2. Major Depressive Disorder
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
What are the symptoms of major depressive disorder?
depressed mood
reduced interest in pleasure
significant weight change
disturbed sleep
abnormal motor activity
fatigue
feelings of worthlessness/guilt
diminished ability to concentrate recurrent suicidal ideas
Looking at MDD symptoms, when can a diagnosis be made?
When 5+ of the behaviours are present
one of them has to be depressed mood or adehonia
What is the main treatment for MDD and when and how were they discovered?
SSRIs are main treatment
1987
accidentally discovered when researching TB
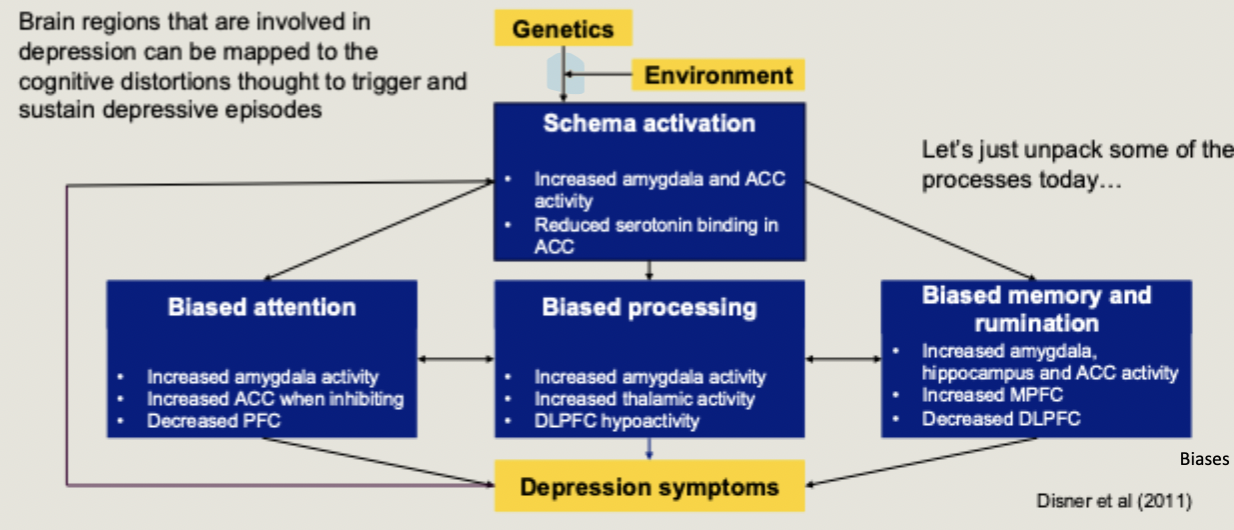
What are the 5 cognitive biases of depression outlined in Beck’s cognitive model?
depressive symptoms generated and maintained by a combination of maladaptive cognitions
biased attention towards negative stimuli
greater awareness/perception for negative stimuli (biased processing)
biased thought and rumination about depressive ideas
biased memory; recall depressive episodes with mire frequency
negative schemas about self and environment
How is a cognitive neuroscientific model of MDD generated
Brain regions that are involved in depression can be mapped to the cognitive distortions though to trigger and sustain depressive episodes
What is the Amygdala important for?
Recognition and generation of emotions
What is the difference in attentional bias between healthy and depressed people?
in healthy controls, attention is generally biased towards positive stimuli.
Individuals with depression instead show an attentional bias for negative stimuli
(more bottom up processing)
What could problems allocating attention lead to?
dysphoria: profound state of unease/ dissatisfaction
What are some brain regions associated with attention?
