Transport In Animals: Exchange & Transport: Biology OCR A Level
Why do multicellular organisms require transport systems?
● Large size (small surface area to volume ratio), subsequently high metabolic rates.
● Demand for oxygen is high, so need a specialised system to ensure a strong supply to all respiring tissues.
Summarise the different types of circulatory system.
● Open= blood can diffuse out of vessels e.g. insects
● Closed= blood confined to vessels e.g. fish, mammals
● Single= blood passes through pump once per circuit of the body
● Double= blood passes through heart twice per circuit of the body
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
Why do multicellular organisms require transport systems?
● Large size (small surface area to volume ratio), subsequently high metabolic rates.
● Demand for oxygen is high, so need a specialised system to ensure a strong supply to all respiring tissues.
Summarise the different types of circulatory system.
● Open= blood can diffuse out of vessels e.g. insects
● Closed= blood confined to vessels e.g. fish, mammals
● Single= blood passes through pump once per circuit of the body
● Double= blood passes through heart twice per circuit of the body
Relate the structure of arteries to their function.
Thick, muscular walls to handle high pressure without tearing. Elastic tissue allows recoil to prevent pressure surges. Narrow lumen to maintain pressure.
Relate the structure of veins to their function.
Thin walls due to lower pressure. Require valves to ensure blood doesn’t flow backwards. Have less muscular and elastic tissue as they don’t have to control blood flow.
Relate the structure of capillaries to their function.
● Walls only one cell thick; short diffusion pathway.
● Very narrow, so can permeate tissues and red blood cells can lie flat against the wall, effectively delivering oxygen to tissues.
● Numerous and highly branched, providing a large surface area.
Relate the structure of arterioles and venules to their function.
● Branch off arteries and veins in order to feed blood into capillaries.
● Smaller than arteries and veins so that the change in pressure is more gradual as blood passes through increasingly small vessels.
What is tissue fluid?
A watery substance containing glucose, amino acids, oxygen, and other nutrients. It supplies these to the cells, while also removing any waste materials.
What types of pressure influence formation of tissue fluid?
● Hydrostatic pressure= higher at arterial end of capillary than venous end.
● Oncotic pressure= changing water potential of the capillaries as water moves out, induced by proteins in the plasma.
How is tissue fluid formed?
As blood is pumped through increasingly small vessels, hydrostatic pressure is greater than oncotic pressure, so fluid moves out of the capillaries. It then exchanges substances with the cells.
How does tissue fluid differ from blood and lymph?
● Tissue fluid is formed from blood, but does not contain red blood cells, platelets, and various other solutes usually present in blood.
● After tissue fluid has bathed cells it becomes
lymph, and therefore this contains less oxygen and nutrients and more waste products.
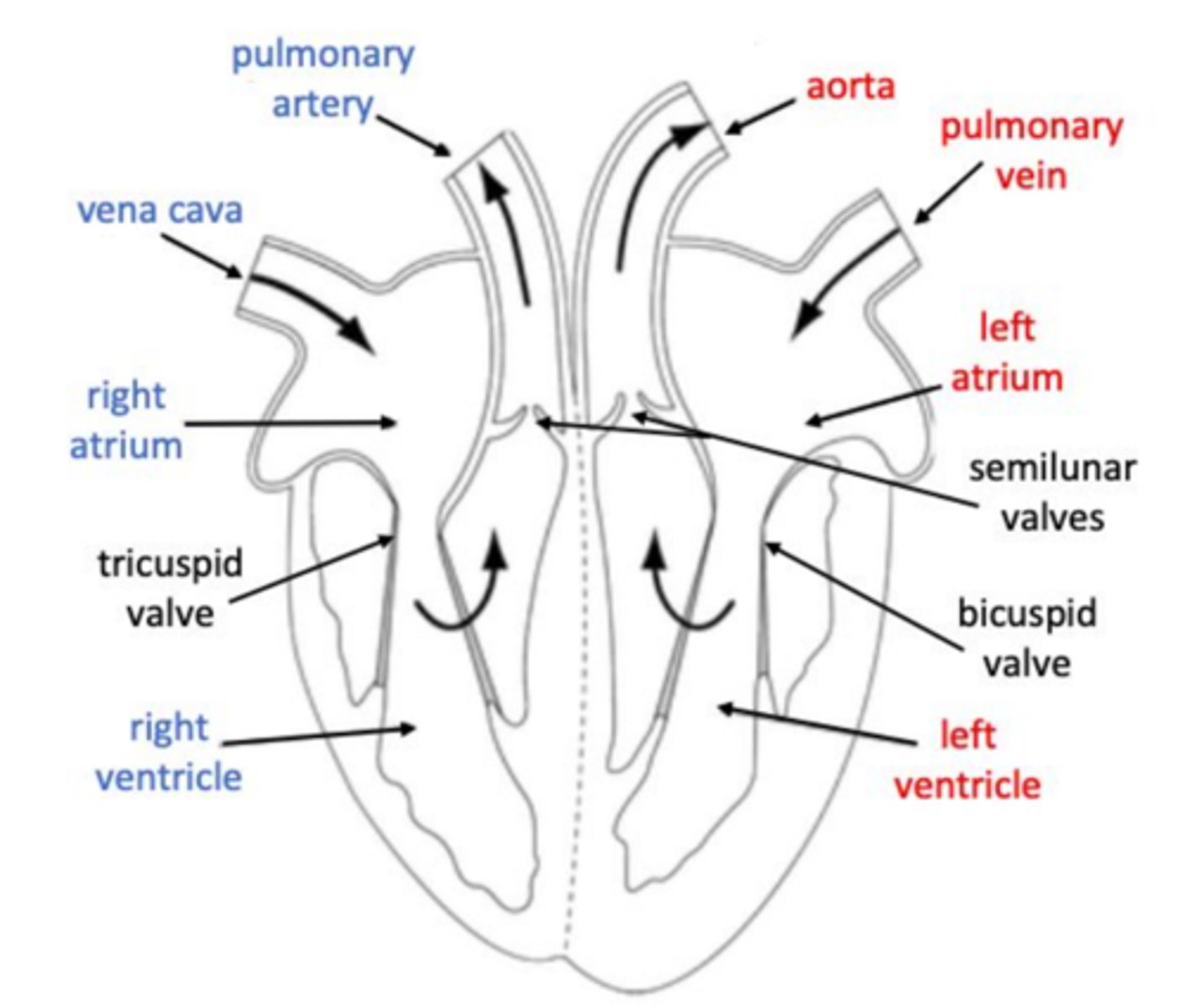
Draw a diagram of the human heart, including names of chambers, vessels, and valves.
Describe what happens during cardiac diastole.
