5. small animal med- urinary tract infections
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
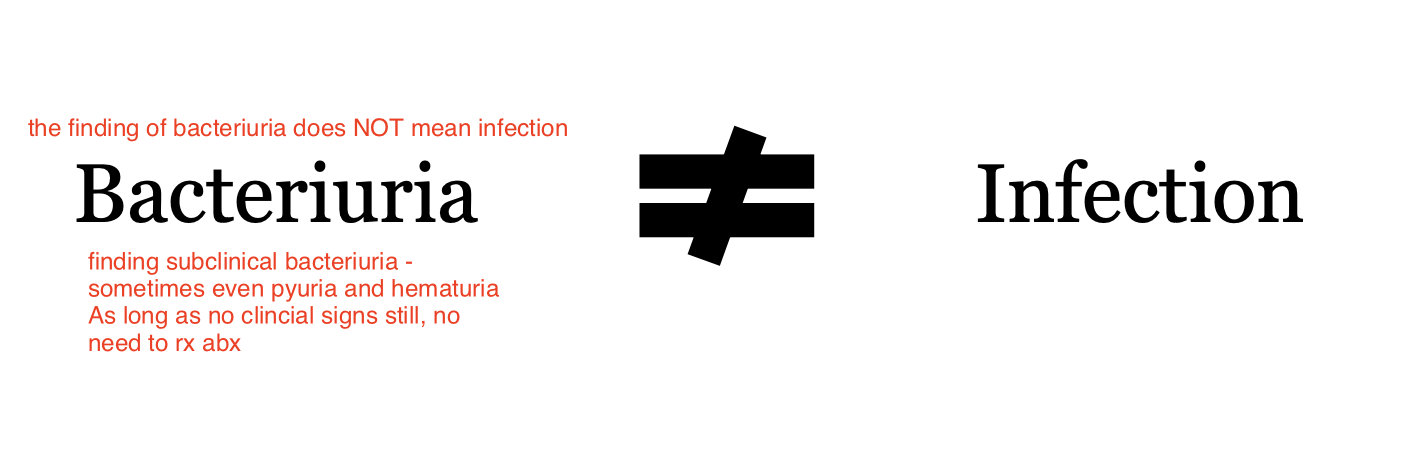
does presence of bacteria in the urine indicate infection?
no
which structures of the urinary tract are considered sterile environments?
kidneys, bladder, and proximal urethra are considered sterile
What are the categories of bacterial urinary tract diseases?
Lower UTI
sporadic bacterial cystitis
recurrent bacterial cystitis
bacterial prostatitis
Pyelonephritis
Subclinical bacteriuria
what is the prevalence of lower UTIs in dogs?
14% of dogs will have a UTI in their lifetime
spayed females and older dogs (>7 years) are at in increased risk
are UTIs more common in cats or dogs?
dogs
when are UTIs seen in cats?
RARE in cats 1-3%
usually in older cats with co-morbidity (CKD, hyperthyroidism, diabetes)
occurs in young cats who have had urinary catheterization or PU surgery
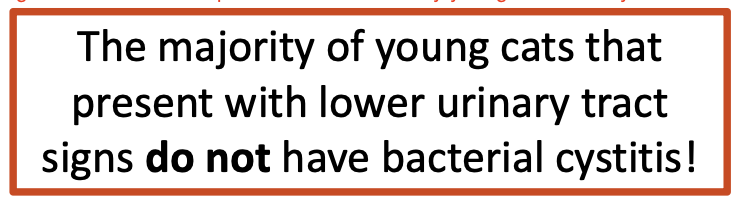
True or False? The majority of young cats that present with lower urinary tract signs usually have bacterial cystitis.
False. These cats likely have either stones or FIC (feline idiopathic cystitis)
what are the lower urinary tract clinical signs?
-stranguria
-pollakiuria (frequent urination in small amts)
-periuria (urinating in inappropriate places)
-hematuria
-licking at urethral opening
what is the most common bacterial uropathogen?
E. coli
(75% or more bacterial infections is E. coli)
what is the definition of sporadic bacterial cystitis?
bacterial infection of the bladder with LUT signs
fewer than 3 episodes in the preceding year
which animals is sporadic bacterial cystitis seen in?
usually healthy pets (non-pregnant females, neutered males)
also animals with no urinary tract anatomical and functional abnormality or relevant comorbidities
how is sporadic bacterial cystitis diagnosed?
