SEM 2 - MSK UQ (WK 1-8)
1/268
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
269 Terms
Recognize prognostic indicators of neck pain
Severity and irritability of symptoms: higher pain and easy provocation → slower recovery
Duration/stage of symptoms: acute (<7–10 days), subacute (10 days–7 weeks), chronic (>7 weeks)
Functional limitations: reduced ROM, impaired ADLs, work limitations
Previous episodes: recurrent neck pain predicts future episodes
Psychosocial factors: anxiety, depression, catastrophizing, low self-efficacy
Red flags or neurological signs: numbness, weakness, or signs of myelopathy → may worsen prognosis
Identify risk factors associated with neck pain
Intrinsic factors (patient-related):
Age (middle-aged adults higher risk)
Female sex (higher prevalence)
Poor posture, weak cervical/upper thoracic muscles
History of trauma or prior neck pain
Extrinsic factors (environmental/behavioral):
Sedentary lifestyle, prolonged computer or phone use
Heavy lifting or repetitive overhead work
Psychosocial stressors at work or home
Smoking and poor general health
Basic bony anatomy of the cervical region
Vertebrae C1–C7: small bodies, large vertebral foramen
Atlas (C1): supports skull, no body, allows nodding (flexion/extension)
Axis (C2): dens (odontoid process) allows rotation
Facets: superior and inferior articular processes → guide motion and resist shear
Transverse processes: contain foramen for vertebral arteries
Spinous processes: attachment for ligaments and muscles
Ligamentous anatomy of cervical region
Anterior longitudinal ligament (ALL): prevents excessive extension
Posterior longitudinal ligament (PLL): prevents excessive flexion, guides disc motion
Ligamentum flavum: connects laminae, maintains tension in neutral posture
Interspinous & supraspinous ligaments: resist excessive flexion
Capsular ligaments of facets: stabilize facet joints during motion
Contribution to cervical stability (facets, joints, IVD, ligaments)
Facets: resist rotation and shear, guide flexion/extension
Intervertebral discs: absorb load, allow controlled motion, prevent vertebrae from collapsing
Joint capsules: limit excessive translation, resist sudden motion
Ligaments: provide passive tension to maintain alignment, protect spinal cord and nerve roots
Basic muscular anatomy of the cervical spine
Superficial muscles (movement & posture):
Deep cervical flexors (stability & fine control):
Deep cervical extensors (segmental control & posture):
Suboccipital muscles (fine movement & proprioception):
Superficial muscles (movement & posture):
Trapezius (upper fibers): elevates scapula, assists neck extension and side bending
Sternocleidomastoid (SCM):
Bilateral contraction → cervical flexion
Unilateral contraction → ipsilateral side bending, contralateral rotation
Levator scapulae: elevates scapula, assists in ipsilateral neck side bending and rotation
Deep cervical flexors (stability & fine control):
Longus colli & longus capitis: maintain cervical lordosis, prevent excessive anterior translation, control segmental flexion
Rectus capitis anterior & lateralis: assist with upper cervical stabilization and flexion
Deep cervical extensors (segmental control & posture):
Semispinalis cervicis & capitis: extend cervical spine, control rotation
Multifidi: stabilize individual segments, resist excessive shear
Splenius cervicis & capitis: extend and rotate the neck ipsilaterally
Suboccipital muscles (fine movement & proprioception):
Rectus capitis posterior major/minor, obliquus capitis superior/inferior:
Control small movements of the atlanto-occipital (AO) and atlanto-axial (AA) joints
Provide proprioceptive feedback
Contribution of cervical muscles to stability and mobility
Stability:
Deep flexors and extensors maintain segmental alignment and prevent excessive shear or translation
Multifidi and deep neck muscles provide dynamic stabilization during motion
Muscles counteract gravitational forces and help maintain neutral posture
Mobility:
Superficial muscles (SCM, splenius, trapezius, levator scapulae) produce larger movements like flexion, extension, rotation, and side bending
Suboccipital muscles provide fine-tuned control of upper cervical movement, especially for head positioning
Key concept:
Stability and mobility are complementary: deep muscles stabilize while superficial muscles generate movement. Imbalance or weakness can lead to poor posture, pain, or risk of injury.
Mechanics of the Cervical Spine (Upper and lower)
Upper Cervical Spine (C0–C2) Mechanics
Atlanto-occipital joint (C0–C1):
Mainly flexion/extension (~10–15°), some lateral bending
Very little rotation
Atlanto-axial joint (C1–C2):
Primarily rotation (~50% of cervical rotation occurs here)
Some flexion/extension (~10°)
Minimal lateral bending
Key idea: Upper cervical spine provides rotation and fine positioning of the head.
2. Lower Cervical Spine (C3–C7) Mechanics
Facets oriented in an oblique plane (~45°): allows combined motion in all planes
Flexion/extension: ~35–40° per segment
Lateral bending: coupled with rotation to the opposite side
Axial rotation: ~30° per segment
Intervertebral discs allow translation and distribute load
Coupled motion: lateral bending and rotation often occur together due to facet orientation
Key idea: Lower cervical spine contributes to overall neck mobility and load-bearing.
