phsyio exam 3
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
95 Terms
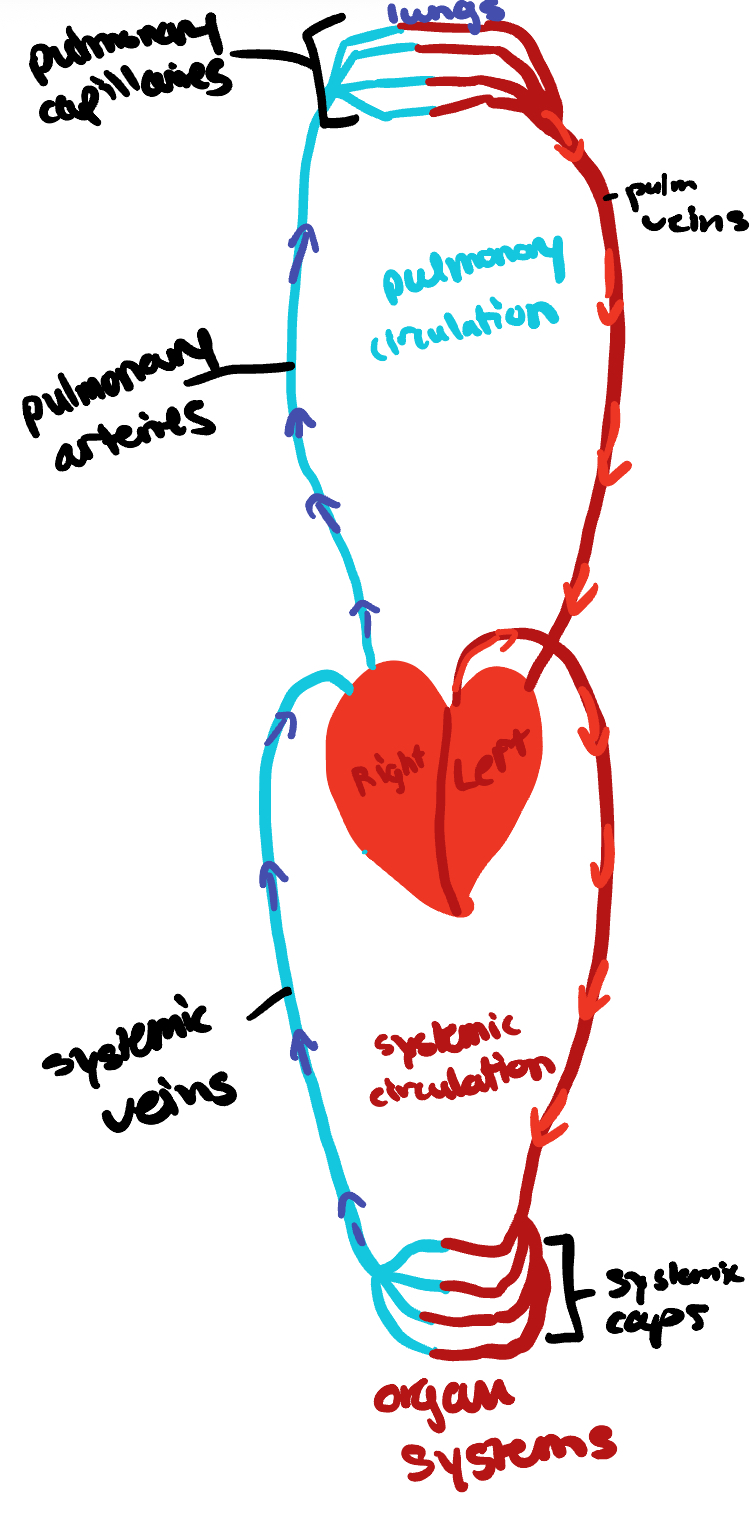
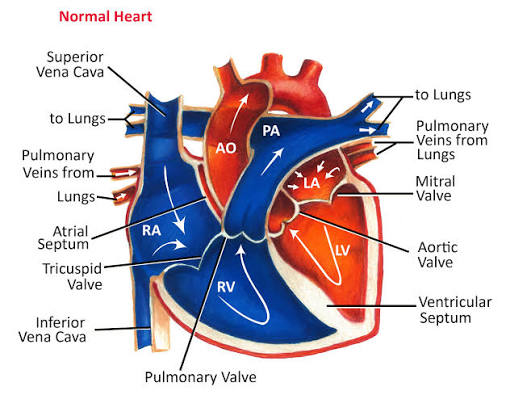
Describe and draw the circulatory routes
Pulmonary: closed loop of vessels, carrying blood between heart and lungs
Systemic: circuit of vessels, carrying blood between heart and other body systems
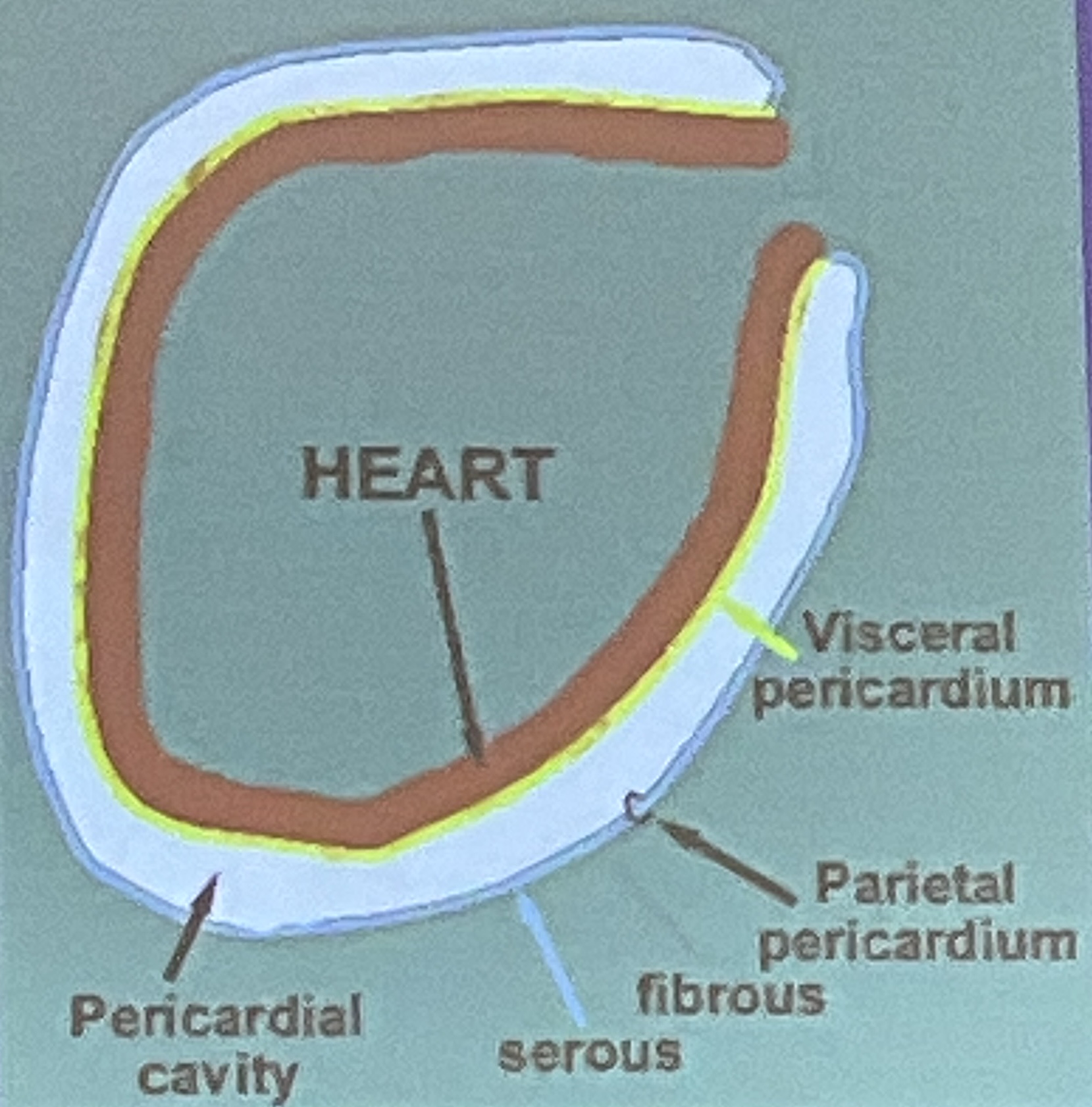
Location and cavities of the heart
Ventral, thoracic, mediastinum, pericardial
Coverings of the heart
Visceral pericardium; serous membrane on the heart
Parietal pericardium: serous membrane lining the cavity
What are the layers of the heart?
