The Adaptive (Specific) Immune System (Part II)- Gonsalves
1/163
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
164 Terms
Antigen challenge
first encounter between an antigen and a naive immunocompetent lymphocyte and an invading antigen
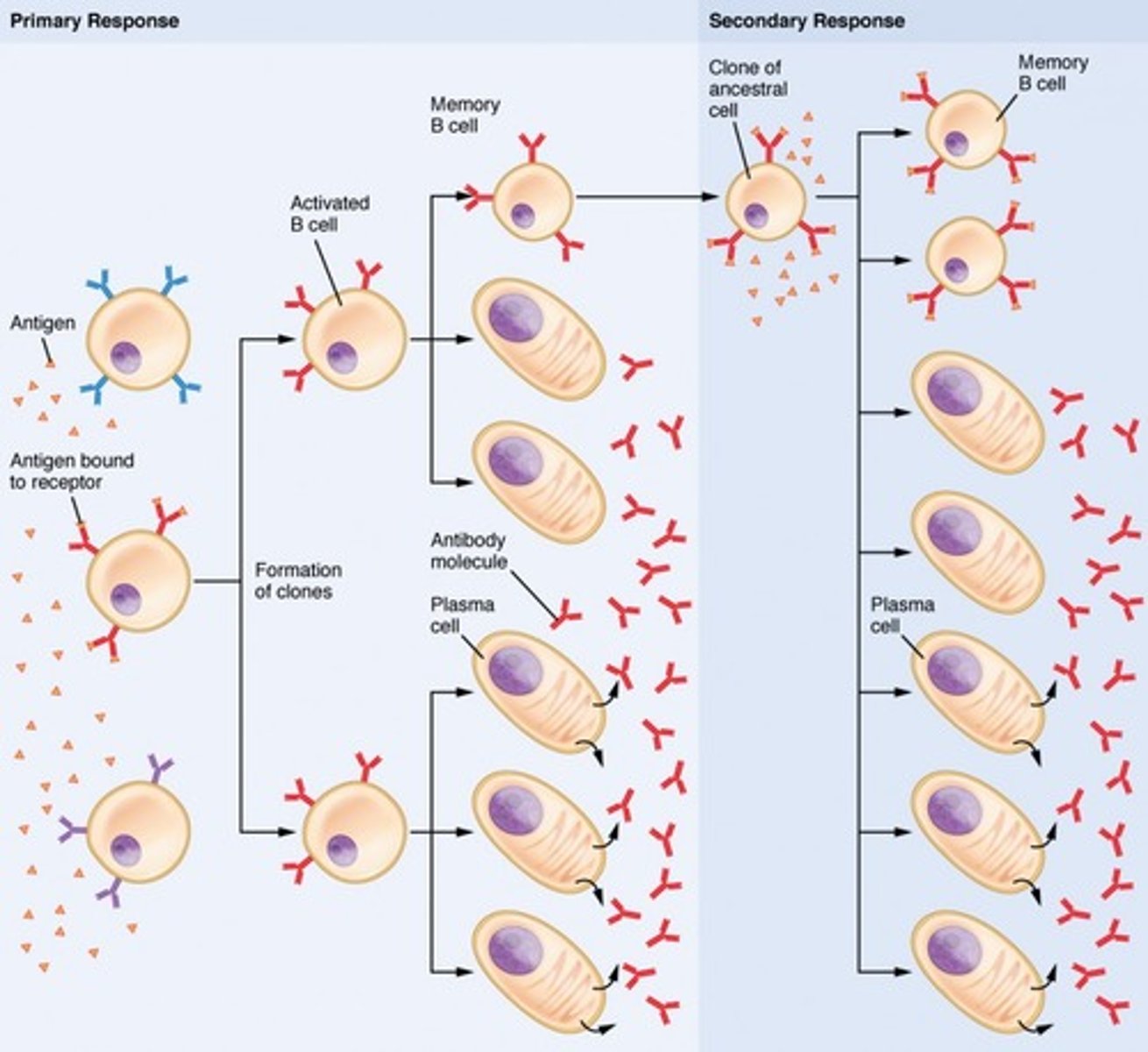
Clonal selection and differentiation of B cells pathway
1. Immunocompetent B cells are activated by antigen binding to receptors on the B cell surface
2. Cross-linked adjacent antigen-receptor complexes are internalized by endocytosis
3. Clonal selection is triggered
4. B cells grow and multiply to form an army of exact replicas called clones
5. Clones become either plasma cells or memory B cells
6. Plasma cells secrete antibodies
7. Memory B cells can mount an almost immediate attack if the same antigen is encountered again
Plasma cells can secrete
antibodies at a rate of 2000 molecules/sec and have a life span of 4-5 days
These cells are long-lived
Memory cells (even up to 75 years!)
What is the primary immune response?
Cellular proliferation and differentiation upon initial exposure to antigen.
Lasts 3-6 days with peak plasma antibody levels reached at about 10 days.
The secondary immune response is the
eexposure to the same antigen = faster and more prolonged than the primary immune response
The secondary response is much faster and stronger due to the
immunological memory of sensitized B cells
The secondary response takes ________ days to reach antibody levels that ___________ those of the primary response.
2-3, EXCEED
Antibodies involved in the secondary response bind with
greater affinity and blood levels remain high for weeks to months
Active humoral immunity
when B cells encounter antigens and produce antibodies against them
2 types of Active Humoral immunity
1. Naturally acquired
2. Artificially acquired
Naturally Acquired active humoral immunity
is obtained by exposure to bacterial and viral infections
Passively Acquired active humoral immunity
obtained from vaccines
Vaccines contain
dead or attenuated (living but extremely weakened) pathogens or part of them
Vaccines can spare us most of the discomfort from a ____________ __________ and provide ______________ _____________ __________________ that are __________________ and reactive.
primary response, functional antigenic determinants, immunogenic
Booster shots
Intensify the immune response, administered after initial vaccine
Vaccines wiped out
smallpox
Vaccines decreased illness like
whooping cough, polio, measles, tetanus, hepatitis B, and pneumonia
Vaccines target what type of cells?
Helper T cells 2(Th2)
What T cells are not specifically targeted by vaccines and why?
Th1 cells (Helper T cells 1) because cellular immunological memory is poorly established, even though they evoke a strong cellular response with lots of antibodies formed.
Vaccines are part of what type of humoral immunity?
Active
In some cases vaccines can cause disease if
the antigen isn't weakened enough or causes an allergic reaction
Naked DNA
are antiviral vaccines and edible vaccines that help prevent allergic responses.
Naked DNA is composed of
plasmid DNA engineered to express a gene of interest, once entered into the host cell.
Passive humoral immunity
antibodies are harvested from the serum of an immune human or animal donor
Does immunological memory occur in passive humoral immunity?