Pathoanatomy of the Cervical Spine
Muscular Pathology
Strain or spasm of cervical muscles (SCM, trapezius, levator scapulae) → pain, limited ROM
Trigger points may refer pain to head, shoulder, or upper back
2. Joint Pathology
Facet joint dysfunction: pain with extension or rotation; may radiate locally or slightly laterally
Capsular irritation or synovitis → local pain and stiffness
3. Intervertebral Disc Pathology
Herniations or bulges: typically posterolateral → may impinge nerve roots
Degeneration: loss of disc height → facet overload, reduced motion
4. Spondylosis (degenerative changes)
Osteophyte formation → nerve root or spinal cord compression
Loss of cervical lordosis → altered biomechanics
5. Radiculopathy
Nerve root compression → pain, numbness, tingling along dermatomal distribution
Often from disc herniation or foraminal stenosis
6. Myelopathy
Spinal cord compression (from spondylosis, ligament hypertrophy, disc herniation)
Symptoms: gait disturbance, hand clumsiness, weakness, hyperreflexia
Review functional anatomy of thoracic spine and rib cage (joints, ligaments, muscles, discs, rib physiology)
1. Joints of the Thoracic Cage
Anterior Joints:
Sternocostal joints (ribs 1–7): connect ribs to the sternum
Interchondral joints (ribs 7–9): between costal cartilages
Costochondral joints: between ribs and their costal cartilages
Posterior Joints:
Costovertebral joints: rib head articulates with its own vertebral body and the one above
Costotransverse joints: rib tubercle articulates with the transverse process
Upper thoracic: convex rib, concave transverse process
Lower thoracic: planar joint
2. Ligaments
Ligamentum flavum – inside vertebral canal, connects laminae
Interspinous, supraspinous, intertransverse ligaments – connect spinous and transverse processes
Capsular ligaments – reinforce facet joints (dorsally by multifidi, ventrally by ligamentum flavum)
3. Muscles
Superficial and intermediate muscles:
Erector spinae: spinalis, longissimus, iliocostalis – posture, extension
Serratus posterior superior: elevates ribs 2–4
Serratus posterior inferior: depresses ribs 8–12
Deep muscles:
Intertransversarii: lateral stabilization
Levatores costarum: elevate ribs
Thoracic rotators: rotation and fine control
4. Thoracic Discs
Less mobile than cervical or lumbar discs
Herniation is rare
Disc changes (bulge, annular tears) may exist even in asymptomatic individuals
5. Rib Mechanics
Flexion of vertebra → anterior rotation of rib (internal rotation)
Extension of vertebra → posterior rotation of rib (external rotation)
Side bending: ribs on concave side approximate, ribs on convex side separate
Vertebral rotation: ipsilateral ribs posterior (external rotation), contralateral ribs anterior (internal rotation)
Respiratory movements:
Pump-handle motion: upper ribs, sagittal plane, increases anterior-posterior diameter
Bucket-handle motion: lower ribs, frontal plane, increases lateral diameter
6. Stability and Function
Thoracic spine stability comes from rib articulations, discs, ligaments, and musculature
Provides protection for thoracic organs and supports upper limb attachment
Guides rib motion for breathing mechanics
Clinical Decision-Making Framework (Patient/Client Management) - 4 componets
Four Core Components
Examination – Collect data
History: patient-reported info
Systems review: cardiovascular, pulmonary, neuromuscular, musculoskeletal, communication
Tests & measures: objective assessment of function, ROM, strength, special tests
Evaluation – Interpret findings
PT diagnosis
Prognosis (return to sport/work, expected recovery timeframe)
Intervention – Treatment delivery
Targeted exercises, manual therapy, patient education, etc.
Re-evaluation – Assess progress
Compare outcomes to initial comparable signs (reproduction of chief complaint)
Adjust plan of care as needed
Differentiate acute, subacute, chronic
Stage – acute (<10 days), subacute (10 days–7 weeks), chronic (>7 weeks), or mixed (acute on chronic)
Explain SINSS
Severity – pain intensity
Irritability – ease of onset, duration, intensity
Nature – type of tissue/structure involved
Stage – acute (<10 days), subacute (10 days–7 weeks), chronic (>7 weeks), or mixed (acute on chronic)
Stability – improving, worsening, or static symptoms
Explain the difference between ridiculophy, myeopthy, and neuropathy
Radiculopathy → Problem at the nerve root (spinal exit).
Causes: herniated disc, stenosis
Symptoms: radiating pain, numbness/tingling in dermatome, weakness
Myopathy → Problem in the muscle fibers.
Causes: genetic, inflammatory, drug-induced
Symptoms: proximal weakness, little/no sensory loss
Neuropathy → Problem in the peripheral nerves.
Causes: diabetes, toxins, vitamin deficiency
Symptoms: glove-and-stocking numbness, burning pain, weakness, ↓ reflexes
A 46 year old female presents to your clinic with neck and arm pain. You believe she has C8 radiculopathy. If you are accurate what did you find on your exam?
Decreased sensation over the medial antecubital fossa, decreased strength of finger abduction
Decreased sensation over the 3rd digit, decreased strength of wrist flexors
Decreased sensation over the thumb, decreased strength of wrist extensors
Diminished sensation on the 5th digit, decreased strength of thumb abduction
Diminished sensation on the 5th digit, decreased strength of thumb abduction
patient presents to your clinic with neck pain worse with cervical sidebending to the right and flexion. You hypothesize it is a joint restriction C5-C6. What is most likely happening?
C5-C6 on the right is not closing
C5-C6 on the left is not closing
C5-C6 on the right is not opening
C5-C6 on the left is not opening
C5-C6 on the left is not opening
DDD and DJD primarily on the right C6-7 level, may referred pain to this general location?