Endothelium myocardium epicardium
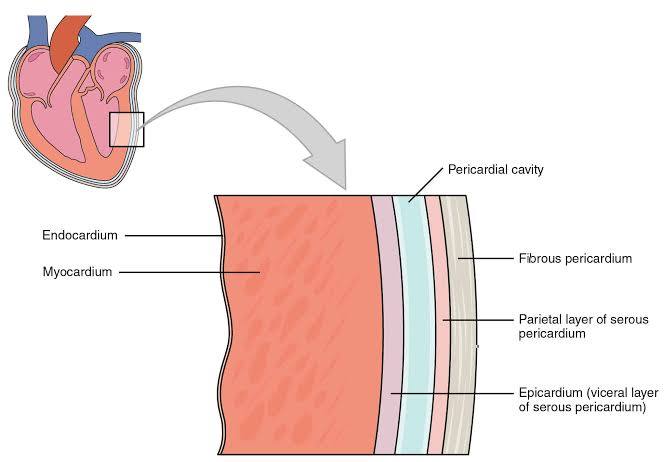
Endothelium
Thin inner tissuw
Epithelial tissue which lines entire circulatory system
Myocardium
Middle layer, composed of cardiac tissue, constitutes bulk of heart wall, does contraction
Epicardium
Thin external layer that covers the exterior of the heart also known as visceral pericardium
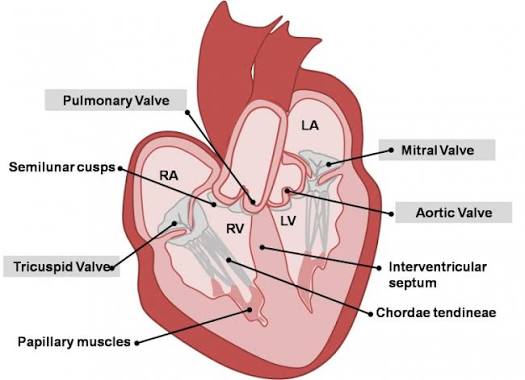
What are the four chambers of the heart?
Atria and ventricles
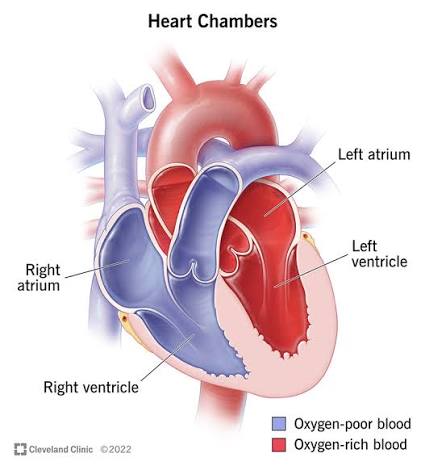
Job of the atria
Upper chambers that receive blood returning to the heart and transfer it to lower chambers
Job of the ventricles
Lower chambers which pump blood from the heart
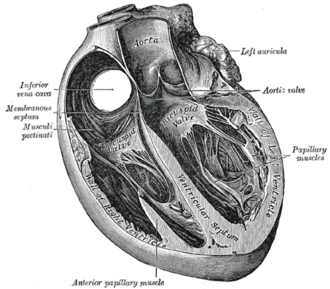
What is the job of the septums ? interventricular interartial
Continuous muscular partition that prevents mixture of blood from the two sides of the heart
What are the two types of valves?
Atrioventricular and semi lunar
Right and left AV valves are positioned between the ____ on right and left sides
Atrium and ventricle
What is the purpose of the AV valve?
Prevent backflow into atria from ventricles during ventricular contraction
What are the two types of AV valves?
Right AV-tricuspid valve
left AV- bicuspid or Mitral valve
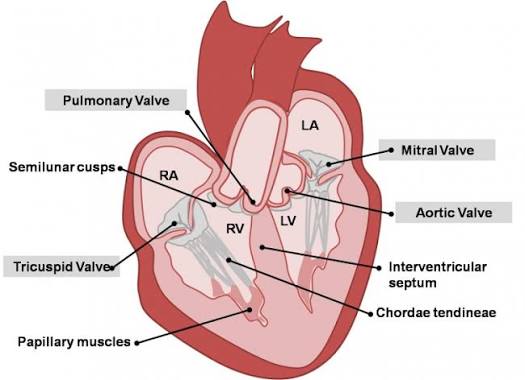
Function of chordae tendinae
Fibrous chords which prevent valves from being averted and inverted during ventricular contraction
Function of papillary muscles
Anchor the cordae tendinae to the muscular ventricular wall
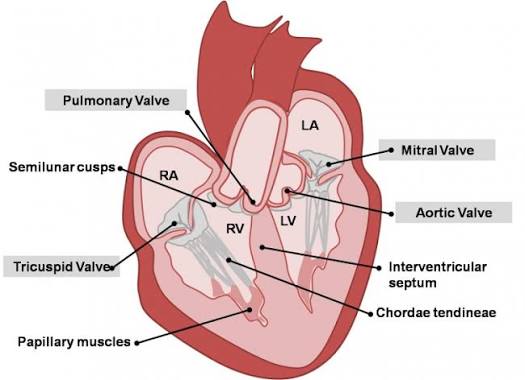
function of semilunar valves
Lie at juncture where major arteries Leave ventricles
prevent backflow of blood into ventricles
What are the two types of semilunar valves?
Aortic valve, which is between the left ventricle and the aorta
Pulmonary valve, which is between the right ventricle and the pulmonary trunk
Arteries definition
Carry blood away from ventricles to tissues
Veins definition
Vessels that return blood from tissues to the atria
Path of blood flow throughout the heart and body
1: Deoxygenated blood enters right atrium from the superior vena cava and inferior vena cava and coronary sinus
2: tricuspid valve
3: right ventricle
4: pulmonary semilunar valve
5: pulmonary trunk → pulmonary arteries → lungs
6: oxygenated blood enters left atrium from pulmonary veins
7: mitral valve
8: left ventricle
9: aortic semilunar valve
10: aorta → body
Definition of autorhythmicity
Heartbeats rhythmically as result of action potential it generates by itself
What are the two types of cardiac muscle fibers?