1. presence of LUT signs with evidence of cystitis (hematuria, pyuria, bacteria) on urinalysis
2. urinalysis performed in all cases to screen for cystitis
3. aerobic culture preferred (via cystocentesis) in dogs (perform in all cats to confirm true infection)
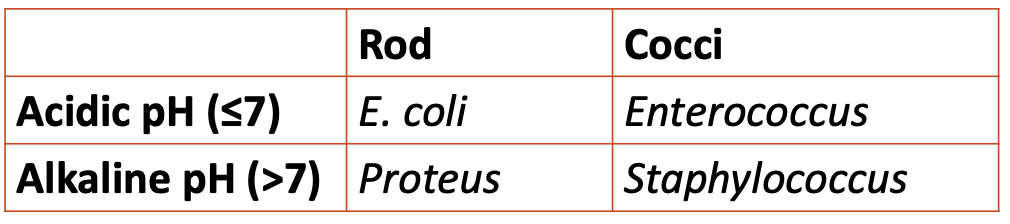
A best guess of bacterial species is based on what factors on UA?
pH and morphology
If you see bacteriuria what else should you look for?
Evidence of co-morbidity (USG - kidney disease?, glucose - DM?, abnormal cells - Cancer?)
how are antibiotics chosen for treatment of sporadic bacterial cystitis?
-guided by suspected bacterial species on urinalysis
-guided by culture and sensitivity, if available
-choose weaker and safer drug
what does it mean to choose a 'weaker' antibiotic?
weaker drugs= noncombination drugs, earlier generation drugs
what does it mean to chose the 'safer' antibiotic?
drugs with wide margin of tolerance, low risk of systemic effects
what is the likely uropathogen causing bacterial cystitis with an acidic pH (at or below 7) and rod bacteria?
e. coli
(most common isolate, often susceptible to beta-lactams and fluoroquinolones)
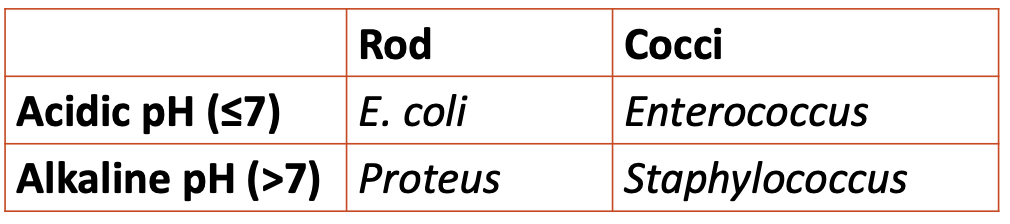
what is the likely uropathogen causing bacterial cystitis with an acidic pH (at or below 7) and cocci bacteria?
enterococcus spp.
(low pathogenicity, common with subclinical bacteriuria, intrinsically resistant to cephalosporins)
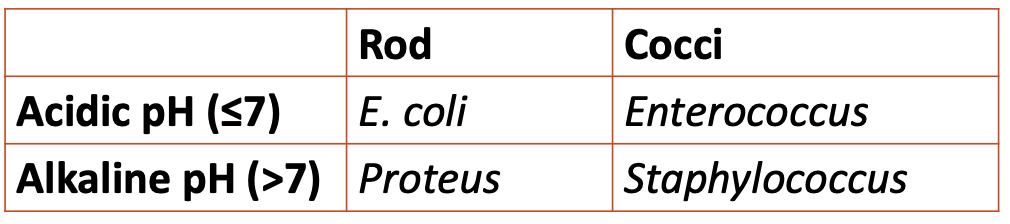
what is the likely uropathogen causing bacterial cystitis with an alkaline pH (above 7) and rod bacteria?
proteus spp
(urease-producing bacteria, promote formation of struvite stones)
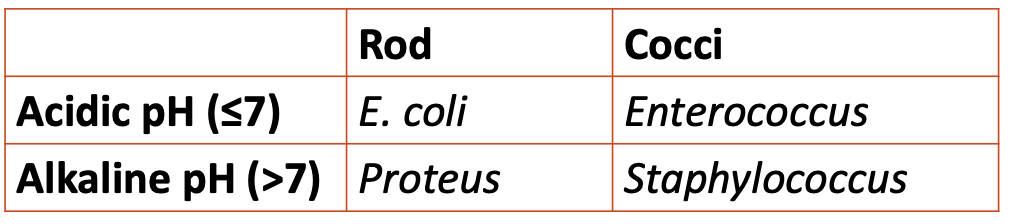
what is the likely uropathogen causing bacterial cystitis with an alkaline pH (above 7) and cocci bacteria?
staphylococcus spp
(urease-producing bacteria, promote formation of struvite stones)
when is empirical antibiotic therapy in lieu of culture justified for treatment of sporadic bacterial cystitis?
justified if:
-limited previous antimicrobial exposure
-no treatment of UTI in past 3 months
what are the empirical antibiotic choices for sporadic bacterial cystitis?
amoxicillin, TMS
second line: fluoroquinolones, 3rd gen cephalosporins
What abx is not first-line choice for empirical abx treatment of sporadic bacterial cystitis?