Over the occiput and upper neck on Right
Over the region of the upper trapezius on Left
Over the region of the upper trapezius on Right
Over the thoracolumbar junction (your response)
Over the region of the upper trapezius on Right
A 69-year-old female who has a 20-year history of neck pain has been working with a PT on cervical stabilization training. The patient has some difficulty, and the PT notices her chin poking out. Which muscle is she likely substituting with?
Longus caputus
Longus colli
Sternocleidomastoid
Middle scalenes
Sternocleidomastoid
If a PT is passively stretching a muscle by placing the patient in R cervical sidebending, L cervical rotation and slight neck flexion, which muscle is the PT stretching?
Left levator scapulae
Right levator scapulae
Left upper trapezius
Right upper trapezius (your response)
Left upper trapezius
What innervates levator scap?
Thoracodorsal
Accessory
Dorsal scapular
Suprascapular
Dorsal scapular
What nerve innervates the upper trapezius?
Doral scapular
Spinal accessory
Thoracodorsal
Suprascapular
Spinal accessory (your response)
A 58-year old male presents to your clinic with neck pain. During your examination you identified a tight right levator scapulae. How would you stretch the right levator scapulae?
Extend the neck, sidebend to the left, and rotate the head to the left
Flex the neck, sidebend to the left and rotate the head to the left
Extend the neck, sidebend to the left, and rotate the head to the right
Flex the neck, sidebend to the left and rotate the head to the right
Flex the neck, sidebend to the left and rotate the head to the left
A 78 year old male is referred to your clinic with loss of balance and numbness in bilateral upper extremities. The physician referral states your patient has cervical myelopathy. Cervical myelopathy is caused by:
Compression of the cauda equina in the lateral foramen
Compression of the spinal cord in the spinal canal
Compression of the nerve root in the vertebral foramen
Compression of the peripheral nerves due to cervical muscle spasm
Compression of the spinal cord in the spinal canal
A 32 year old female presents to your clinical with reports of neck pain which began 3 weeks ago. She notes the neck pain started after she was involved in a motor vehicle collision. Many anatomical structures can be damaged during a motor vehicle collision including the posterior longitudinal ligament. Which of the following is true of the posterior longitudinal ligament?
Resists sidebending
Resists flexion
Resists rotation
Resists extension
Resists flexion
You are performing an examination on an 45 year old female who woke up approximately 2-weeks ago with reports of neck pain. You identify restricted movement in the cervical spine. Decreased movement of the joints between the atlas and axis would result in?
Increased rotation of head/neck
Limited rotation head/neck
Limited flexion of head/neck
Increased flexion of head/neck
Limited rotation head/neck
A 32 year old male injured his neck when he slipped getting out of bed one night and hit his head on the wall. He reports he had an MRI which showed a herniated C5/C6 cervical disc and there are free floating fragments (pieces of the nucleus pulposus have broken off). This is known as a?
Extrusion
Disc degeneration
Prolapse
Sequestration
Sequestration
Which of the following is a poor prognostic indicator for long-term outcomes of neck pain?
A. Female sex
B. Age 20–30 years
C. Traumatic onset
D. Symptoms <2 weeks
✅ Correct Answer: C. Traumatic onset
Which risk factor is associated with the persistence of neck pain?
A. Prior low back pain
B. Male sex
C. High baseline pain intensity
D. Young athletic age
✅ Correct Answer: A. Prior low back pain
The alar ligaments primarily function to:
A. Limit extension of the occiput
B. Connect dens to occiput and limit rotation/side bending
C. Reinforce the vertebral body discs
D. Prevent forward translation of the atlas on the axis
B. Connect dens to occiput and limit rotation/side bending, prevents anterior and posterior displacement of the atlas on axid
Which cervical ligament is a continuation of the posterior longitudinal ligament (PLL)?
A. Ligamentum nuchae
B. Tectorial membrane
C. Cruciform ligament
D. Anterior atlanto-occipital ligament
B. Tectorial membrane
Which structure passes through the transverse foramen of the cervical vertebrae?
A. Carotid artery
B. Vertebral artery
C. Spinal cord
D. Internal jugular vein
B. Vertebral artery
Which muscle is most critical for motor control and stability of the cervical spine?
A. Upper trapezius
B. Longus colli
C. Sternocleidomastoid
D. Levator scapulae
B. Longus colli
The levator scapulae differs from the upper trapezius in rotation because it produces:
A. Contralateral rotation
B. Ipsilateral rotation
C. No rotation
D. Opposite action depending on position
✅ Correct Answer: B. Ipsilateral rotation
During cervical protraction (chin poke):
A. Upper cervical flexes, lower cervical extends
B. Upper cervical extends, lower cervical flexes
C. Both upper and lower cervical extend
D. Both upper and lower cervical flex
B. Upper cervical extends, lower cervical flexes
The ligamentum nuchae is a continuation of which structure?
A. Anterior longitudinal ligament
B. Supraspinous ligament
C. Ligamentum flavum
D. Posterior longitudinal ligament
B. Supraspinous ligament
The close-packed position of the atlanto-axial joint (C1–C2) is:
A. Flexion
B. Extension
C. Neutral
D. Protraction
A. extension
What is the action of the upper traps and how would i stretch it
action
extend
SB ipsilateral
Rotate Contralateral
stretch
flex
SB cont.
rotate ipsilateral
What is the action of the levator scap and how would i stretch it
action
extends, SB ipsilateral, rotate ipsilateral
stretch
flexion, SB cont. rotate cont.
What is the action of the scalenes and how would i stretch it
action
flexion, SB ipsilateral, rotate cont.
stretch
extend, SB cont, rotate ips.