Contractile cells and pacemaker cells
Describe contractile cells
99% of cardiac muscle cells, do mechanical work of pumping, normally do not initiate on electrical activity
Describe pacemaker cells
Do not contract, specialized for initiating action, potential responsible for contraction of working cells
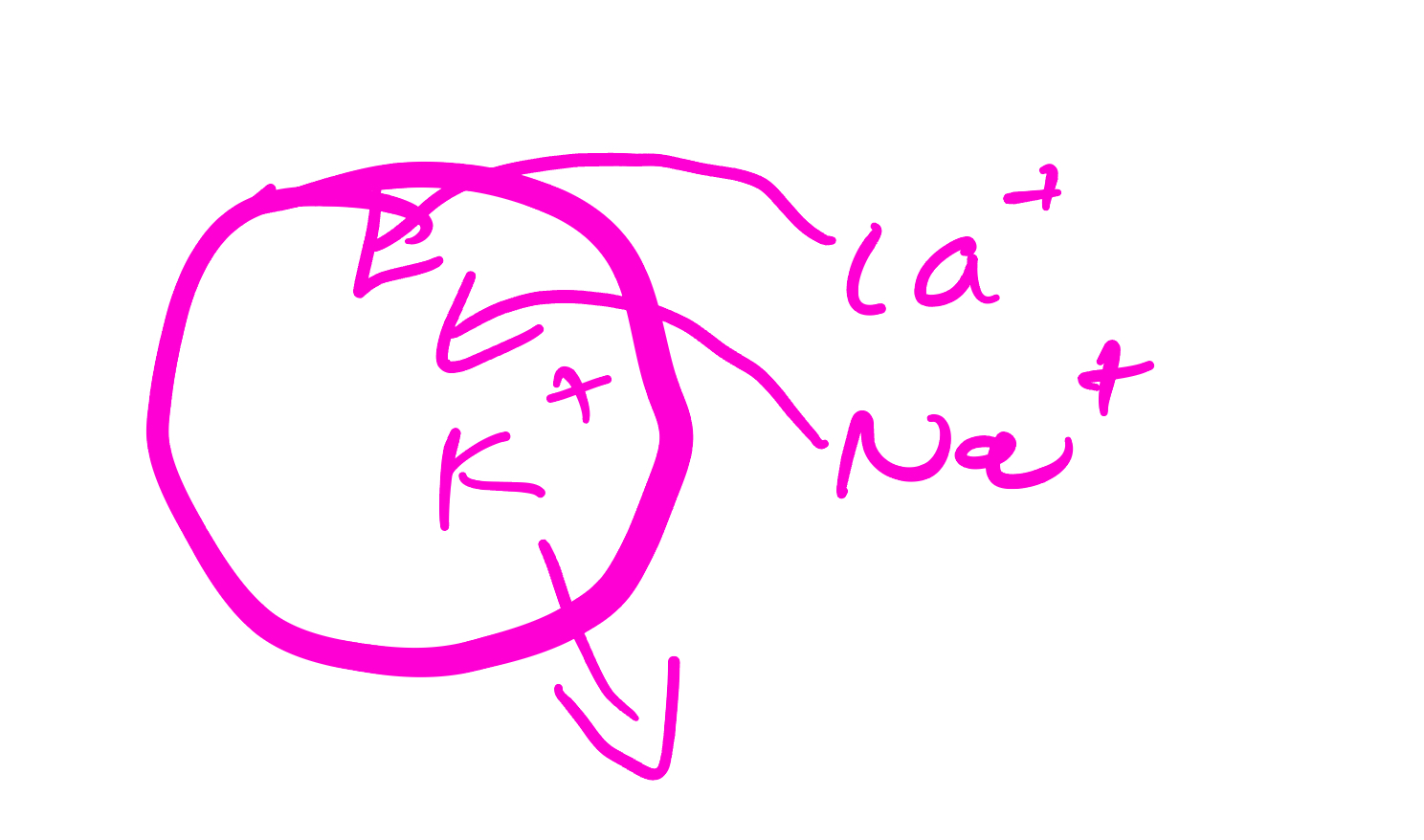
Draw the cell with calcium sodium and potassium where they are in higher concentration and draw arrows to show where they will diffuse
Draw pacemaker potential and label the changes in permeability of the ions that are responsible for generating the pacemaker potential
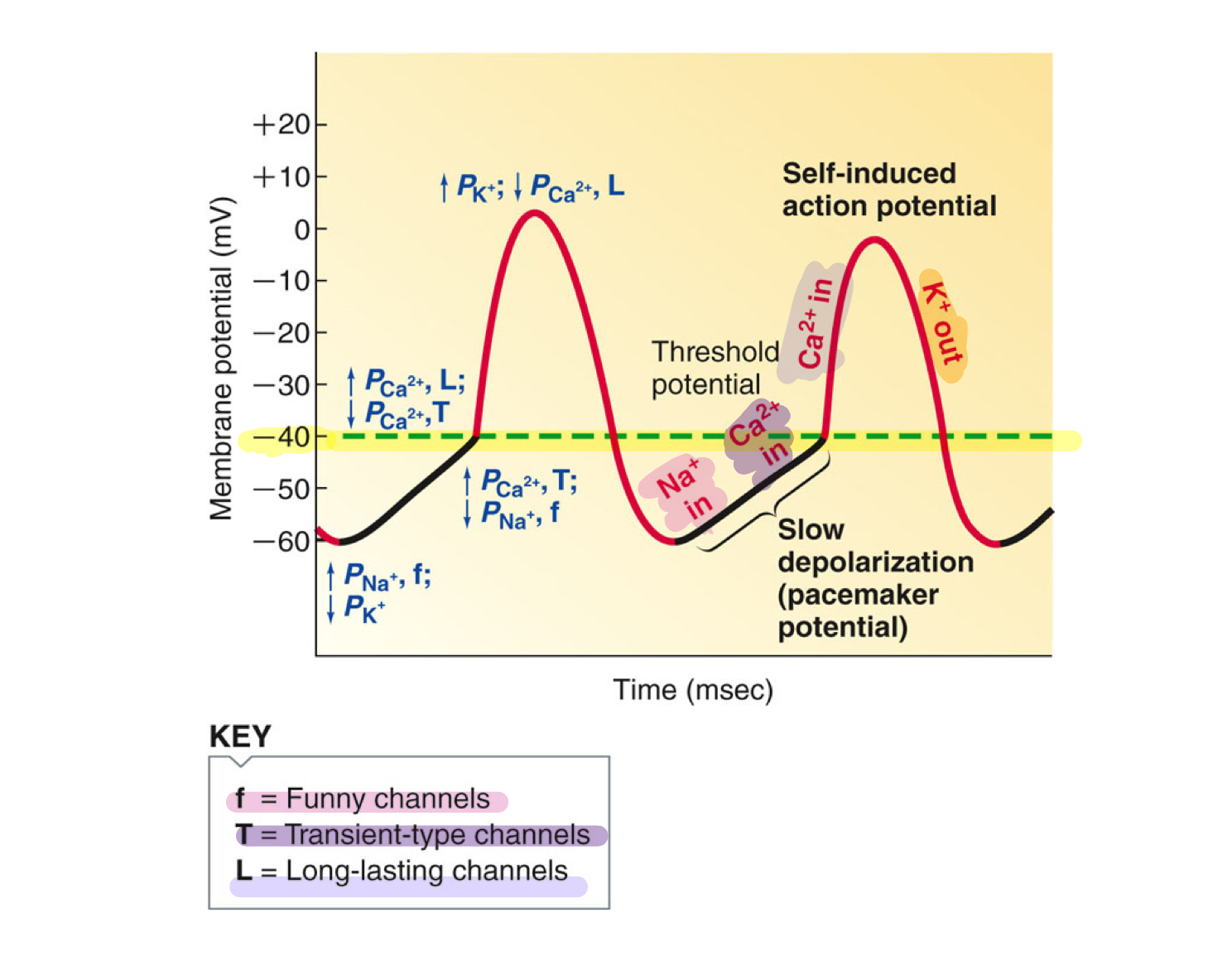
list the steps involved in the generation of a pacemaker potential
Sodium channels open at -60mV
Calcium T type slow leak into threshold (-40)
L Type open= depolarize
Potassium open to repolarize
Start over again with sodium= MP drifts up
Deoxygenated blood enters what chamber of the heart?
RA
What veins deliver oxygenated blood to the heart
Pulmonary veins
What valves do not have chordae tendinae
Semilunar valves: pulmonary and aortic
What valve prevents blood from re-entering the right atrium
Tricuspid valve
What chamber receives blood from the coronary sinus?
Right atrium
What are the first two branches of the aorta?