parts of the parietal cortex
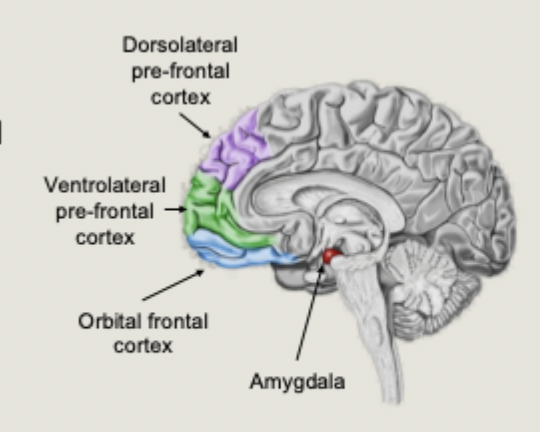
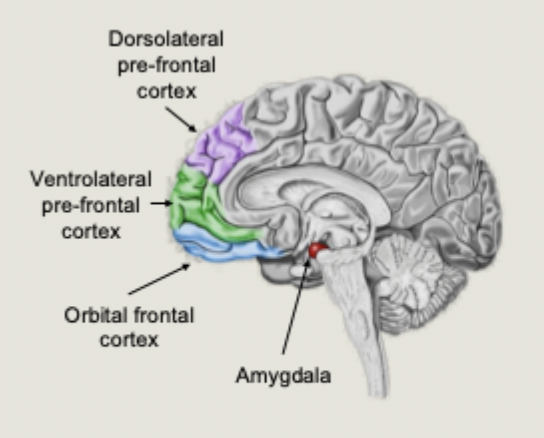
prefrontal cortex (PFC), including VLPFC and DLPFC
(more top down processing)
What did Siegle find using fMRI with unmedicated depression patients and healthy controls during two tasks:
A digit sorting task (cognitive)
a personal relevance ratings of words task (emotional)
patients with depression showed increase amygdala activity for negative words, and decreased DLPFC for both tasks
Negative emotional response is stronger, and less well regulated by top-down brain areas involved in attention allocation
Reward processing is affected in depression, how is reward in the brain supported?
supported by a fronto-striatal network: neural pathways that connect frontal lobe regions with the basal ganglia (striatum)
nucleus accumbens is part of the reward network - it is a major input to the striatum (basal ganglia)
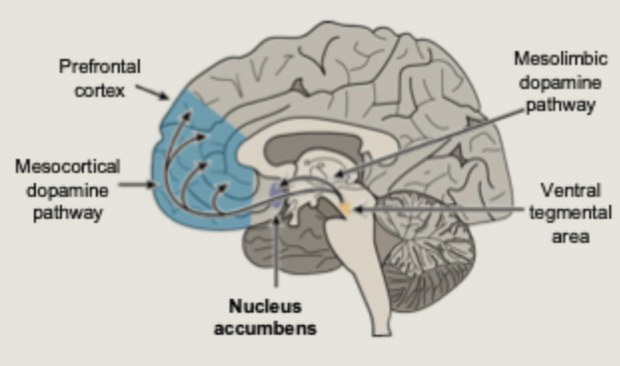
Disruption in which network has been argued to be the basis of adehonia?
The fronto-striatal reward network
What did Heller et al find about neural activation when asking depressed participants to either enhance or suppress emotional response to positive or negative images?
depression patients failed to sustain nucleus accumbens activation when amplifying, with deficits specific to positive emotion
patients who failed to sustain NAcc activity reported less intense positive emotion
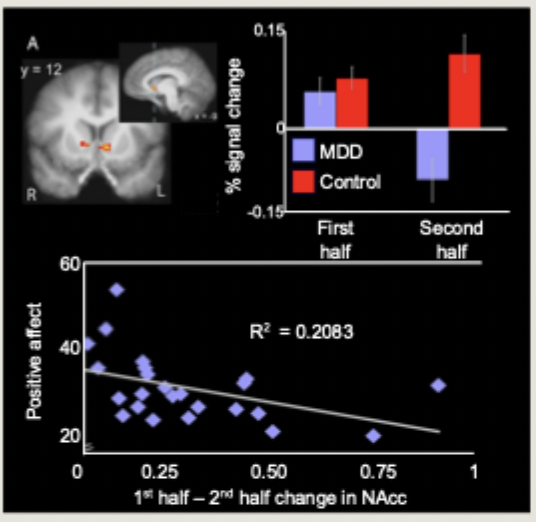
In Heller’s study of NAcc activation and enhancing emotions what was sustaining NAcc activation reflective of?
reduced prefrontal connectivity
What are the mechanisms of biased memory in depression?