The heart is relaxed.
Blood enters the atria, increasing the pressure and pushing open the atrioventricular valves.
This allows blood to flow into the ventricles.
Pressure in the heart is lower than in the arteries, so semilunar valves remain closed.
Describe what happens during atrial systole.
The atria contract, pushing any remaining blood into the ventricles.
Describe what happens during ventricular systole.
The ventricles contract. The pressure increases, closing the atrioventricular valves to prevent backflow, and opening the semilunar valves. Blood flows into the arteries.
How do you calculate cardiac output?
Cardiac output = heart rate x stroke volume
What does myogenic mean?
The heart’s contraction is initiated from within the muscle itself, rather than by nerve impulses.
Explain how the heart contracts.
● SAN initiates and spreads impulse across the atria, so they contract.
● AVN receives, delays, and then conveys the impulse down the bundle of His.
● Impulse travels into the Purkinje fibres which branch across the ventricles, so they contract from the bottom up.
What is an electrocardiogram (ECG)?
A graph showing the amount of electrical activity in the heart during the cardiac cycle.
Describe types of abnormal activity that may be seen on an ECG.
● Tachycardia= fast heartbeat (over 100bpm)
● Bradycardia= slow heartbeat (under 60bpm)
● Fibrillation= irregular, fast heartbeat
● Ectopic = early or extra heart beats
Describe the role of haemoglobin.
Present in red blood cells.
Oxygen molecules bind to the haem groups and are carried around the body, then released where they are needed in respiring tissues.
How does partial pressure of oxygen affect oxygen-haemoglobin binding?
As partial pressure of oxygen increases, the affinity of haemoglobin for oxygen also increases, so oxygen binds tightly to haemoglobin. When partial pressure is low, oxygen is released from haemoglobin.
What do oxyhaemoglobin dissociation curves show?
Saturation of haemoglobin with oxygen (in %), plotted against partial pressure of oxygen (in kPa). Curves further to the left show the haemoglobin has a higher affinity for oxygen.
Describe the Bohr effect.
As partial pressure of carbon dioxide increases, the conditions become acidic causing haemoglobin to change shape. The affinity of haemoglobin for oxygen therefore decreases, so oxygen is released from haemoglobin.
Explain the role of carbonic anhydrase in the Bohr effect.
● Carbonic anhydrase is present in red blood cells.
● Converts carbon dioxide to carbonic acid, which dissociates to produce H+ ions.
● These combine with the haemoglobin to form haemoglobinic acid.
● Encourages oxygen to dissociate from haemoglobin.
Explain the role of bicarbonate ions (HCO3-) in gas exchange.
Produced alongside carbonic acid. 70% of carbon dioxide is carried in this form. In the lungs, bicarbonate ions are converted back into carbon dioxide which we breathe out.
Describe the chloride shift.
The intake of chloride ions across a red blood cell membrane. This repolarises the cell after bicarbonate ions have diffused out.
How does foetal haemoglobin differ from adult haemoglobin?
The partial pressure of oxygen is low by the time it reaches the foetus, therefore foetal haemoglobin has a higher affinity for oxygen than adult. Allows both mother’s and child’s oxygen needs to be met.