Right and left coronary arteries
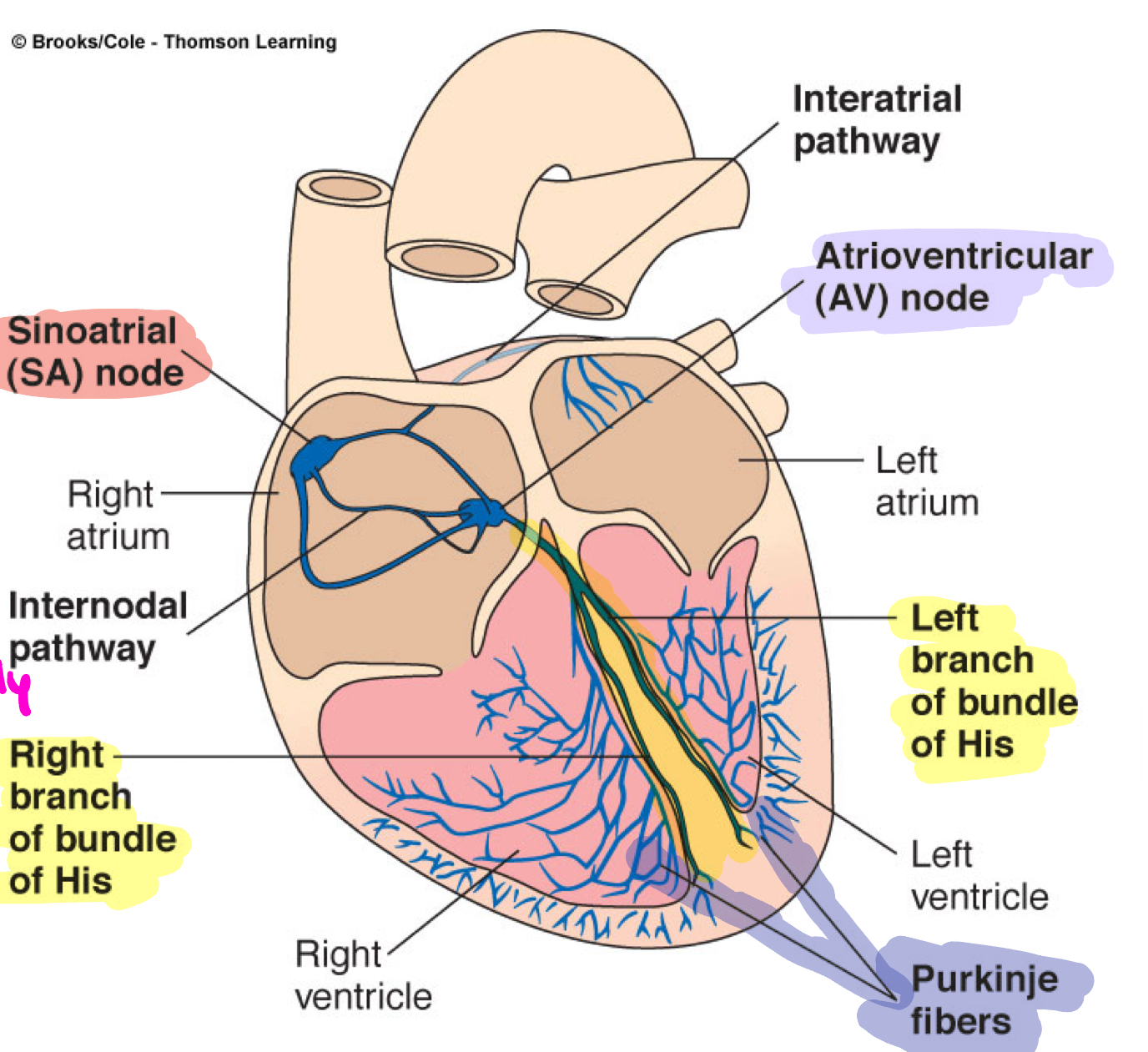
where are the pacemaker cells found in the heart?
SA node
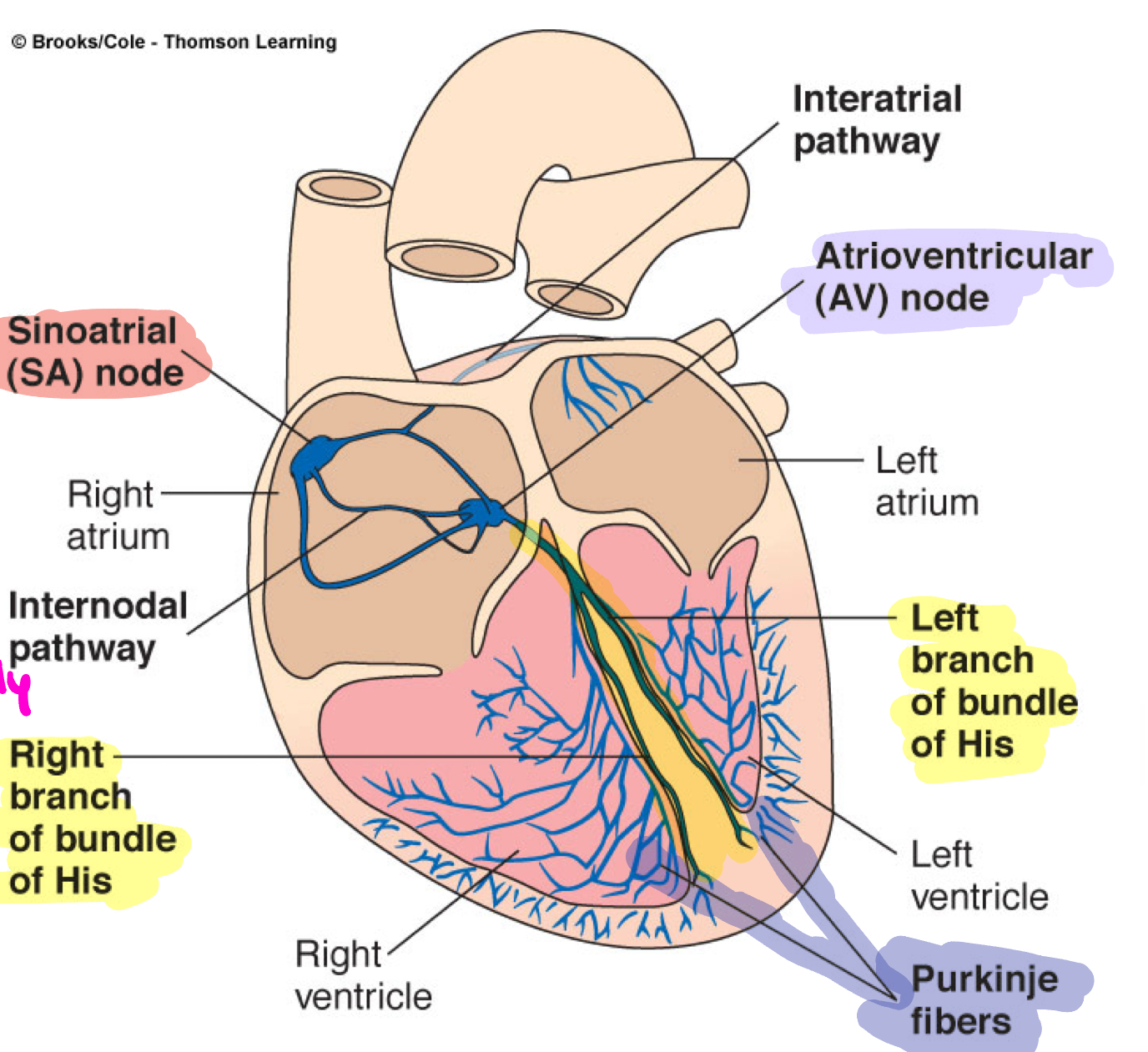
If the SA and AV node do not work, what will be the pacemaker and what will the heart rate be?