Increased awareness for negative stimuli influences likelihood that negative information will be encoded and later recalled.
activity in the amygdala facilitates the encoding and retrieval of emotional stimuli in healthy individual by modulating brain regions associated with memory
biased memory in depression associated with amygdala hyperactivity, which is positively correlated with activity in the hippocampus
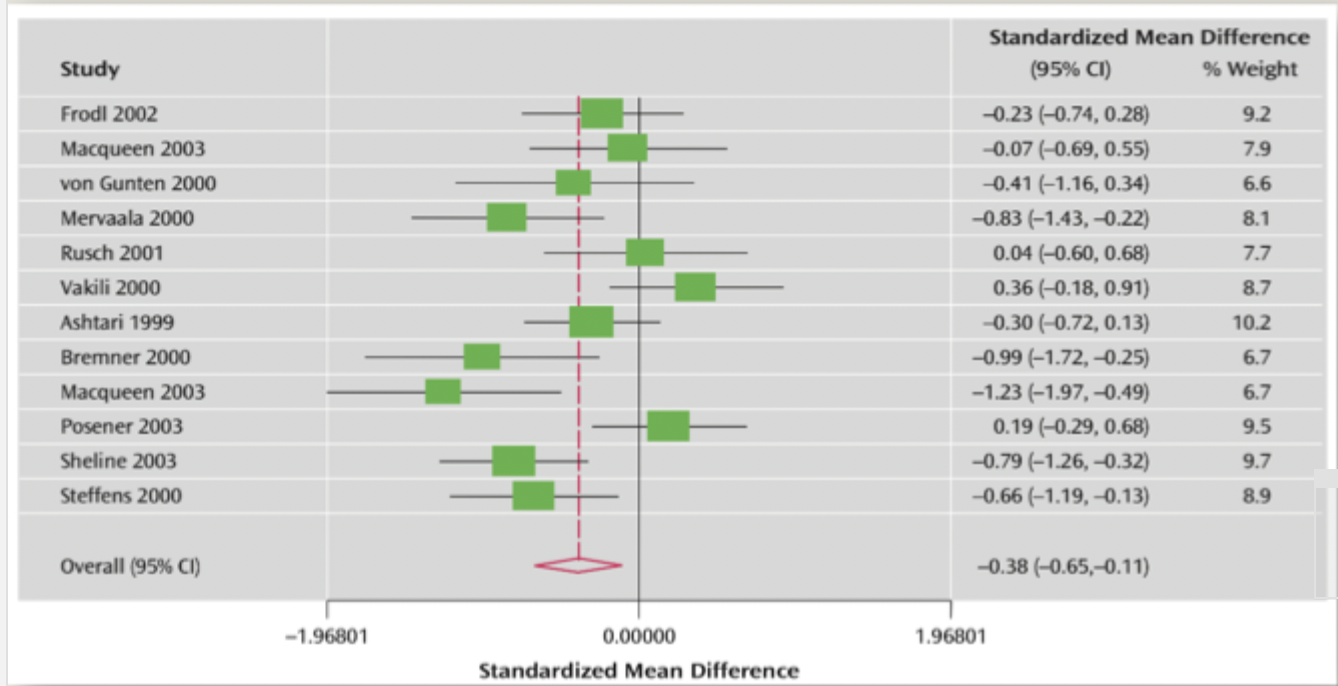
What does Videbech and Ravnkilde’s meta-analysis show about the hippocampus and depression?
hippocampal size in depression is smaller
What does human post-mortem data show decreased levels of in hippocampus of depressed patients and what effect does this cause?
decreased levels of BDNF (protein concentrated in hippocampus)
impairs memory encoding
demonstrates neuroplasticity at a very specific level
however, not clear if this is a cause or a result of depression
Which neurochemicals are implicated in depression?
cortisol
brain derived neurotropic factor (BDNF)
monoamines: dopamine, serotonin, noradrenaline
these chemicals can affect eachother
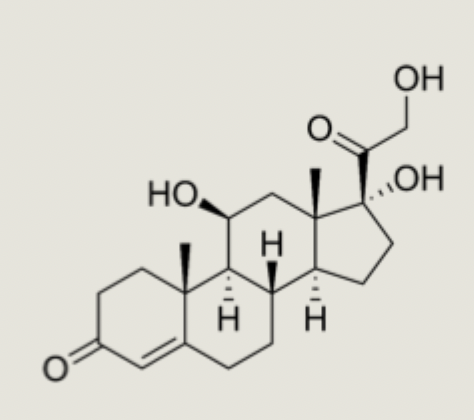
What are the effects of cortisol and how is it implicated in depression?
a steroid hormone, increases blood sugar, suppresses immune system, increases metabolism
increased cortisol raises performance during stress
people with depression may have elevated levels of cortisol
What is the function of Brain derived neurotrophic factor (BDNF)
maintains and supports growth of neurons/synapses
expressed in many brain areas but especially related to memory formation in the hippocampus
may lead to neuronal atrophy, impaired synaptic plasticity, and reduced ability to adapt to stress

What are monoamines?