What is the action of the SCM and how would i stretch it
action
Flexion of cerv spine
2. Extension of OA
3. SB ipsilateral
4. Rotate contralateral
stretch
extend, SB con., rotate ips. flex OA
Understand signs and symptoms that might be associated with serious pathology in individuals with neck pain. (6)
cervical fracture
cervical ligament instability
cervical myelopathy
cervical arterial dysfunction
cancer
systemic reffered pain
Recognize yellow flags in individuals with neck pain
Psychosocial factors that increase risk of disability/work loss (not malingering).
Recognize key patient history findings specific to the cervicothoracic region
Age
Sex
Occupation
History of present illness or chief complaint
Slow or sudden onset
5 Ds
3 Ns
cranial nerve signs
ataxia
Identify any precautions or contradictions
Precautions: suspected yellow flags (monitor closely, adjust treatment).
Contraindications (urgent/emergency referral):
Acute cervical fracture or instability.
Progressive neurological deficits (myelopathy).
Severe vascular symptoms (5 D’s, 3 N’s, ataxia).
Suspected cancer/systemic disease.
SINSS (severity, irritability, nature of complaint, stage, stability of disorder)
Understand the importance of using patient reported outcomes for measuring pain, function/disability and pain catastrophizing
Establish patient-centered functional goals
Third party payers are beginning to require outcome measures
Unbiased measure of the patient’s health status
Understand the minimal clinically important difference for outcome measures commonly used in patients with neck and thoracic pain
NPRS (pain):
Mechanical neck pain → 1.3–2 points
Cervical radiculopathy → 2.5 points
NDI (function/disability): 10–19%
PSFS: 2 points
FABQ: prognosis tool (not change measure).
PCS: ≥30 = clinically significant catastrophizing.
GROC: 4–5 = moderate improvement, 6–7 = large improvement.
what does the sharp purser test and transverse ligament test test
Sharp-Purser Test
Tests: Integrity of the transverse ligament of the atlas (C1).
Purpose: Detects instability at C1–C2.
Positive sign: Clunk or sliding motion of the atlas (C1) on the axis (C2), reduction of symptoms (especially neuro signs, dizziness).
Transverse Ligament Stress Test
Tests: Strength/stability of the transverse ligament directly.
Purpose: Checks if C1 can be displaced anteriorly on C2 (which could compress the spinal cord).
Positive sign: Reproduction of neurological symptoms (paresthesia, dizziness, nystagmus, nausea) or excessive soft end-feel.
how do you preform the sharp purser test
how do you preform the transverse ligament test
how do you preform the alar ligament test
=1. Sharp-Purser Test (Tests: Transverse Ligament / Atlantoaxial instability)
Purpose: Detect anterior translation of C1 on C2 (atlantoaxial instability, often in RA or trauma).
Steps:
Patient is sitting upright.
Examiner stabilizes C2 spinous process with one hand.
Examiner places the other hand on the forehead to apply a posteriorly directed force.
Patient may be asked to slightly flex the neck.
Observe for:
A “clunk” or sliding back of the head.
Reduction of symptoms (relief of dizziness, pain, or neurological signs).
Positive Test:
Posterior translation of the head with symptom relief → transverse ligament instability.
2. Transverse Ligament Stress Test
Purpose: Directly stresses the transverse ligament of C1.
Steps:
Patient is supine, neck slightly flexed (~20°).
Examiner grasps the head and gently anteriorly translates C1 relative to C2.
Monitor for:
Patient symptoms: dizziness, nausea, numbness, or paresthesia in extremities.
Excessive movement (may use radiograph for confirmation).
Positive Test:
Reproduction of neurological symptoms → transverse ligament compromise.
3. Alar Ligament Test
Purpose: Tests the alar ligaments, which limit rotation and side-bending of C1 on C2.
Steps:
Patient is supine, head in neutral position.
Examiner stabilizes C2 spinous process with one hand.
Examiner passively side-bends or rotates the head to one side.
Observe C2 movement:
Normally, C2 should move immediately with C1.
Positive Test:
Delayed or absent movement of C2 → alar ligament laxity/instability.
Patient may also report pain, numbness, or dizziness.