No, immunity ends when the "borrowed" antibodies naturally degrade in the body
Passive immunity can be conferred naturally
from a mother to a fetus and the mother's antibodies can protect the baby for several months
Artificial passive immunity
can come from sera (plural of serum) such as gamma globulin that is administered after hepatitis exporsure, antivenoms, or antitoxins
Antibodies are also called
immunoglobins
Igs
are gamma globulin part of the blood
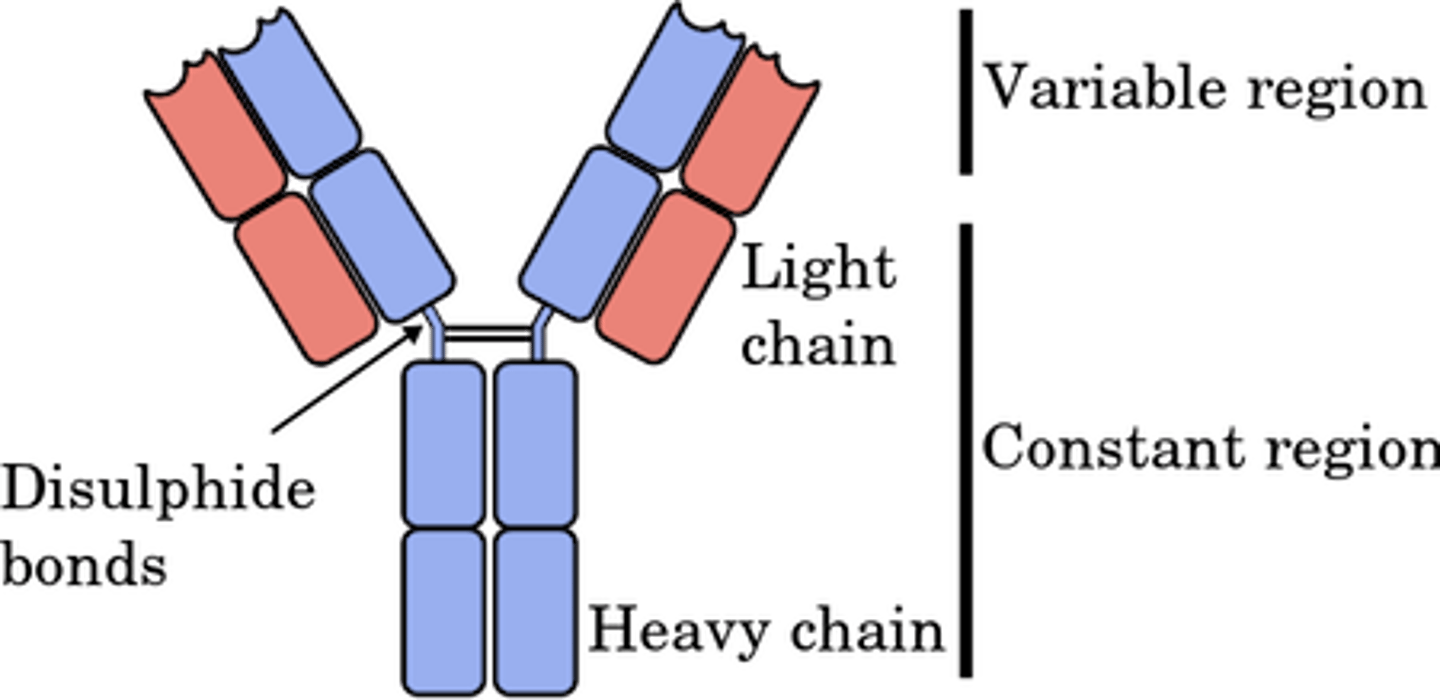
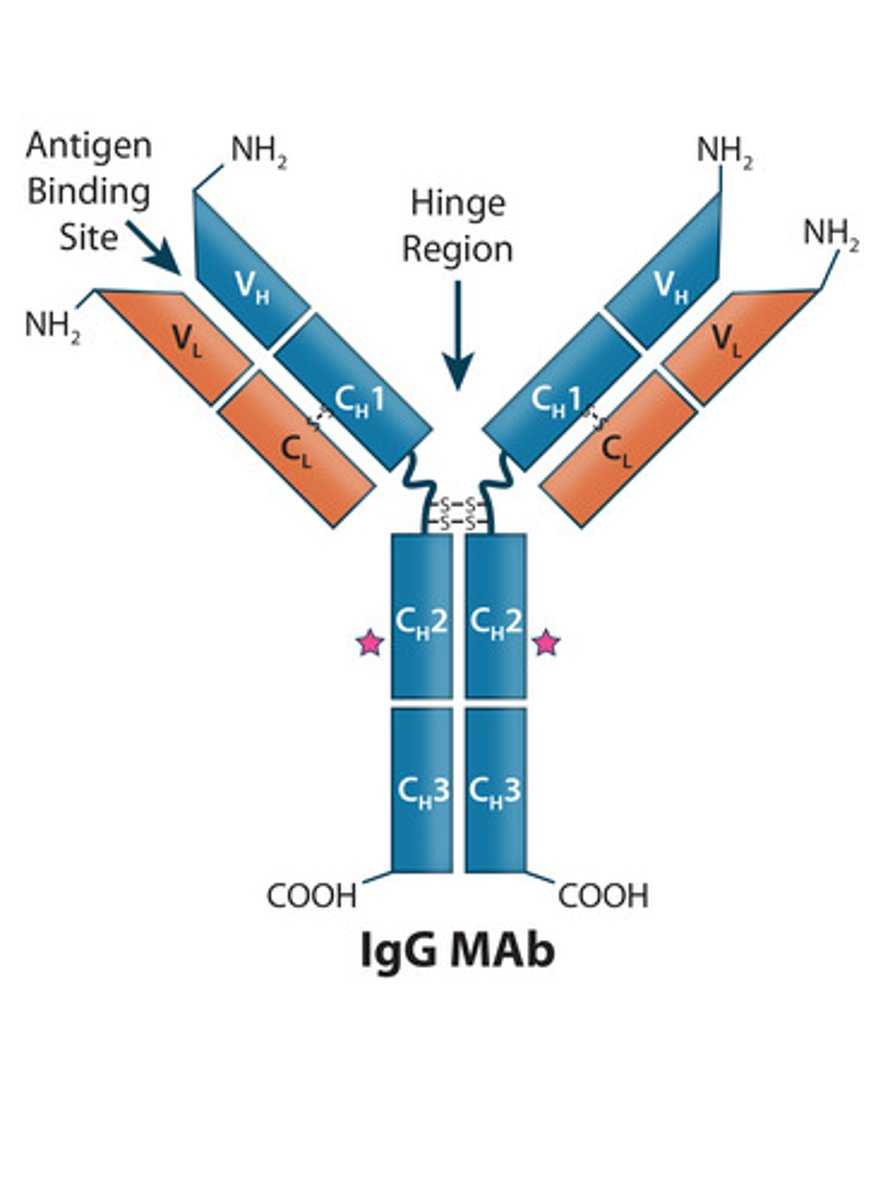
Antibody Structure
1. 4 looping polypeptide chains
-2 heavy
-2 light
2. Hinge region
3. Roughly T or Y shaped
4. Variable region at the ends of the H and L chains
5. Constant region
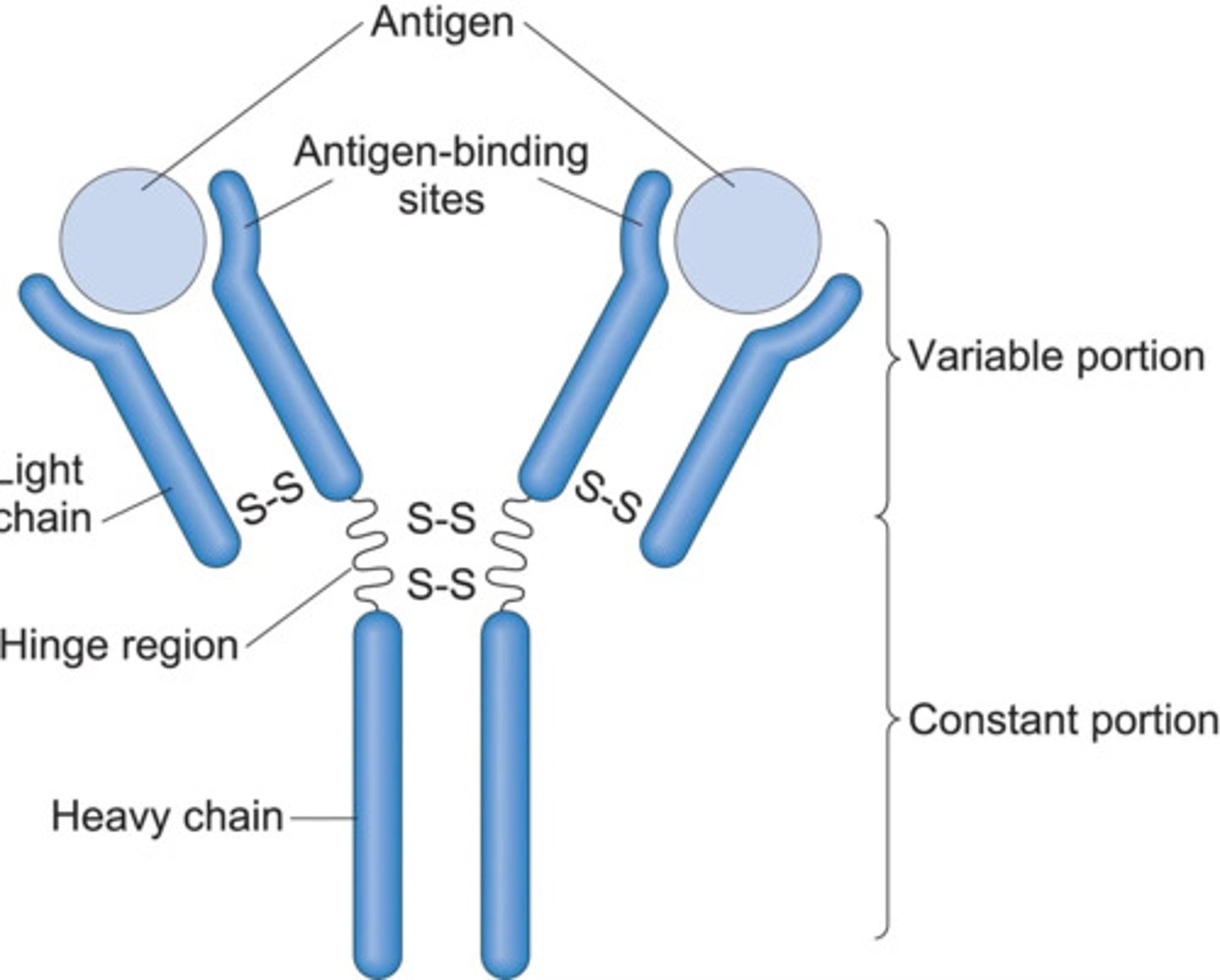
Looping polypeptide chains are linked together by
disulfide bonds
Heavy chains (H chains)
2 identical chains that are apart of an antibody made up of 400 amino acids individually
Light chains (L)
2 identical chains in the antibody and are about half the size of the heavy chains
Hinge region
is at the approximate middle where 2 disulfide bonds connect the 2 heavy chains. It provides flexibility to the molecule to allow two antigen-binding sites to function independently.