Neurotransmitters, they are released by neurons to send signals to other neurons
What is the function of the monoamine dopamine and where is it released?
reward and motivation
released from ventral tegmental area to forebrain networks
What is the function of the monoamine serotonin and where is it released?
happiness molecule but also many complex behaviour (e.g. dominance)
released from Dorsal Raphe to forebrain networks
What is the function of the neurotransmitter Noradrenaline and where is it released?
“fight or flight” molecule that prepares the body for action
released to organs all over the body
When were monoamine treatments discovered?
Discovered in the 1950s, but not really any better understood today
How long does it take for monoamine treatments to be effective?
2-4 weeks, have to overcome homeostatic feedback mechanisms
instantaneous effect: placebo
What are two limitations of monoamine treatments?
Many different side effects (insomnia, restlessness, aggression, suicidal thoughts, dizziness, nausea, headaches)
effects can wash-out over time
How should monoamine treatments be administered?
Should not be a single treatment but as part of a treatment program
What is the monoamine theory of MDD?
in the healthy brain, monoamine neurotransmitters (e.g. serotonin) are released and bind to receptors on the postsynaptic neuron
transmission is terminated by re-uptake of the transmitter

How can MDD be treating using the monoamine theory of MDD?
Blockade of the re-uptake sites increases the concentration of monoamine neurotransmitters available at receptor sites and restores mood
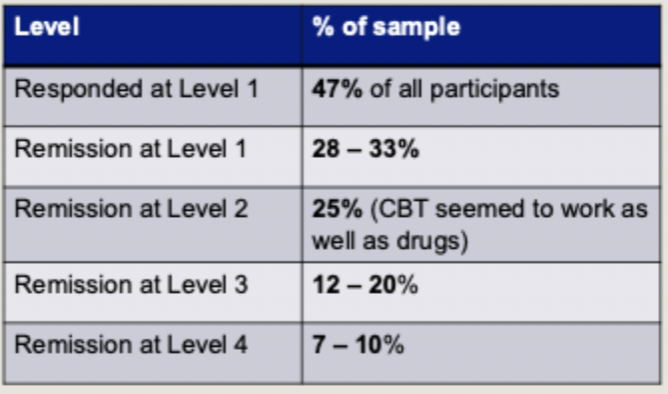
What were the 4 levels used in the STAR*D large-scale test of drug efficacy?
level 1: citalopram (SSRI for 14 weeks)
level 2: different antidepressant (SSRI) + optional CBT
level 3: different antidepressant + lithium or thyroid hormone
level 4: antidepressant + monoamine oxidase inhibitors (MAOI) or serotonin-norepinephine reuptake inhibitors (SNRI)
moved up level if ineffective
What were the results for the STAR*D test of drug efficacy?
approximately 70% of all participants who completed the treatment showed remission (no longer met criteria for MDD)
withdrawal rates increased at each level
some groups showed better responses (women, better educated, wealthier)
What did the CoBalT study find testing the efficacy of CBT?
usual care or usual care + CBT
monitored over 12 months
improvement seen in 46% of ppts in intervention group vs 22% in usual care (a signif diff p<.001)
What is the heritability of MDD?
MDD is highly heritable (50% chance if parent is diagnosed)
MDD is more heritable in women than men
we all have at least some of the genes that correlate with MDD
the extent to which we have genes that cause MDD varies
there is not one “depression gene”
How many base pairs are in the human genome?