DO NOT USE CLAVAMOX
what is the duration of antibiotic therapy for sporadic bacterial cystitis?
5 days
For sporadic bacterical cystitis consider what additional medication pending urine culture?
2-3d of NSAID
how should patients with sporadic bacterial cystitis be monitored?
-monitor for resolution of clinical signs
-post-treatment UA and urine culture not required if clinical resolution of LUT signs
when is further investigation warranted when monitoring the treatment of sporadic bacterial cystitis?
-lack of clinical response within 48 hours of starting antibiotic
-relapse of clinical signs shortly after discontinuation of antibiotics
what is the definition of recurrent bacterial cystitis?
diagnosis of 3 or more episodes of clinical bacterial cystitis in the preceding 12 months or 2 or more episodes in the preceding 6 months
what is recurrent bacterial cystitis the result of?
result of relapsing or persistent infection or reinfection
Look for predisposing factors
how are relapsing/persistent infections and reinfections differentiated in cases of recurrent bacterial cystitis?
if isolate is different from previous organism isolated→ reinfection
if isolate is same organism with the same susceptibility pattern→ relapse or persistent infection
what are risk factors and comorbidities that predispose dogs and cats to UTIs?
-endocrinopathy
-kidney disease
-obesity
-abnormal vulvar conformation
-congenital abnormalities of urogenital tract
-prostatic disease
-bladder tumor
-polyploid cystitis (benign polyp-like inflammatory masses)
-urolithiasis
-immunosuppressive therapy
-rectal fistula
-urinary incontinence/retention
SPOOKI CUB RAP
stones, prostatic dz, obesity, obstructions, kidney disease, immunosuppresive
congenital, urinary incontinence, bladder tumor
rectal fistula, abnormal vulvar conformation, polypoid cystitis
what does the work-up exam include for patients with recurrent bacterial cystitis?
-genital exam
-chemistry panel
-UA and culture
-radiographs
-ultrasound
-refer for cystoscopy
what is the treatment for recurrent bacterial cystitis?
-review prev abx use and susceptibility pattern (compliance? duration? dose?)
-give NSAID and/or empirical abx pending urine culture
-avoid repeat use of abx that the pet has not fully responded to in the past
-reassess once you get C&S results
-treat with chosen antibiotics for 7-10 days
what are the treatment goals of recurrent bacterial cystitis?
clinical cure with minimal risk of adverse effects of antibiotic
microbiologic cure is desirable but not always possible
what are current thoughts on cranberry extract?
thought to reduce adherence of E. coli uropathogens BUT not enough data in vet med to support its use ☹
which animals is bacterial prostatitis most commonly seen in?
male intact dogs
what are the common etiological agents of bacterial prostatitis?
similar bacteria as found in bacterial cystitis
brucella canis is a zoonotic cause of prostatitis (reportable in OR)
what are clinical signs of bacterial prostatitis?
same as bacterial cystitis, plus:
-fever
-malaise
-inappetence, vomiting, diarrhea, tenesmus
-septic shock
how is prostatitis diagnosed?
-per rectum palpation of prostate (very painful typically)
-CBC/chem/UA/urine culture
- +/- ultrasound to assess size and structure of prostate
- +/- cytology of prostatic wash or prostatic fluid collection by FNA
what is the challenge of treating prostatitis with antibiotics?
the blood prostate barrier limits penetration of antimicrobials, especially in chronic prostatitis when the barrier may be less compromised
what antibiotics are used to treat bacterial prostatitis?
lipid soluble antibiotics:
-first line or empiric therapy: fluoroquinolone e.g. enrofloxacin (except ciprofloxacin)
-second line: clindamycin or macrolides
how long is antibiotic therapy for bacterial prostatitis?
4 weeks
which antibiotics should be avoided for treatment of bacterial prostatitis?
amoxicillin, cephalosporins, aminoglycosides, tetracyclines (these dont cross blood prostate barrier)
and ciprofloxacin
AACCT
besides antibiotics, what are other treatments for prostatitis?