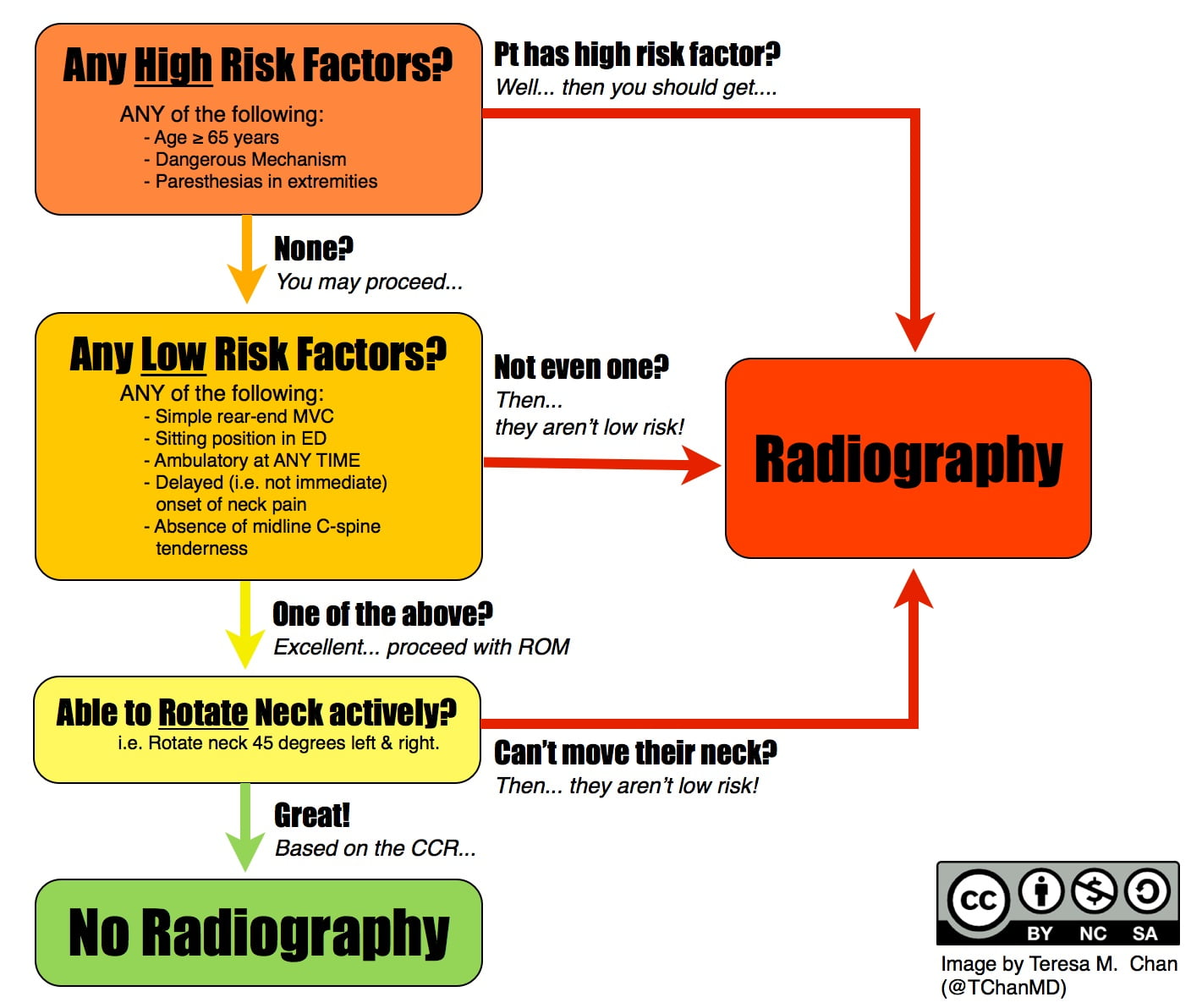
c spine rule
what are the 5 Ds and 3 Ns
1.dizziness
2.Drop attacks - falling
3. Dysphagia - difficulty swallowing
4. Dysarthria - slurred speech
5. Diplopia - seeing double
6. Nausea
7. Numbness
8. Nystagmus - an involuntary, rhythmic oscillation of the eyes
what indicates cervical myelopathy
Babinski - extension of toes instead of flexion of toes in response to sole of foot being stroked
Hoffman's - tapping or flicking of 3rd digit to bring together the thumb and index finger
clonus - rhythmic beating movements of the ankle with firm 90 streth of ankle and achilles tendon
hyperreflexia - an overactive muscle reflex, often indicating a problem with the brain or spinal cor
MCID (minimum clinically important difference) vs MCII (minimum clinically important improvement)
MCID - The smallest change in an instrument that is perceived to an important difference by the patient.
MCII - The smallest change in an instrument that is perceived to be beneficial by the patient.
what numbers are skipped in the fabq
1, 8, 13, 14, 16
explain SINSS

A patient was involved in a MVC 2 weeks ago and fractured their left femur and sustained a whiplash injury. They underwent an ORIF to repair the fracture and now come to see you. Their NDI score is 14 points. This means?
No disability
Mild disability
Moderate disability
Severe disability
A patient reports to your clinic and scores a 4 on the patient specific functional scale. To be confident that the patient meets the minimal clinically important improvement they must score at least which of the following?
2
3
5
6
6
On your observation your patient has forward shoulder. You hypothesize they might have a tight pectoralis major (sternal portion). The position to assess this would be?
Patient supine arm in 30 degrees of abduction
Patient supine arm in 60 degrees of abduction
Patient supine arm in 90 degrees of abduction
Patient supine arm in 120 degrees of abduction
Patient supine arm in 120 degrees of abduction
You have a patient with neck and arm pain. You want to place them in a position neurodynamic tension for the ulnar nerve. The best position for this is?
Shoulder abduction and ER, elbow extended, forearm supinated, wrist and fingers extended
Shoulder abduction and ER, elbow flexed, forearm supinated, wrist and fingers extended
Shoulder abduction and ER, elbow extended, forearm pronated, wrist and fingers extended
Shoulder abduction and ER, elbow flexed, forearm pronated, wrist and fingers extended
Shoulder abduction and ER, elbow flexed, forearm pronated, wrist and fingers extended
You have a patient supine and maximally flex the head then rotate to both sides. One side if 45 degrees and the other is 30 degrees. This is indicative of?
Tension headache
Cervicogenic headache
Hypomobile first rib
Cervical radiculopathy
Cervicogenic headache
You have a patient who "strained" their neck while lifting their kayak onto the roof rack. You want to test their neck flexor muscle endurance test. What is a normal hold time for asymptomatic people?
10 seconds
20 seconds
30 seconds
40 seconds
40 seconds
A patient presents to your clinic with reports of neck pain that started when he was participating in a caber toss competition. A normal reading for the craniocervical flexion test would be?