All four chains together form a molecule called a _________ ___________ that is roughly _____ or _______ shaped
antibody monomer, Y, T
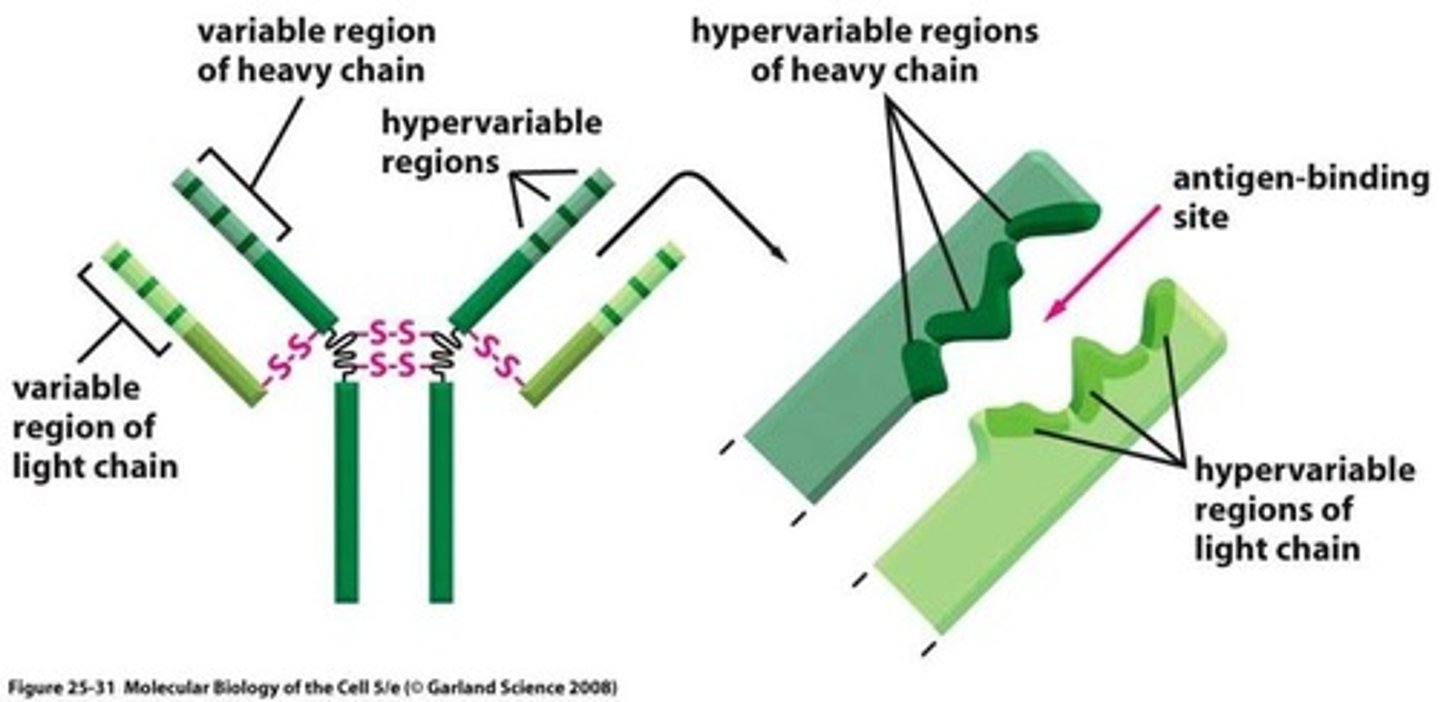
Variable region
The region at the end of the H and L chains of antibodies that varies from one antibody to another even within one class. This is the antigen binding site.
Constant regions form the _________ of the monomer and determine the _________ ___________.
stem, antibody class
Constant regions
the effector regions and dictate which cells and chemicals the antibody can bind to and how the antibody class will function in antigen elimination.