-castration (if breeding, consider finasteride - shrinks prostate)
-MUST drain prostatic abscess (sx or u/s guided percutaneous drainage)
what is the definition of pyelonephritis?
infection of renal parenchyma that occurs from ascending infection (more commonly) or bacteremia due to animal being septic
what is the most common pathogen isolated from pyelonephritis?
e. coli
what are clinical signs of pyelonephritis?
systemic signs of illness and renal pain
what lab abnormalities are seen with pyelonephritis?
-bacteriuria, pyuria, hematuria
-inflammatory leukogram
-azotemia
-glucosuria, proteinuria, cellular casts (tubular epithelial, RBC, WBC)
how is pyelonephritis diagnosed?
difficult to prove diagnosis without renal biopsy or pyelocentesis
a presumptive diagnosis is made based on systemic signs, positive urine culture, and azotemia
In an AKI or acute on chronic kidney disease, what should you ALWAYS perform?
urine culture (screen for pyelonephritis!)
why should you always perform a urine culture in AKIs or acute on chronic kidney disease?
to screen for potential pyelonephritis
culture even if quiet urine sediment or no LUT signs present
± blood culture if febrile!
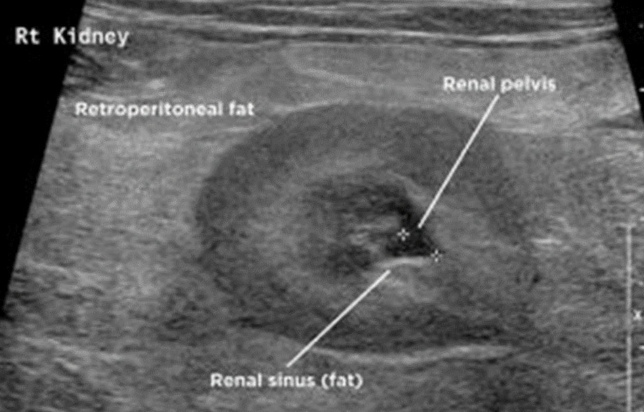
what abnormalities may be seen on ultrasound in patients with pyelonephritis?
U/S findings are nonspecific:
-renal pelvic dilation (+/- echogenic fluid - suggestive of pus)
-dilated ureter
-blunting of renal papilla
-hyperechoic retroperitoneal fat around kidney
how is pyelonephritis treated?
-start tx ASAP while awaiting culture results
-treat for AKI (IV fluids, monitor UOP)
-antibiotics for 14 days
which antibiotics are used for treatment of pyelonephritis?
-fluoroquinolone (oral and injectable)
-cefpodoxime (oral)
-ceftazidime or cefotaxime (injectable)
FCC
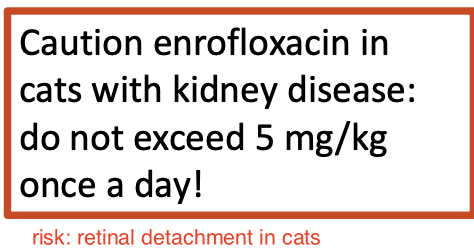
why should you use enrofloxacin with caution in cats with kidney disease?
do not exceed 5mg/kg once a day
cats w/ kidney disease may have reduced renal excretion of drug, so can accumulate and cause toxicity
what other differentials should be considered if there is no improvement in systemic signs/hematology/azotemia within 72 hours of antibiotic therapy for treatment of pyelonephritis?
-subclinical bacteriuria?
-renal neoplasia
-ureterolith
-ischemic injury
-lepto (dogs)
LINUS
how are patients treated for pyelonephritis monitored?
recheck chem, UA, and urine culture 1-2 weeks after cessation of antibiotics
what is the definition of subclinical bacteriuria?
presence of bacteria in urine in the absence of clinical evidence of infectious disease (ie no LUT or signs or AKI)
which animals is subclinical bacteriuria seen in?
occurs in both healthy pets (dogs > cats) and those with disease (diabetes, immunosuppression, CKD)
what are the most common isolates of subclinical bacteriuria?
enterococcus spp > e. coli
should you treat animals with subclinical bacteriuria?
tx is discouraged for these animals, there is no evidence that tx improves outcome
tx also contributes to abx resistance and recolonization often follows abx tx
Identifying __ of cystitits may be challenging (unobservant Os, cats, pets w/ paresis or paralysis) so need to use clinical judgement and look at each case individually.
clinical signs
Ask yourself: What is the bacteria? What is the susceptibility profile? Evidence of pyelonephritis? Can O reliably detect clinical signs? At risk of struvite uroliths? Urine pH?
how should animals with subclinical bacteriuria be monitored?
if no tx indicated (as in most cases), ask owner to monitor for LUT signs (if LUT signs develop, recheck UA and urine culture)
recheck in 3-6 months in pets with comorbidities