10 second hold at 20 mm HG
10 second hold at 24 mm HG
10 second hold at 26 mm HG
10 second hold at 30 mm HG
10 second hold at 26 mm HG
A 65 yo old patient reports to your clinic with neck pain with radicular symptoms. You find the hand intrinsic muscles (abductors) to be 4-/5 and sensation on the medial aspect of the forearm is slightly decreased. You hypothesize involvement of?
C6
C7
C8
T1
T1
A patient presents to you clinic following a MVC and reports facial numbness. You are expecting cranial nerve involvement. Which cranial nerve is involved if you are accurate?
Optic
Trigeminal
Hypoglossal
Trochlear
Trigeminal
Your patient is a 46 yo male who was involved in a MVC. You are performing ligamentous testing to the cervical spine and find a positive Sharp Purser test and find it to be positive. This is indicative of what ligament?
Alar
Nuchal
Posterior longitudinal
Transverse
Transverse
A 26 yo female presents with left sided neck pain. She notes it started after a backpacking trip. You perform your exam and find that she has decreased flexibility of the right SCM. What position would you put the cerv spine to stretch the right SCM?
Chin retraction, SB left, rot right
Chin retraction, SB left, rot left
Chin retraction, SB right, rot left
Chin retraction, SB right, rot right
Chin retraction, SB left, rot right
Which of the following is most consistent with cervical myelopathy?
A. Local neck pain that improves with rest
B. Numbness in the face and dizziness with neck rotation
C. Wide-based gait, hyperreflexia, and hand muscle wasting
D. Pain with cervical rotation that decreases with manual traction
✅ Answer: C – Wide-based gait, hyperreflexia, hand wasting = UMN signs/myelopathy.
Which statement best describes a yellow flag in a patient with neck pain?
A. A red flag indicating cancer or vascular pathology
B. A psychosocial factor that increases the risk of long-term disability
C. A malingering behavior where the patient fakes pain
D. A contraindication to beginning physical therapy
✅ Answer: B – Yellow flags are psychosocial barriers, not faking.
A 70-year-old woman presents after a fall in her bathroom. Which finding would make you most concerned for a cervical fracture?
A. Delayed onset of neck pain
B. Ability to rotate head 45° each way
C. Midline cervical spine tenderness
D. Sitting position in ED without distress
✅ Answer: C – Midline tenderness is a high-risk finding for fracture.
Which of the following would be an absolute contraindication to continuing physical therapy without referral?
A. Patient reports fear that pain will worsen with activity
B. Patient reports dizziness and diplopia after neck movement
C. Patient has mild anxiety about returning to work
D. Patient avoids vacuuming due to pain
✅ Answer: B – Dizziness + diplopia = vascular red flag → immediate referral.
A 45-year-old male presents with neck pain, radicular arm pain, and bowel/bladder changes. Based on history alone, what is the most likely hypothesis?
A. Mechanical neck pain with yellow flags
B. Cervical fracture
C. Cervical myelopathy
D. Cervical arterial dysfunction
Answer: C – Radicular arm pain + bowel/bladder + age >45 = myelopathy
What is the MCID for the Numeric Pain Rating Scale (NPRS) in mechanical neck pain?
A. 0.5 points
B. 1.3–2 points
C. 2.5 points
D. 10–19%
B – NPRS MCID for mechanical neck pain = 1.3–2 points.
A patient completes the Neck Disability Index (NDI) and scores 20/50. How is their level of disability classified?
A. Mild
B. Moderate
C. Severe
D. Complete
Score 15–24 = moderate disability.
Which tool is used primarily for prognosis and not for detecting change over time?
A. NDI
B. NPRS
C. FABQ
D. PSFS
Answer: C – FABQ = prognosis (fear-avoidance beliefs).
A score of ≥30 on the Pain Catastrophizing Scale (PCS) indicates:
A. Severe physical disability
B. Clinically significant catastrophizing
C. Minimal clinically important difference
D. Prognosis for rapid recovery
Answer: B – PCS ≥30 = clinically significant catastrophizing.
The Sharp-Purser Test is positive when:
A. The patient reports increased dizziness and nausea
B. There is reproduction of local pain in the posterior neck
C. A clunk is felt and symptoms decrease when posterior force is applied to the forehead
D. The patient is unable to rotate the head 45°
C – Sharp-Purser reduces symptoms with clunk → transverse ligament instability.
Which cluster of symptoms is most consistent with cervical arterial dysfunction?
A. Headaches, radicular pain, bowel/bladder dysfunction
B. Drop attacks, diplopia, dysarthria, dizziness
C. Delayed onset neck pain, ability to sit, ability to ambulate
D. Wide-based gait, Hoffman’s sign, Babinski sign
B – The “5 D’s” = vascular insufficiency.
In managing a patient with strong yellow flags, which of the following strategies is most appropriate?
A. Rely primarily on passive treatments (modalities, rest)
B. Provide education that “pain does not always equal harm” and use graded activity
C. Refer immediately to the ER for imaging
D. Avoid activity to prevent further tissue damage
✅ Answer: B – Education + graded activity = key management.
A patient with cervical radiculopathy reports their pain dropped from 7/10 to 5/10 on the NPRS. Is this change clinically meaningful?
A. Yes, because the change is ≥1 point
B. No, because the change does not reach the MCID of 2.5 points
C. Yes, because any decrease in pain is meaningful
D. No, because NPRS cannot be used in cervical radiculopathy
B – MCID for cervical radiculopathy = 2.5 points
Which of the following positive findings would raise strong suspicion for cervical myelopathy?