Antibodies can
fix complement, circulate in the blood, be found in body secretions, cross the placental barrier
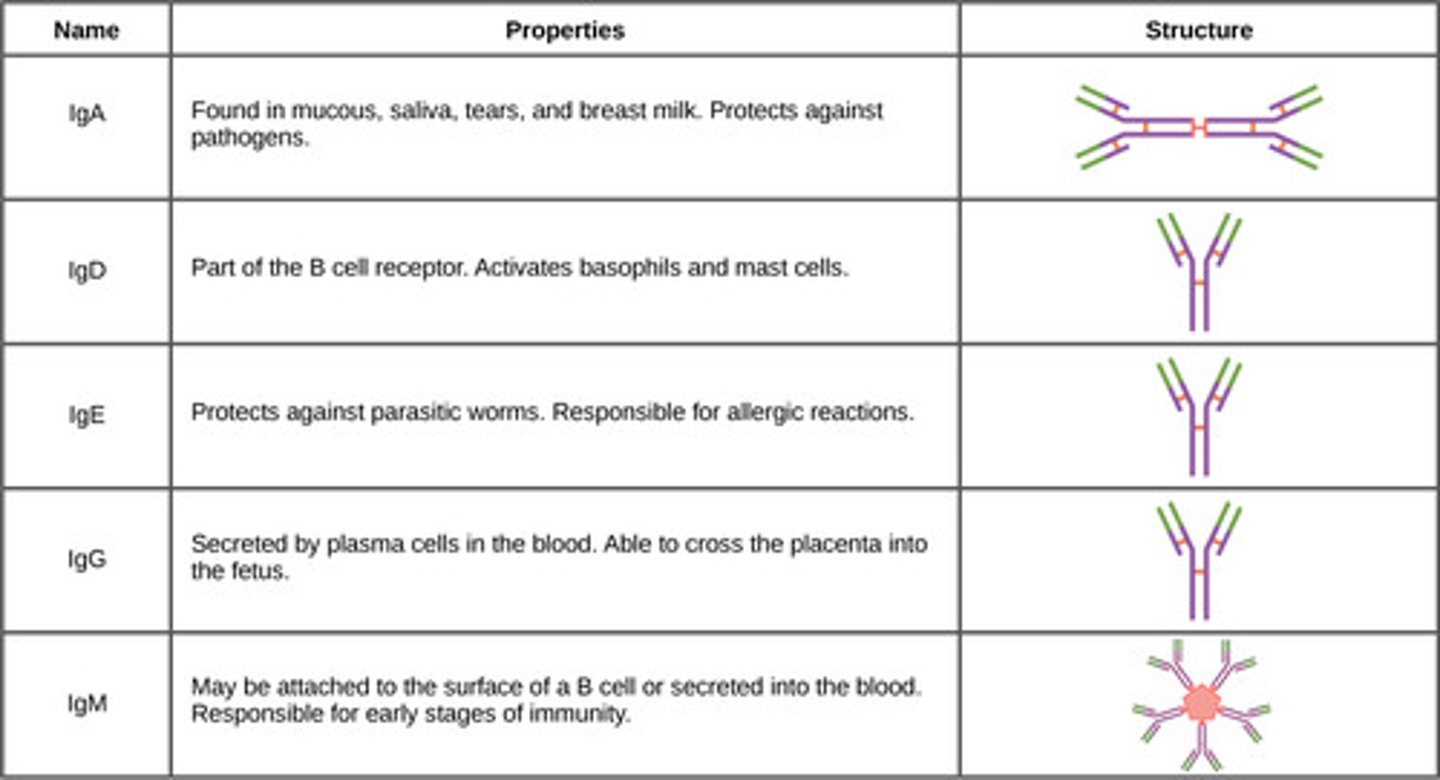
Antibody classes
IgG, IgA, IgM, IgE, IgD (GAMED)
Types of active immunity (Natural vs Artificial)
Natural- adaptive immune response
Artifical- vaccine immune response
Types of passive immune response (Natural vs Artificial)
Natural: trans-placental antibodies/breastfeeding
Artificial: Immune globulin injections
All antibody classes exist as monomers except
IgA- exists as dimer shape
IgD and monomer form of IgM act as
antigens on the surface of the B cells
IgM has 2 shapes
Monomer and Pentamer
IgD
exists as a monomer and is attached to the external surface of B cells where it functions an an antigen receptor and is important in B cell activation.
IgM
exists in monomer or pentamer forms
1. monomer attached to B cell surface and is an antigen receptor
2. pentamer circulates in the blood plasma and is released by plasma cells during the primary response. Acts as a potent agglutinating agent and readily fixes and activates complement.
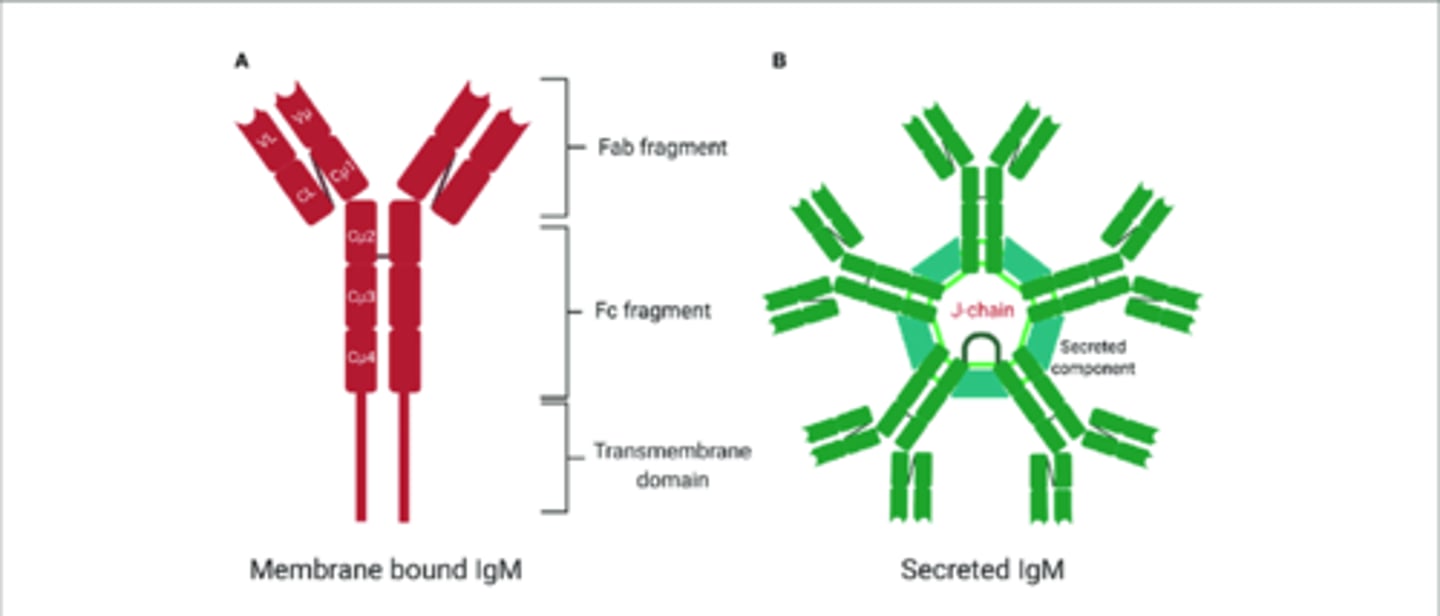
This immunoglubin's presence in the blood indicates current infection
IgM
Usually the first antibody released
Pentamer IgM
IgG
1. Exists as a monomer and is the most abundant and diverse antibody in plasma and accounts for 75-85% of circulating antibodies.
2. Can protect against bacteria, viruses, toxins and can fix complement.
3. It is the main antibody for both primary and secondary responses
Immunoglobin that is a potent agglutinator
IgM
IgM puts all the enemies
in one place and easier for it because they have 5 receptor sites.
IgM stimulates the
fixing and activating of a complement
The second antibody released is
IgG
IgG comprises ________ of antibodies
75-85%
IgG neutralizes
toxins, viruses and is also used in anti-venoms
IgA
1.A dimer in plasma and is also secretory because it is present in body secretions such as saliva, sweat, intestinal juice and breast milk.