Purkinje fibers
20-40
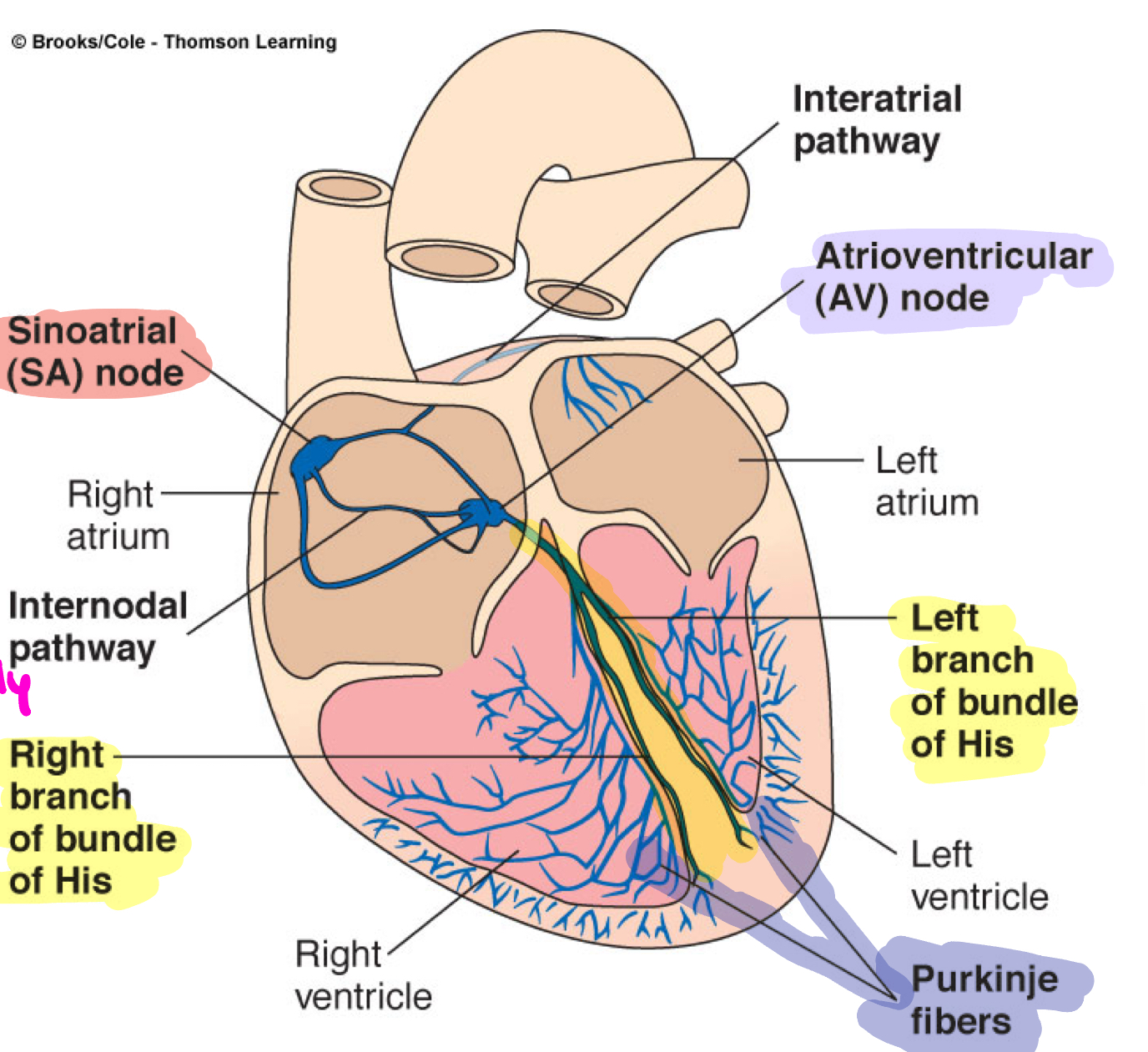
List the steps in the conduction circuit
cardiac impulse originates at SA node
action potential spreads throughout right and left atria
atria contract
impulse passes from atria to ventricles through AV node
action potential briefly delayed at AV node
impulse travels rapidly down interventricular septum by means of bundle of his then to L and R Bundle branches
impulse rapidly disperes throughout myocardium by means of Purkinje fibers
rest of ventricular cells activated by cell-to-cell spread of impulse through gap junctions
ventricles contract
What initiates the cardiac cycle?
Electrical impulses from the sinoatrial (SA) node.
