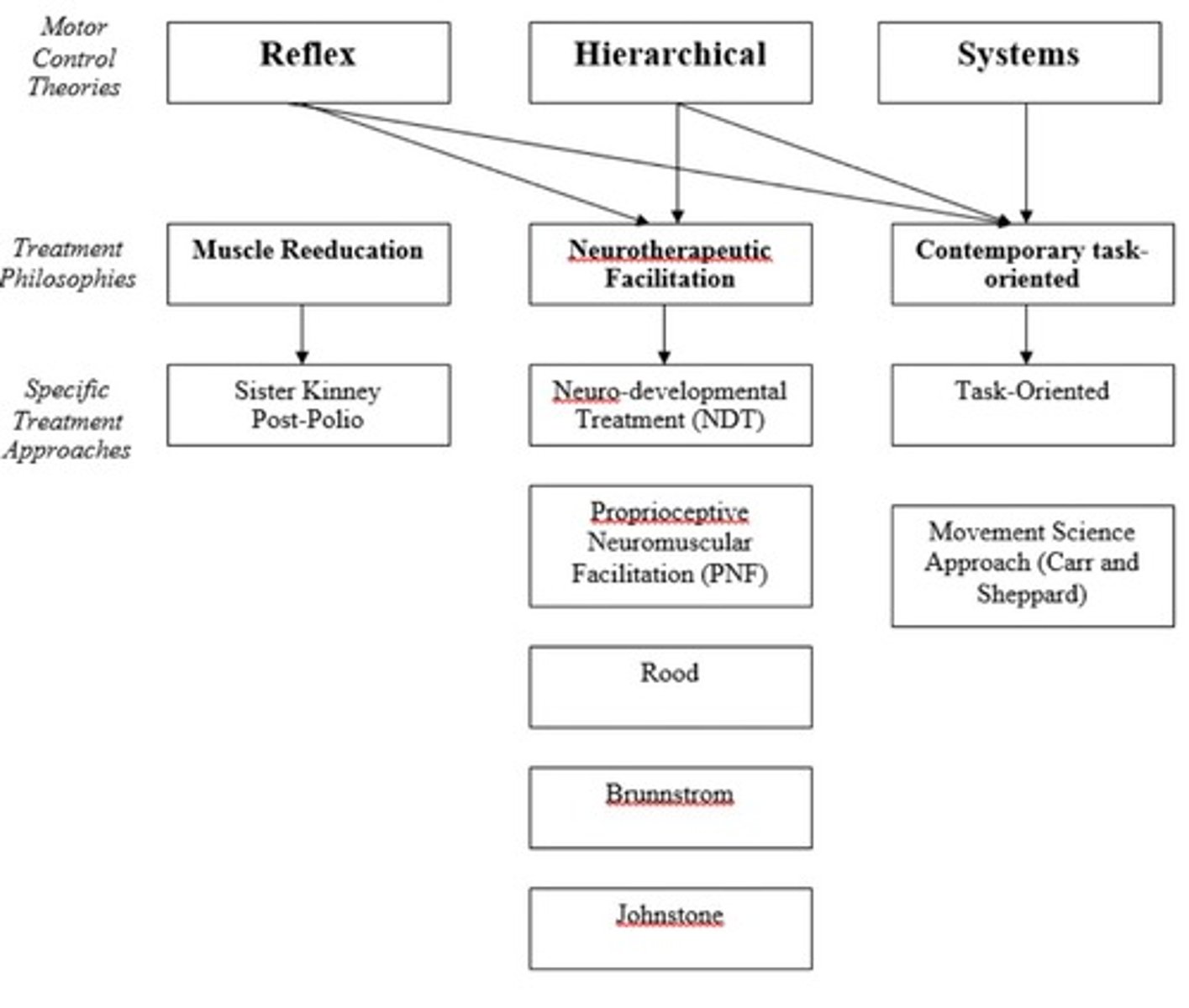
What characterizes hierarchical motor control theories?
They involve a top-down organization and recovery from injury follows developmental progression.
What is a limitation of hierarchical motor control theories?
They do not account for Central Pattern Generators (CPGs).
What are two clinical implications of hierarchical motor control theories?
Facilitate normal reflexes and inhibit primal reflexes.
What is the focus of systems motor control theories?
They emphasize reflexes and synergies as strategies to limit degrees of freedom.
What is a key aspect of systems motor control theories regarding motor behavior?
Interactive systems at the same level control motor behavior to achieve tasks.
What is a clinical implication of systems motor control theories?
Movement is organized around behavioral goals.
What is muscular reeducation in the context of motor control?
It focuses on individual muscles rather than the system and does not consider the CNS.
What is a limitation of muscular reeducation?
Abnormal patterns are typically a problem.
What does neurotherapeutic facilitation aim to achieve?
It aims to affect the nervous system itself rather than just secondary effects on muscles and joints.