2. It helps prevent pathogens from gaining access to the body.
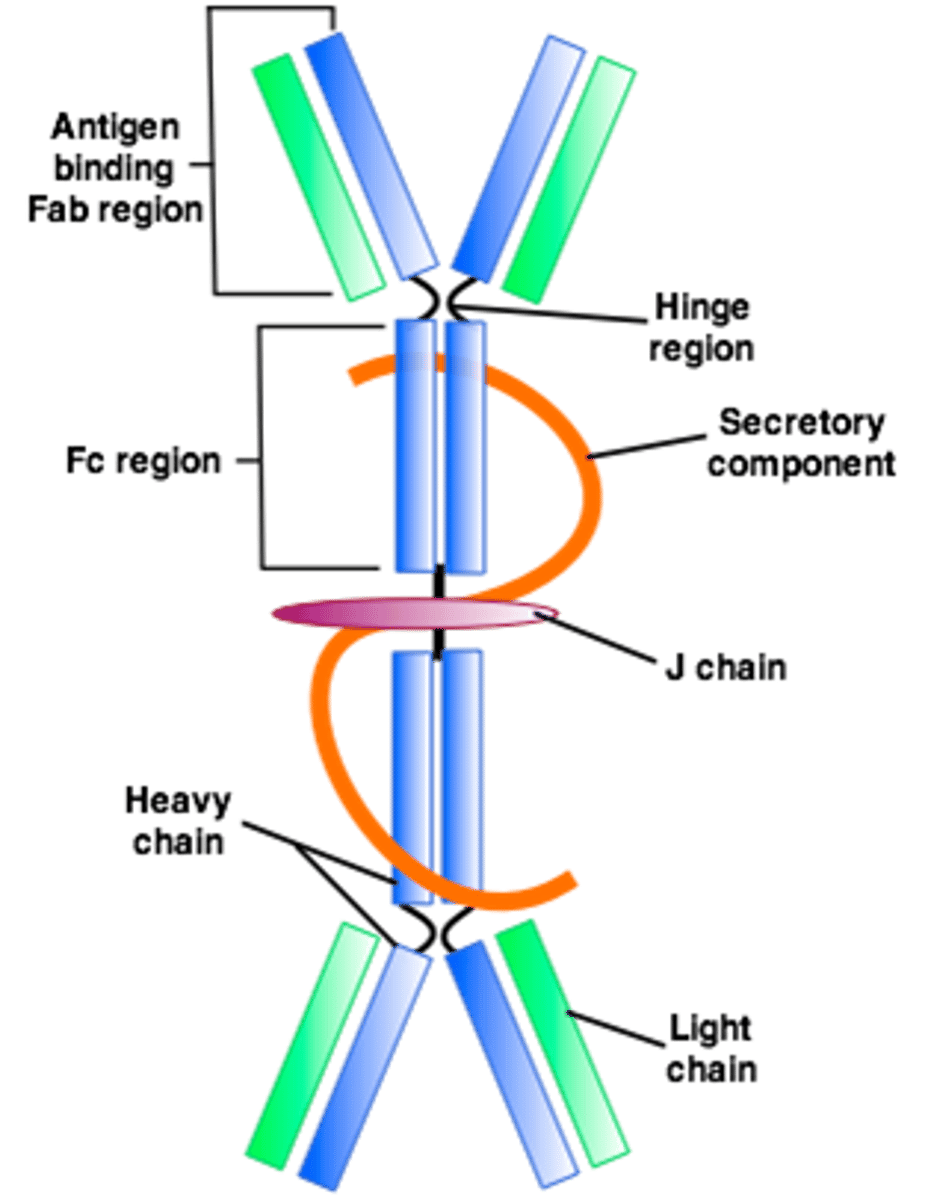
IgA enhances the
external innate defenses
IgE
1. A monomer that is secreted by the epithelial plasma cells and almost never found in the blood.
2. They bind to mast cells and basophils when activated by an antigen and it causes those cells to release hitamine and other chemicals that mediate inflammation and allergic reactions.
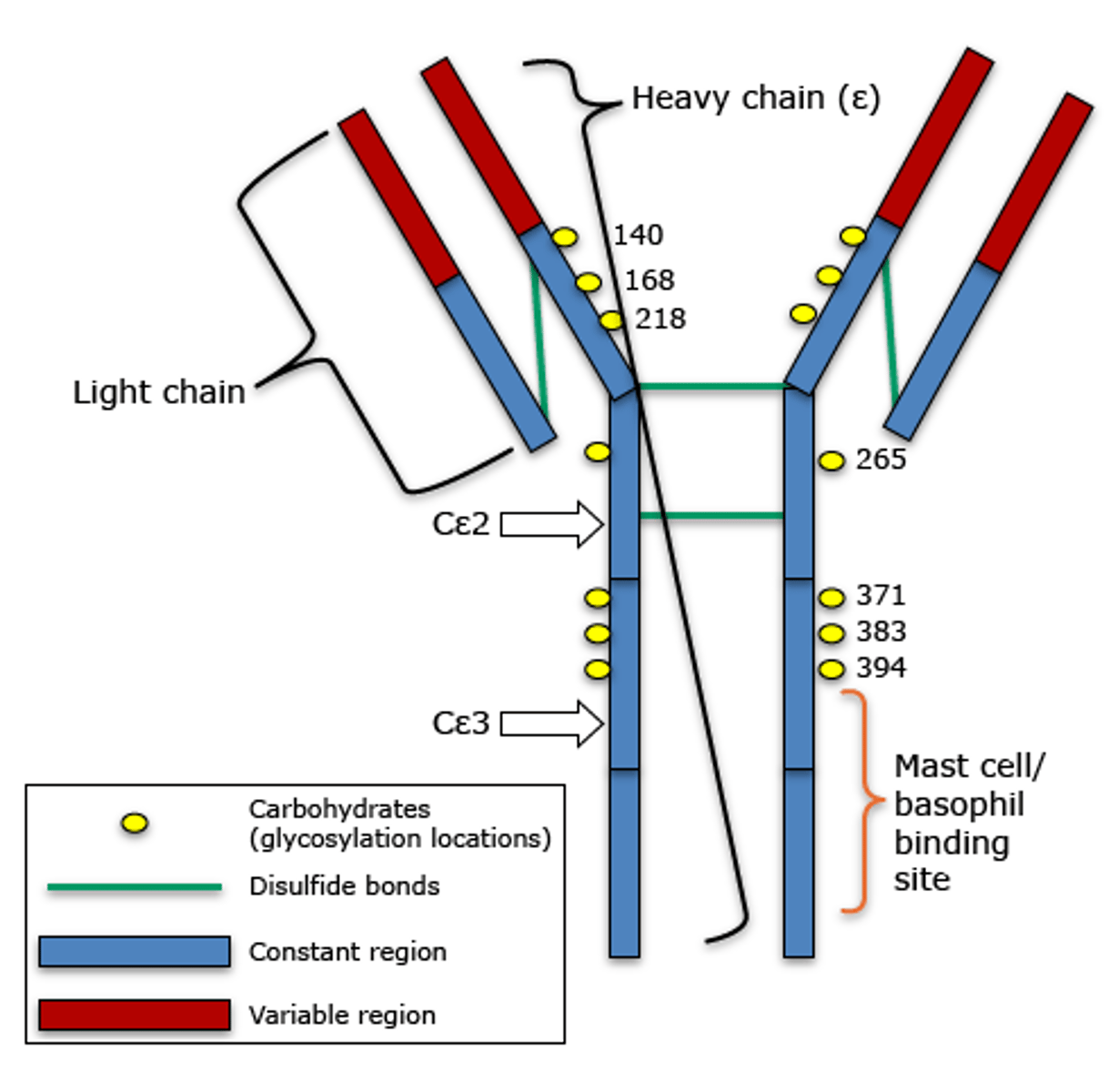
IgE activates
basophils and mast cells which release histamines and cause inflammation
Blood IgE levels rise dramatically during
allergic reactions or chronic gastrointestinal tract problems (never in the blood besides these cases)
What distinguishes one class of antibody from another?
Each antibody structure consists of two heavy chains and two light chains, which join to form a Y-shaped molecule. Each type of antibody has a different amino acid sequence at the tips of the "Y" which is why each antibody is shaped differently.
Antibody diversity
1. Somatic recombination
2. Hypervariable regions + Random mixes of H and L genes
3. Plasma cells can secrete 2 or more different antibody classes with the same antigen specificity
Somatic recombination
Plasma cells can make over a billion types of antibodies due to the reshuffling of gene segments.
Gene segments recombine as
B cells become immunocompetent and the newly assembled genes become expressed in the surface receptors of the B cells. B cells when activated become plasma cells which release the newly assembled genes as antibodies.