What mechanical event follows SA node activation?
Atrial contraction (atrial systole).
What is the role of the atrioventricular (AV) node in the cardiac cycle?
It delays the impulse to allow the atria to fully contract before the ventricles do.
Through which structures does the impulse travel after the AV node?
The Bundle of His and Purkinje fibers.
What mechanical event is triggered by ventricular depolarization?
Ventricular contraction (ventricular systole).
What happens during ventricular repolarization?
The ventricles relax (diastole), allowing the heart to refill with blood.
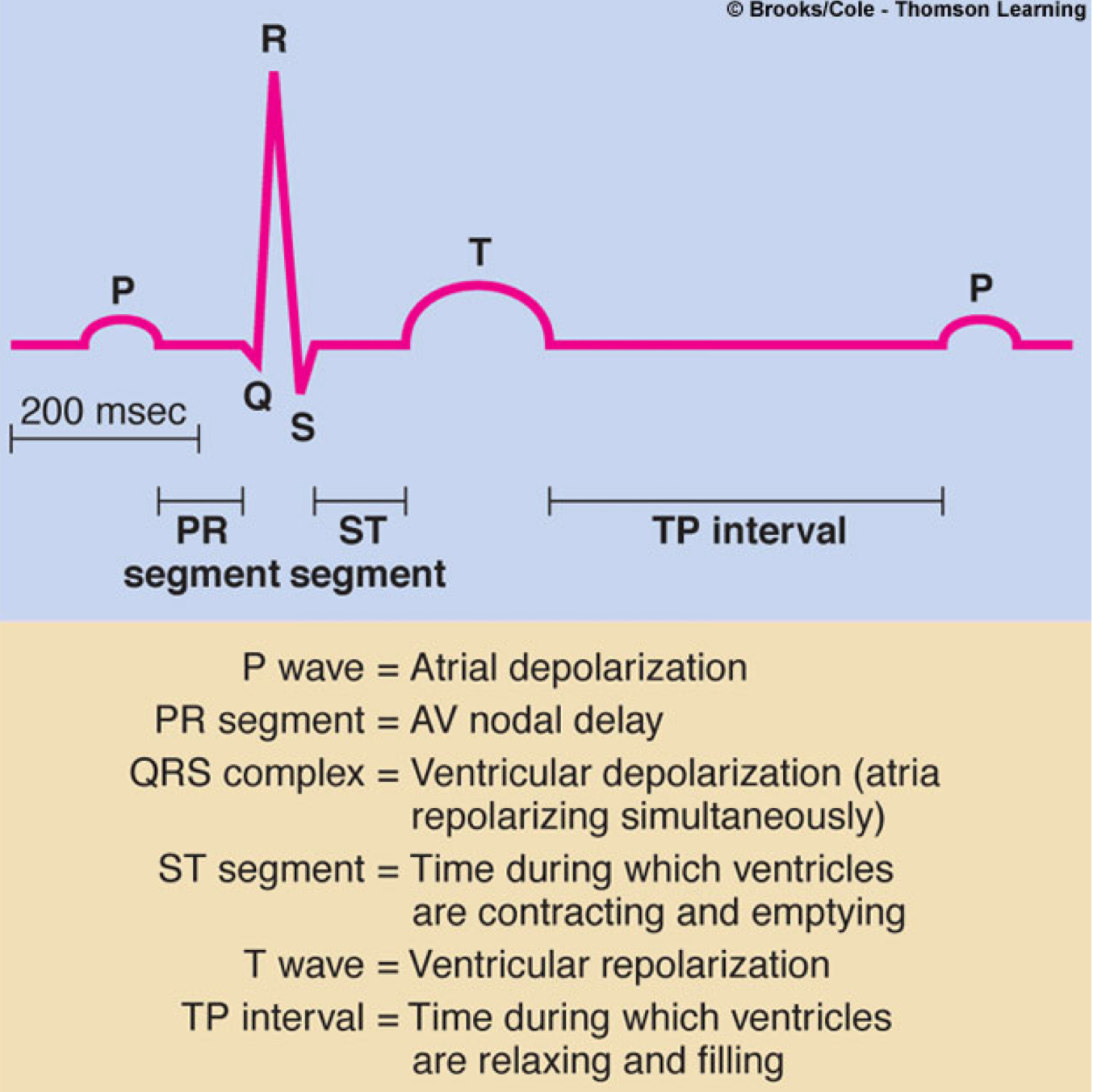
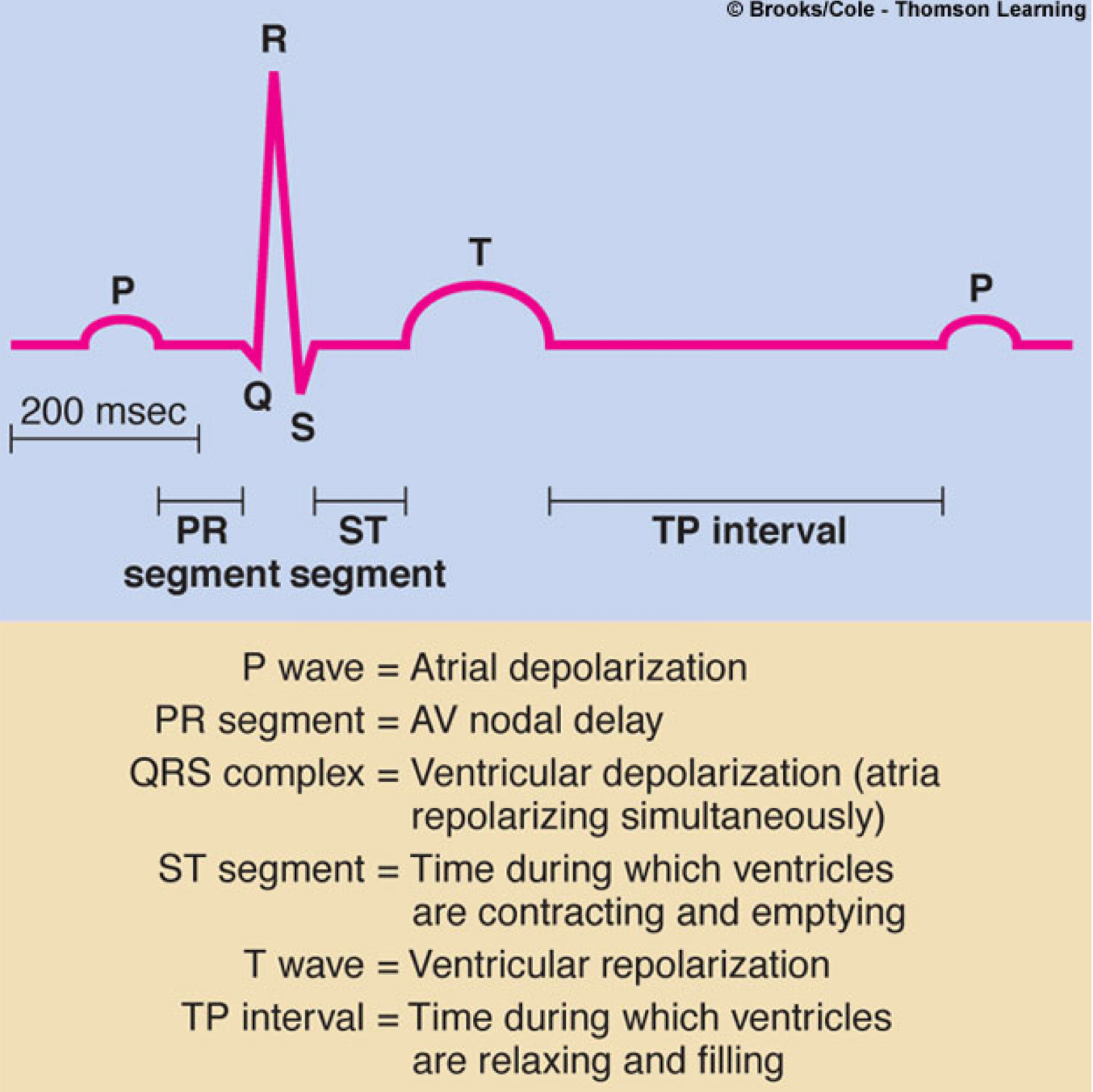
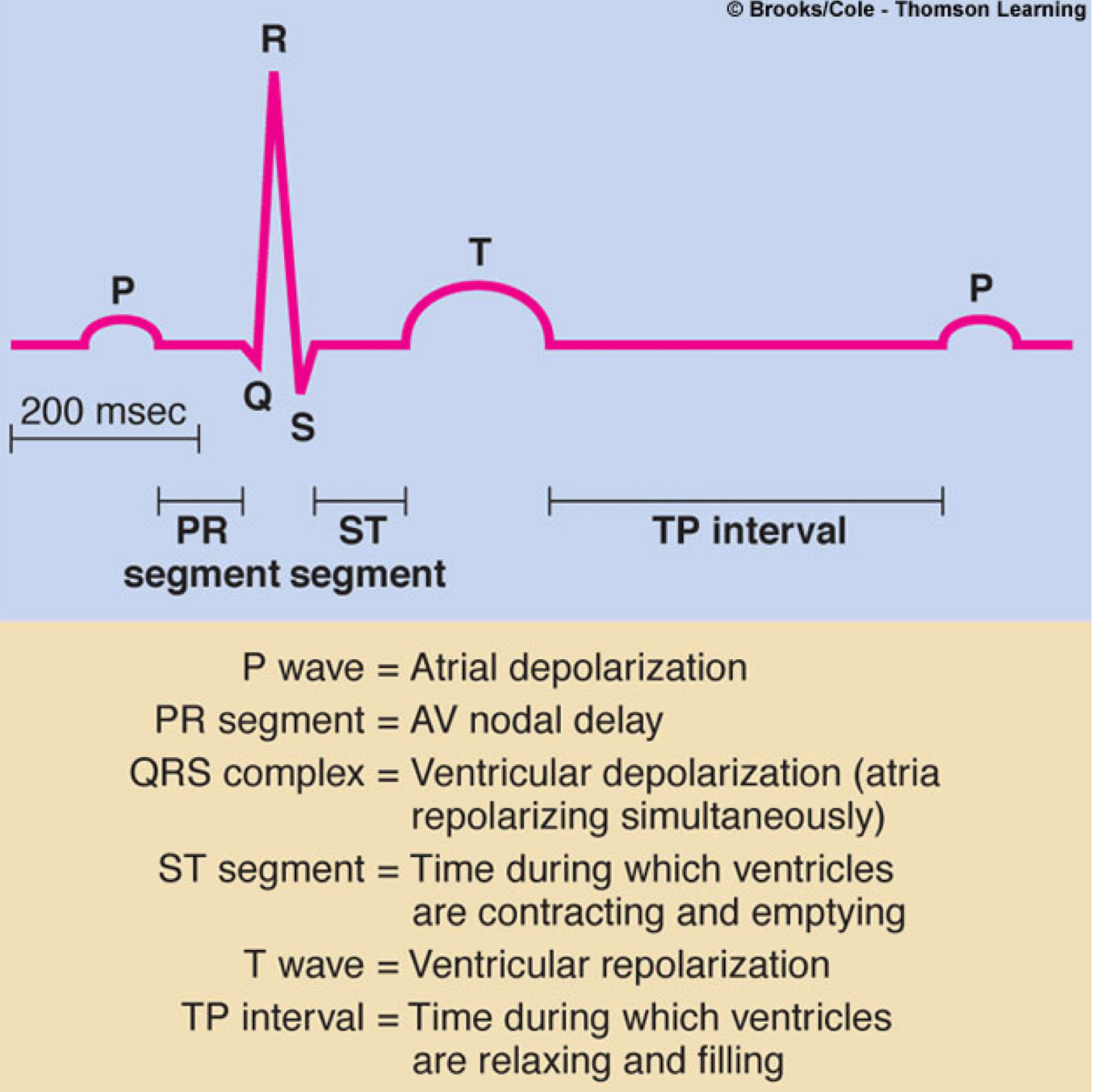
Draw and label the ECG.