A. Decreased deep tendon reflexes, younger than 30 years old, pain relief with rest
B. Wide-based gait, positive Babinski sign, positive Hoffman’s sign, age >45
C. Normal gait, negative Hoffman’s, localized paraspinal tenderness
D. Limited cervical ROM, relief with cervical traction, negative inverted supinator sign
✅ Answer: B – The Wainner Myelopathy Cluster includes:
Wide-based gait deviation
Positive Hoffman’s sign
Inverted supinator sign
Positive Babinski sign
Age >45
Patient-Reported Outcomes (PROs) for Cervical Spine medical history
NDI – Neck Disability Index
Measures: Neck-specific disability.
Scoring: 10 items, each 0–5 → total ×2 = % disability (0–100%).
0–4 = None, 5–14 = Mild, 15–24 = Moderate, 25–34 = Severe, ≥35 = Complete disability.
MCID: 10–19%.
NPRS – Numeric Pain Rating Scale
Measures: Pain intensity (current, best, worst).
Scoring: 0 = no pain → 10 = worst imaginable pain.
MCID: 1.3–2 points (mechanical neck pain), 2.5 points (cervical radiculopathy).
VAS – Visual Analog Scale
Measures: Pain intensity.
Scoring: 10 cm line → patient marks pain between 0 (no pain) and 10 (worst pain).
MCID: about 1.3–2 cm.
PCS – Pain Catastrophizing Scale
Measures: Catastrophic thinking related to pain (rumination, magnification, helplessness).
Scoring: 13 items, each 0–4 → total 0–52.
≥30 = clinically significant catastrophizing.
MCID: None established, ≥30 used as cutoff.
FABQ – Fear-Avoidance Beliefs Questionnaire
Measures: Beliefs about how activity/work may worsen pain.
Scoring: 16 items, each 0–6 → two subscales:
Physical Activity (0–24)
Work (0–42)
Higher scores = worse prognosis.
MCID: None (prognostic, not change-sensitive).
PSFS – Patient-Specific Functional Scale
Measures: Functional limitations chosen by patient.
Scoring: 3–5 activities rated 0 (unable) → 10 (normal).
MCID: 2 points.
GROC – Global Rating of Change
Measures: Overall perception of change since treatment started.
Scoring: –7 = very much worse → 0 = no change → +7 = very much better.
+4 to +5 = moderate improvement.
+6 to +7 = large improvement.
MCID: +4 or higher.
Which ligaments are primarily assessed in ligamentous instability tests?
A. Transverse and alar ligaments
B. Anterior longitudinal ligament only
C. Ligamentum flavum
D. Supraspinous and interspinous ligaments
A – Transverse and alar ligaments maintain upper cervical stability.
Thoracic pain may be referred from all of the following except:
A. Stomach/pancreas
B. Heart/lungs/diaphragm
C. Liver/gallbladder
D. Biceps tendon
✅ Answer: D – Biceps tendon pain is musculoskeletal, not systemic referral.
A patient presents with neck pain, bilateral leg weakness, hyperreflexia, and hand clumsiness. Based on history alone, the most likely hypothesis is:
A. Cervical fracture
B. Cervical myelopathy
C. Cervical ligamentous instability
D. Muscular strain
✅ Answer: B – UMN signs + bilateral symptoms = myelopathy.
Which muscles are typically tight in upper crossed syndrome?
A. Deep neck flexors and lower trapezius
B. Pectoralis major, upper trapezius, levator scapulae
C. Serratus anterior and rhomboids
D. Gluteus maximus and hamstrings
Answer: B. Pectoralis major, upper trapezius, levator scapulae
Which muscles are usually weak in upper crossed syndrome?
A. Upper trapezius and levator scapulae
B. Pectoralis major and minor
C. Deep neck flexors, lower trapezius, serratus anterior
D. Latissimus dorsi and teres major
Answer: C. Deep neck flexors, lower trapezius, serratus anterior
How many supine head lift repetitions are considered “functional”?
A. 1–2 reps
B. 3–5 reps
C. 6–8 reps
D. 0 reps
Answer: C. 6–8 reps
In the prone head lift (extension) test, holding the head up for 12 seconds is considered:
A. Functional
B. Functionally fair
C. Functionally poor
D. Nonfunctional
Answer: B. Functionally fair
Which of the following is NOT an indication for balance testing in a patient with neck pain?