Hypervariable regions
domains on immunoglobulin heavy and light chains variable regions that are in direct contact with antigen and are frequently mutated to allow diverse antigenic specificities to be recognized
Primary response and antibody diversity
Starts with IgM release by a plasma cell followed by secretion IgG by the same plasma cell
Secondary responses consist almost entirely of _____ release
IgG
Defense mechanisms of antibodies
1. Complement fixation and activation
2. Neutralization
3. Agglutination
4. Precipitation
(C.f.a N.A.P) Calling for a NAP
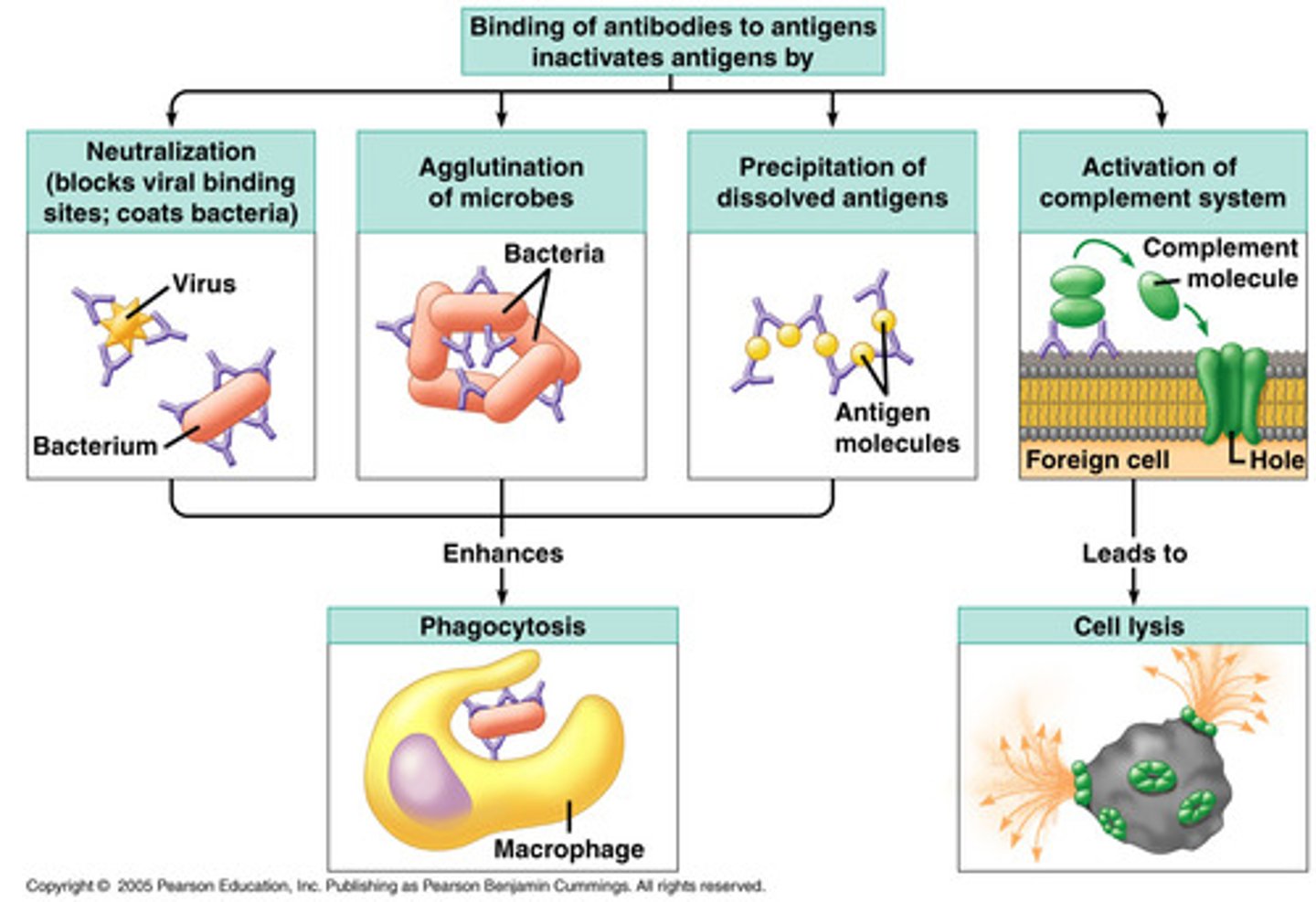
Complement and Activation
1. Chief weapon against cellular antigens
2. Antibodies bind to cells, change shape on constant regions and allow complement fixation onto the antigenic surface causing the cell to lyse.
3. Also starts a positive feedback loop enhancing inflammatory response and promoting phagocytosis via opsonization.
Antibodies inactivate
antigen-bearing invaders and tag them for destruction
A common event that takes place is the
antigen-antibody complex (immune complex)
Neutralization
Antibodies bind to specific sites on the main antigen, preventing them from binding to their cellular targets and causing injury.
Covering their binding sites so they can't attack their targets and make viral factors
Agglutination
cross-linking of many antigen-antibody complexes as to cause clumping
(Gather all the enemies, antigens and pathogens, together and limit their ability to spread. Also marked for cellular targets)
Precipitation
soluble molecules/antigens are cross-linked into large complexes and settle out of a solution where they are easily captured and consumed by phagocytes
If the antigen is a toxin and not a cell this is the defense used
(Take "bad" molecules out of the solution)
Antigen-antibody complex
The complex formed when multiple antibodies bind to multiple antigens. The bound antigen and antibody act as a unitary object.
What facilitates the removal of antigen-antibody complexes?
Complement fixation to immune complexes facilitates their removal by phagocytes. It also prevents deposits by facilitating their binding to erythrocytes, which transport immune complexes to the spleen and the liver where resident phagocytes such as macrophages dispose of them.
Monoclonal antibodies
commercially available pure antibody preparations specific for a single antigenic determinant produced by the descendants of a single cell.
(proteins made in a lab that bind to one antigen only)
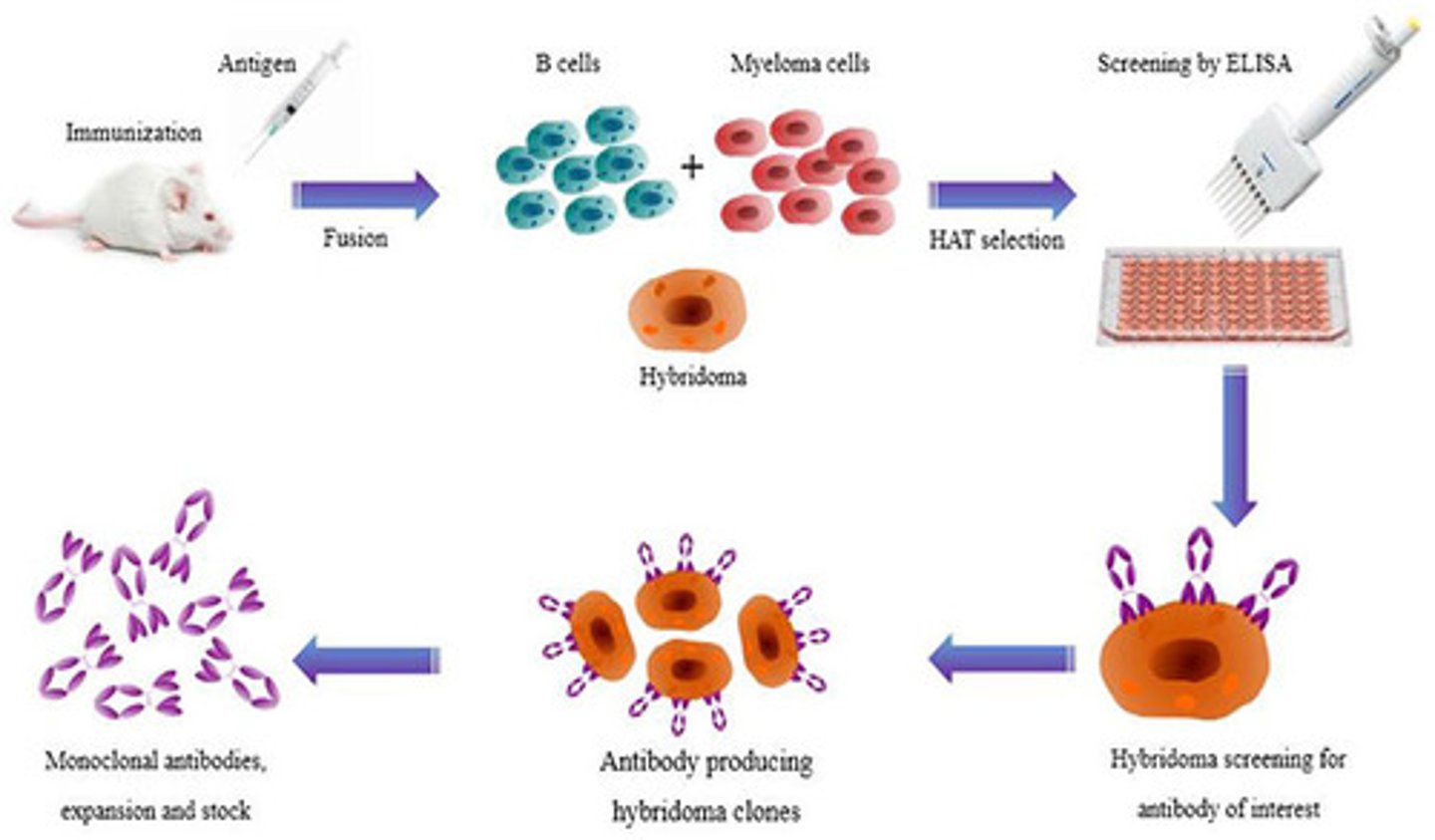
Monoclonal antibodies are made from
hybridomas
Hybridomas
are fusions of tumor cells (myeloma) and B lymphocytes. It has good characteristics of each such as the ability to proliferate indefinitely in culture (myeloma) and can produce a single type of antibody( B lymphocytes)
Monoclonal antibodies can be used to diagnose
pregnancy, some sexually transmitted diseases, some types of cancer, hepatitis, and rabies
Can treat leukemia and lymphomas by specifically delivering anticancer drugs.