If the SA node is not firing, what would you see (or not see) on the ECG and what would
the rate be?
absent p waves
What does the P wave on an ECG represent?
Atrial depolarization.
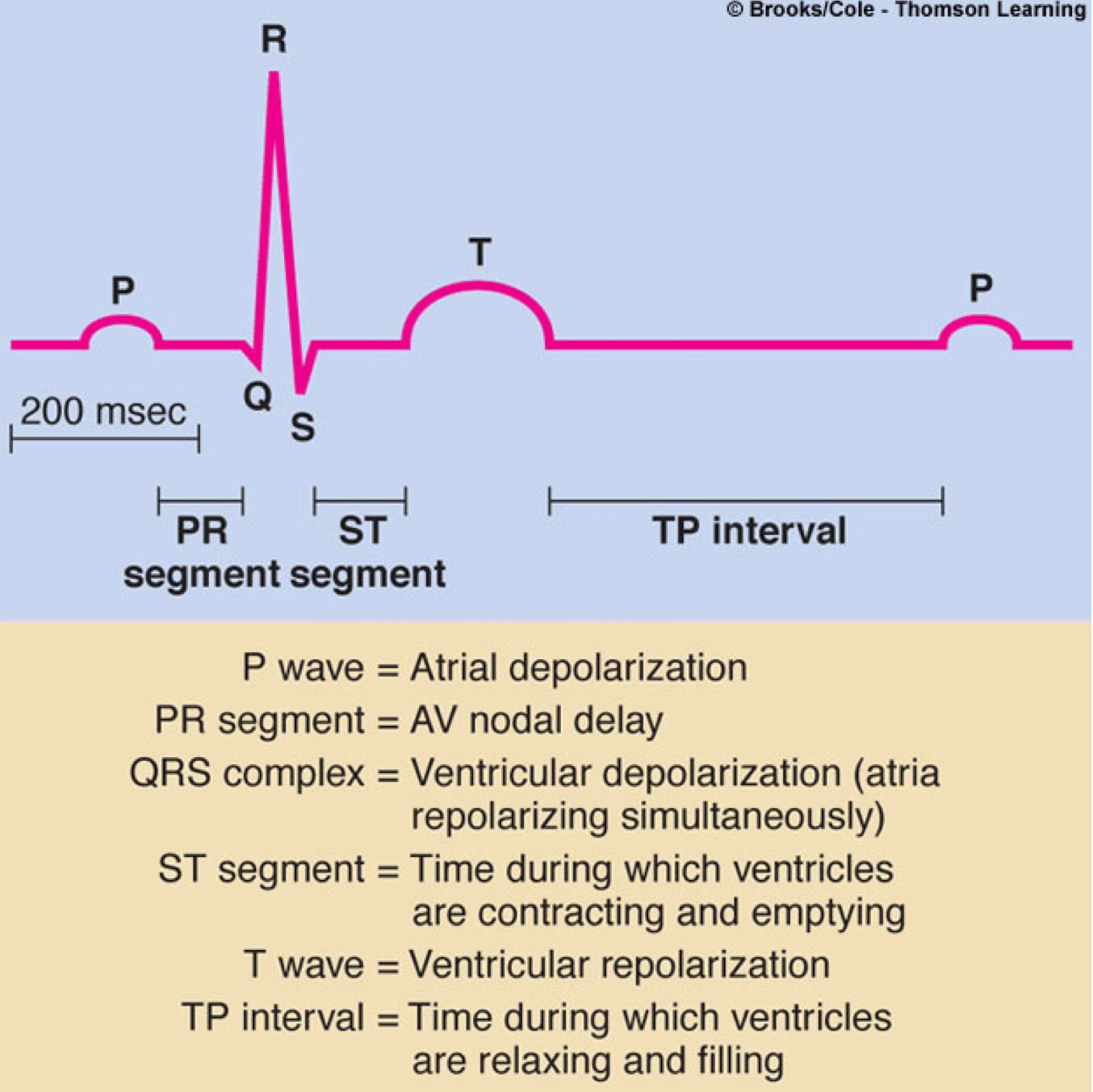
What does the QRS complex on an ECG represent?
Ventricular depolarization.
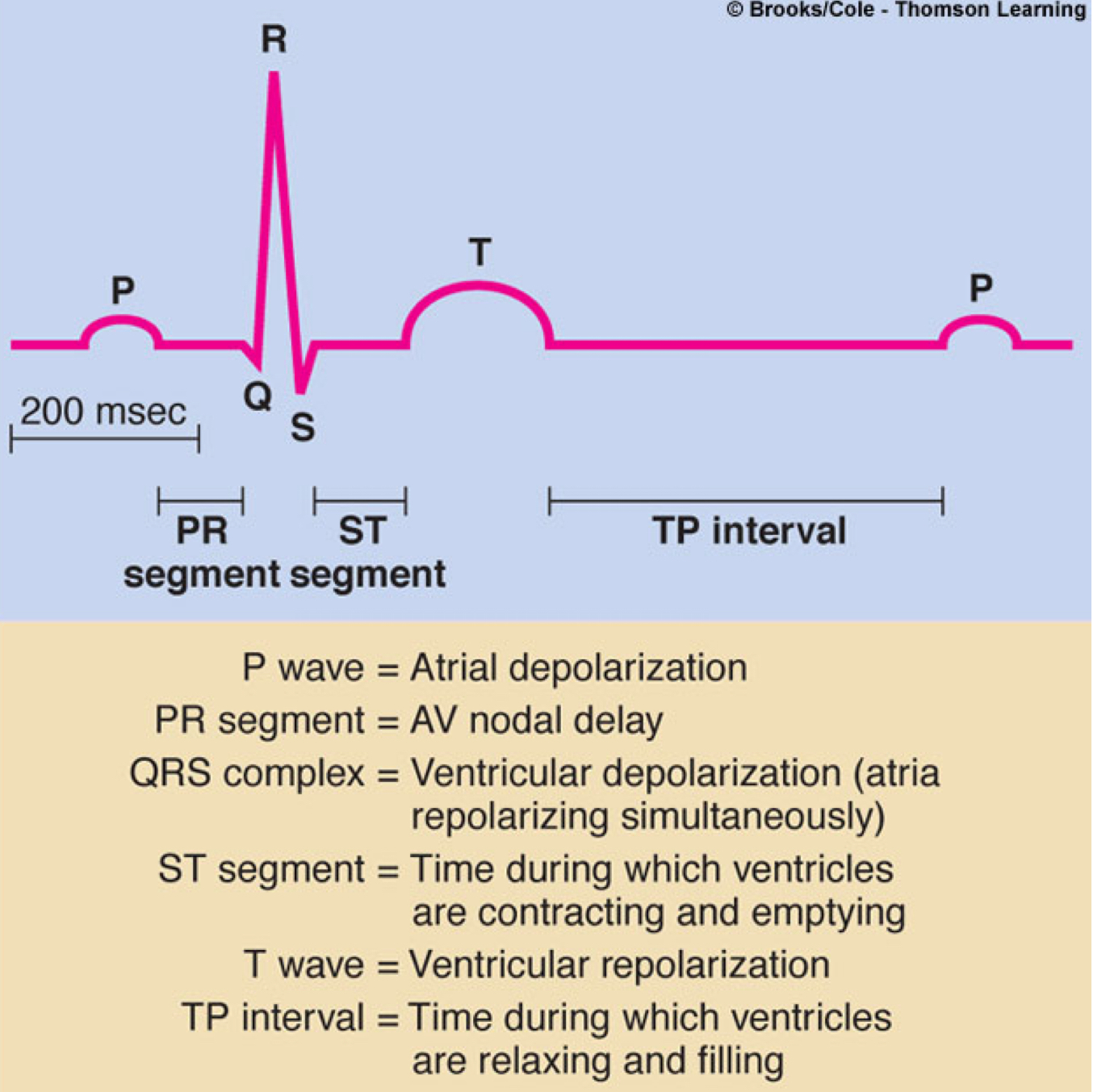
What does the T wave on an ECG represent?