A. Presence of cervicogenic dizziness
B. Positive cranial nerve findings
C. Patient reports occasional mild neck stiffness
D. Ataxia
Answer: C. Patient reports occasional mild neck stiffness
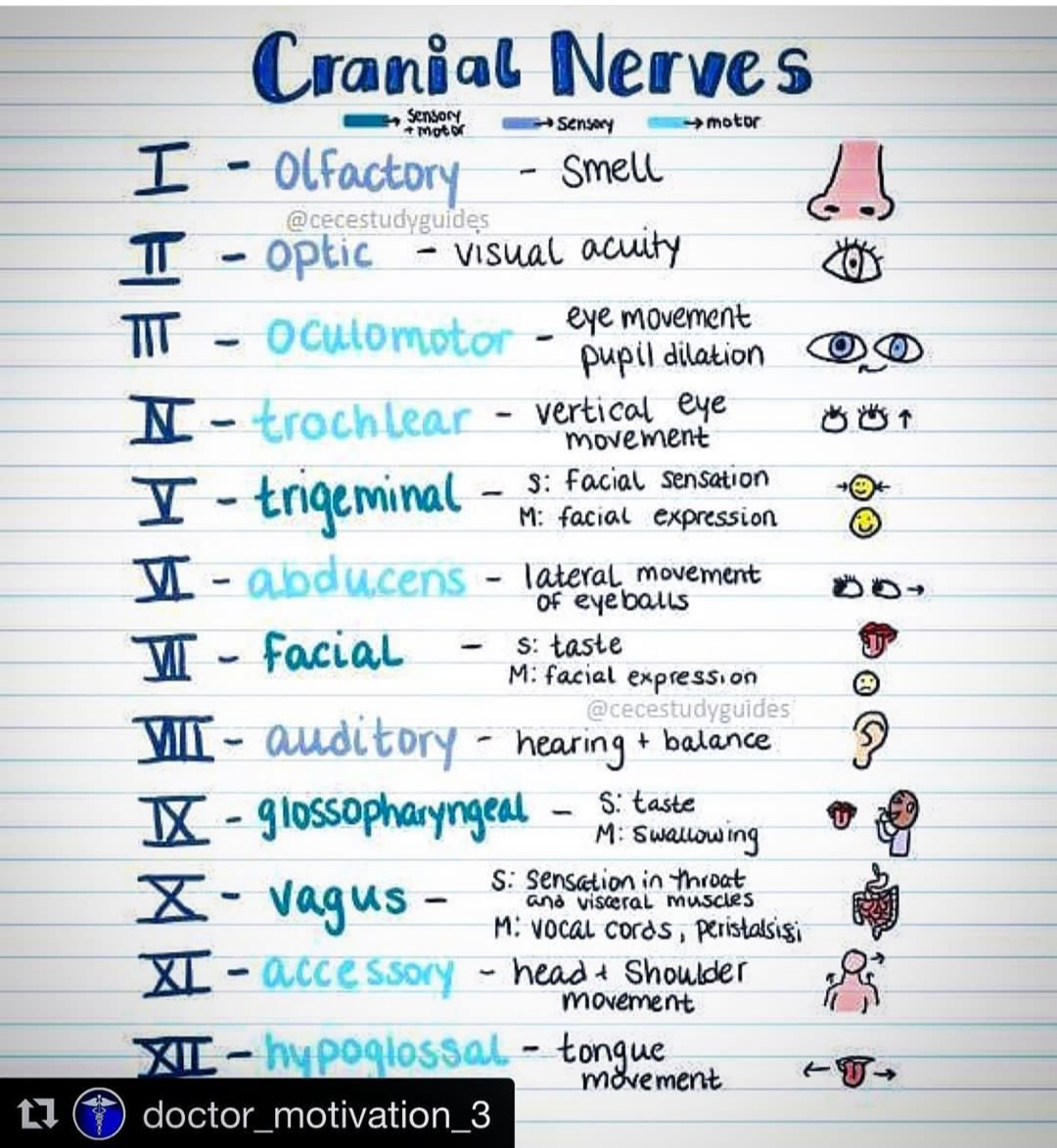
name the cranial nerves and their action
To place the radial nerve in a position of tension (not considering the c-spine position) the patient should be in which of the following position?
Shoulder depressed, shoulder IR, forearm pronation, wrist flexion and ulnar deviation
Shoulder depressed, shoulder IR, forearm supinated, wrist flexion and radial deviation
Shoulder depressed, shoulder IR, forearm pronation, wrist extension and ulnar deviation
Shoulder depressed, shoulder IR, forearm pronation, wrist flexion and radial deviation
Shoulder depressed, shoulder IR, forearm pronation, wrist flexion and ulnar deviation
Why is pathoanatomical diagnosis often challenging in neck pain?
Patients rarely report pain clearly
Imaging may not identify the pain source
Physical therapists lack adequate diagnostic tools
Pain is often psychosomatic
Imaging may not identify the pain source
If a patient presents with red flags, what is the correct action?
Begin physical therapy treatment
Continue but monitor symptoms
Refer to social worker for consultation
Refer to physician
Refer to physician
Which term refers to a flare-up of symptoms on top of a long-standing problem?
Chronic flare
Persistent subacute
Acute on chronic
Persistent chronic
Acute on chronic (your response)
The acronym SINSS includes
Signs, Imaging, Nerve, Staging, Sensitivity
Sensory, Intensity, Neurological, Structural, Stress
Stability, Irritability, Nerve, Severity, Symptoms
Severity, Irritability, Nature, Stage, Stability
Severity, Irritability, Nature, Stage, Stability (your response)
Minimal irritability means:
Pain worsens quickly and lingers
Pain comes on slowly and eases quickly
Pain does not change with activity
Pain always requires medication
Pain comes on slowly and eases quickly
Which of the following is a hallmark symptom of the mobility deficit classification?
Centralized or unilateral neck pain
Constant bilateral arm numbness (your response)
Headaches radiating from the occiput
Pain radiating to the hand
Centralized or unilateral neck pain
Manual therapy in the mobility deficit classification should always be combined with:
Passive modalities
Exercise
Medication
Traction
Exercise
Which of the following is the most common mechanism of onset for movement coordination impairments?
Degenerative disc disease
Whiplash
Postural syndrome
Osteoarthritis
Whiplash
Cervicogenic headaches are typically:
Bilateral and constant
Bilateral and not constant
Unilateral and constant
Unilateral and not constant
Unilateral and not constant
What is the purpose of the Distraction test?
To assess nerve root compression
To detect vertebral artery insufficiency
To evaluate ligamentous laxity (your response)
To check for first rib dysfunction
To assess nerve root compression