monoclonal antibodies
Types of T cells
1. CD4 (T4 cells) (Helper T cells)
2. CD8 cell (T8 cells) (Cytolytic T cells)
3. Delayed hypersensitive T cells (Tdh)
4. Suppressor T cells (Ts)
5. Memory T cells
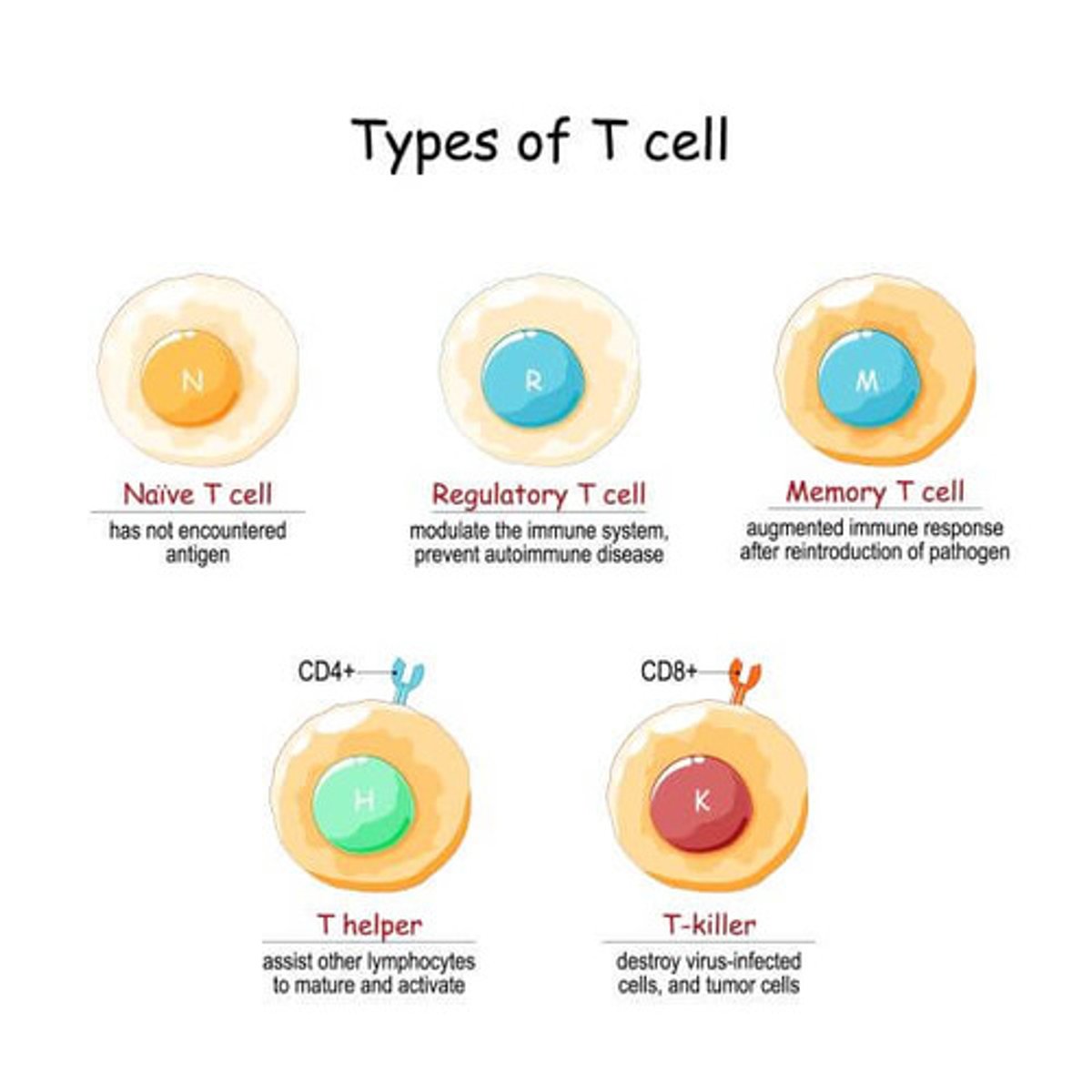
CD4
1. Primarily helper T cells (Th)
2. Have the glycoprotein CD4 cell surface receptors displayed
(all helper t cells have CD4 glycoproteins.)
CD8
1. Primarily cytolytic (cytotoxic) T cells (Tc)
2. Have the glycoprotein CD8 cell surface receptors displayed
(all cytotoxic cells have CD8)
Delayed Hypersensitive T cells (Tdh)
promote nonspecific killing by macrophages and is important in delayed hypersensitivity reactions like allergic contact dermatitis which follow skin contact with poison ivy and heavy metals.
Suppressor T cells (Ts)
stop activity of B and T cells once the infection has been conquered by secreting suppressor factors which suppress the immune response.
Memory T cells
These are similar to memory B cells in the fact that they are generated during the primary response and may exist in the body for years, allowing rapid response to subsequent reinfections of the same antigen.
T cells can recognize and respond only to
processed fragments of protein antigen displayed on the surface of cells
T cells are more effective at _______ ________ unlike antibodies, which cannot attack microorganisms that can quickly slip inside body cells and multiply like __________ _____________.
cell-cell interactions, tuberculosis bacillus
Th cells (Helper T cells)
1. Bind with specific antigens presented by an APC and stimulates production of other cells like Tc cells and B cells.
2. It can also act directly by secreting cytokines like interleukins 2, 4, and 5
3. Enhance the activity of Tc cells
Tc cells (Cytolytic T cells, Killer T cells, Cytotoxic, or CTL)
1. Activated by an antigen presented by any body cell and are recruited by Th cells.
2. Specialize in killing virus-invaded body cells and cancer cells.
3. Is involved involved with the rejection of foreign tissue grafts.
4. Secretes lymphotoxin and perforin
Lymphotoxin
causes DNA fragmentation and promotes inflammation
Perforin
causes cell lysis by creating large pores in the membrane of target cells
T cell cloning requires
"double recognition" such that immunocompetent T cells must be able to recognize the antigen and MHC protein
Class I MHC (process of binding to an antigen and presenting)
1. Class I MHC are made in the ER where endogenous antigens and foreign proteins are synthesized in a body cell from viral activity or cancerous cells.