3 billion
almost all identical across all humans
What are SNPs
single nucleotide polymorphisms
result in changes across individuals and groups
mapping these SNPs is much easier since the human genome project
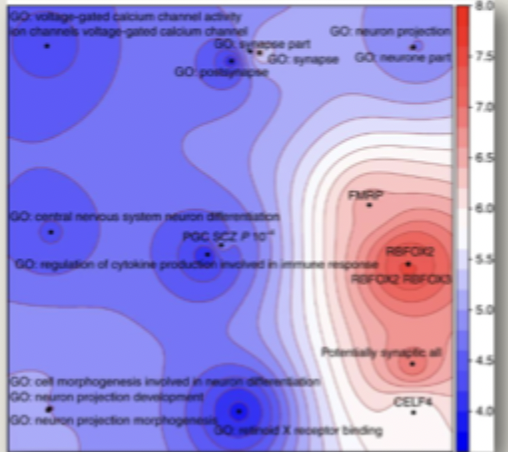
What did Wray et al (2018) find were some hot spot genetic location for MDD?
44 variants argued to map onto 19 genetic pathways to depression
weight and body size (OLFM4 and NEGR1)
neuron development and brain inflammation (LRFN5)
over-activation in fight or flight systems (RBFOX1)
neurotransmitter systems for dopamine (DRD2)
calcium signalling (CACNA1E and CACNA2D1)
glutamate neurotransmitter (GRIK5 and GRM5)
presynaptic vesicle trafficking (PCLO)
brain development (TCF4)
How can a road map and polygenic risk scores be used in MDD?
can be used to identify likelihood of developing depression
use polygenomic sequencing to compare an individuals DNA to the roadmap
estimate how likely one is to develop depression at some point in their life
What is the function of 5-HTT gene?
regulates the expression and transportation of serotonin in the brain
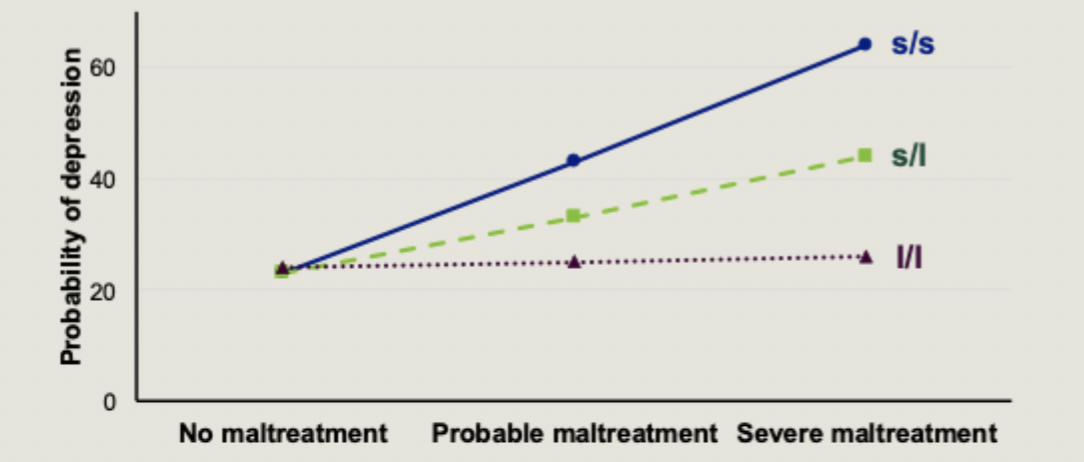
What are the versions of the 5-HTT gene?
two versions of the gene, a short (s) version and a long (l) version
so our three groups are: s/s, s/l, l/l
What did Caspi et al find looking at three groups of 5-HTT gene in combination with childrens’ exposure to stressful life events
the 5-HTT s/s homozygote allele variant is not enough to cause MDD
a combination of the 5-HTT s/s variant and early stressful life events will increase chances of a later MDD diagnosis
the risk of MDD is thus an output of both one’s genetic predisposition and one’s environment
What did Pezawas et al find in the brain structure of carriers of the s/s 5-HTT gene variant?
voxel brain morphometry used to measure grey matter volume of 5-HTT gene
carriers of the s/s variant show reduced volume in amygdala and perigenual cingulate
connectivity between amygdala and cingulate impaired when viewing fearful stimuli
What did Smeraldi et al find in their drug study of MDD patients with participants split according to 5-HTT genotype and treated with an SSRI
those with s/s genotype experience less improvement than those this l/l and s/l
genetics interacts not just with the environment but also treatment