2. The antigens are transported to the ER by special transport proteins called TAPs.
3. The antigen is then loaded onto the the Class I MHC protein where the complex (MHC + antigen) is incorporated into the plasma membrane
4. The complex is displayed and CD8 can recognize
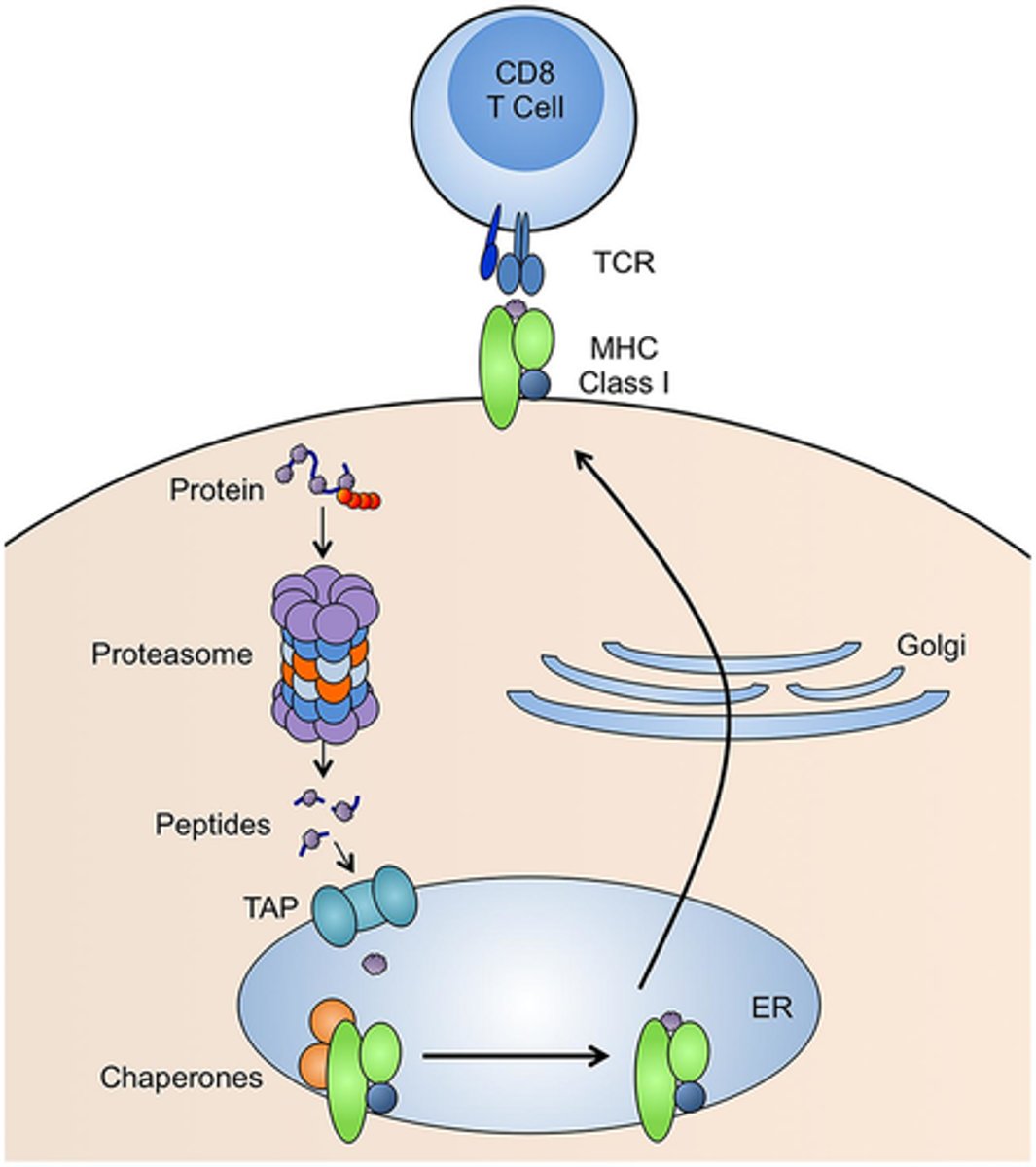
Class I MHC are
proteins that are displayed by all body cells except for red blood cells and are always recognized by CD8 T cells. If a cell is infected they will bind to the antigen and display this protein as well.
Class II MHC
proteins that are displayed on the surface of mature B cells, some T cells, and antigen-presenting cells, where they enable the cells of the immune system to recognize one another.
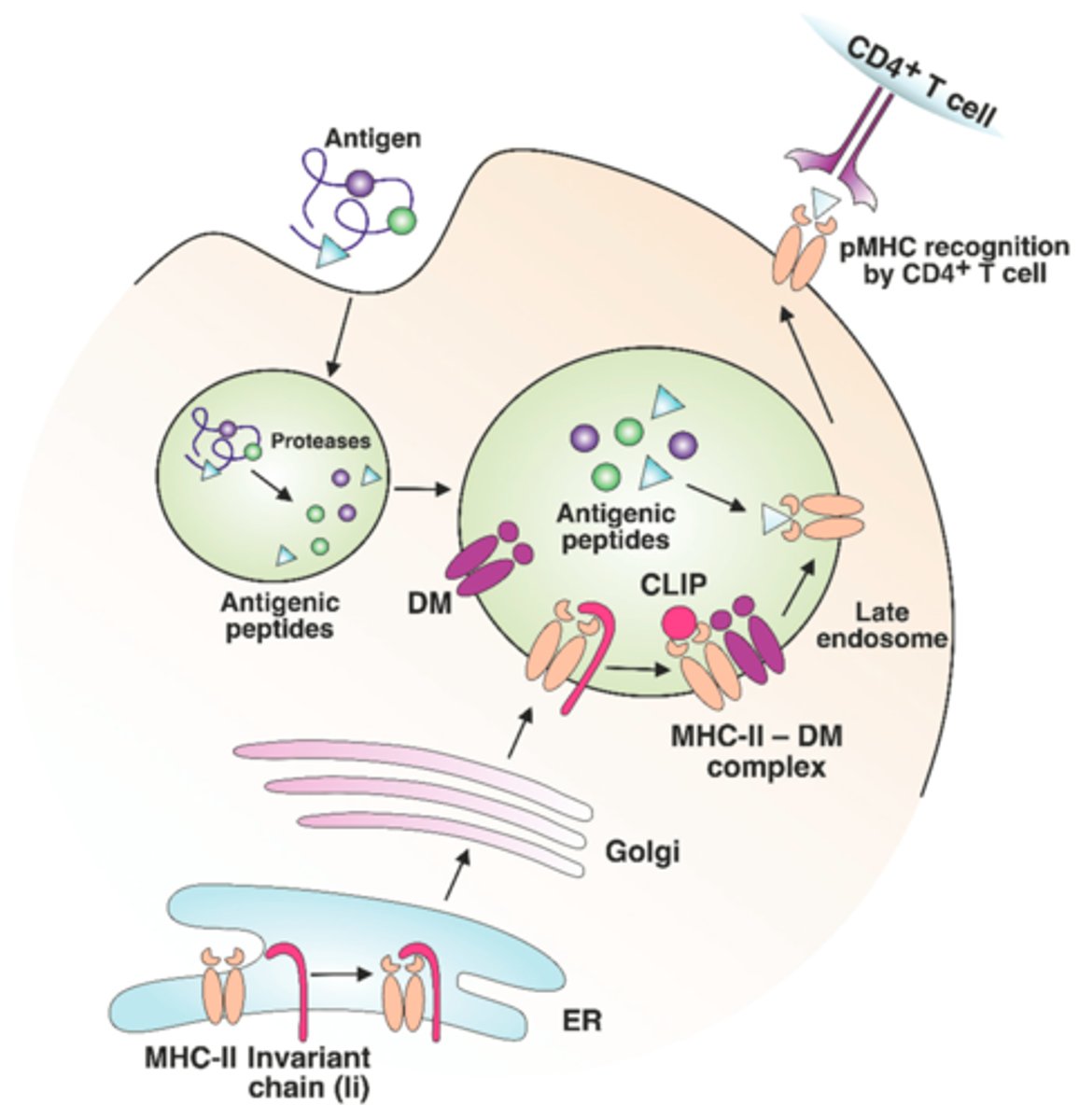
Class II MHC (process of antigen binding and presenting)
1. Synthesized in the ER but unlike MHC proteins they have an invariant chain attached which prevents MHC Class II binding to peptides in the ER.
2. the MHC Class II protein migrates to the phagolysosome where the invariant chain is removed.
3. Exogenous antigens are loaded onto the MHC Class II.
4. The loaded MHC Class II proteins are then displayed on the surface of the surface of the cell.
5. CD4 (T helper cells) can recognize them