Ventricular repolarization.
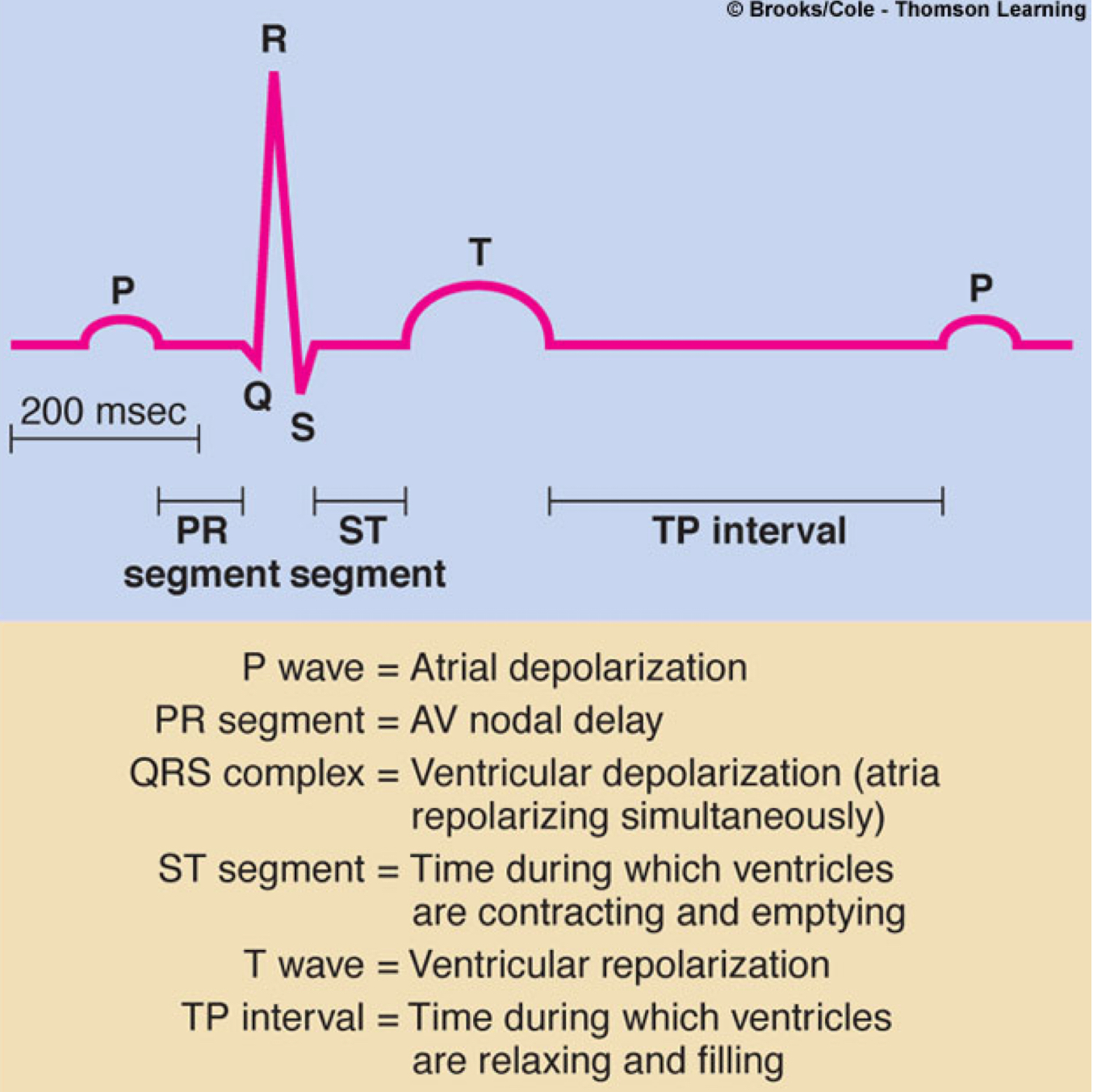
PR segment
AV node delay
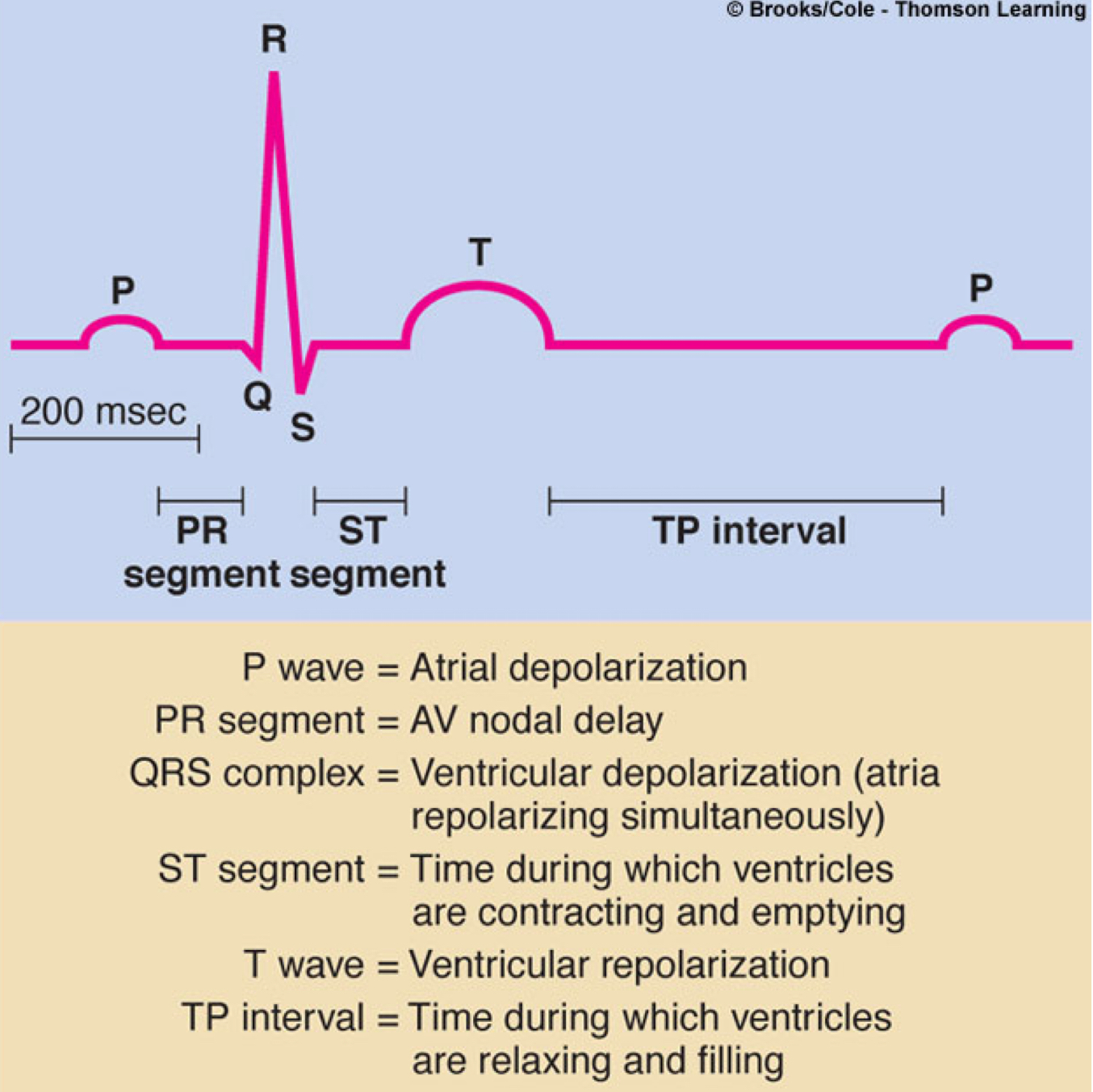
ST segment
time during which ventricles are contracting and emptying
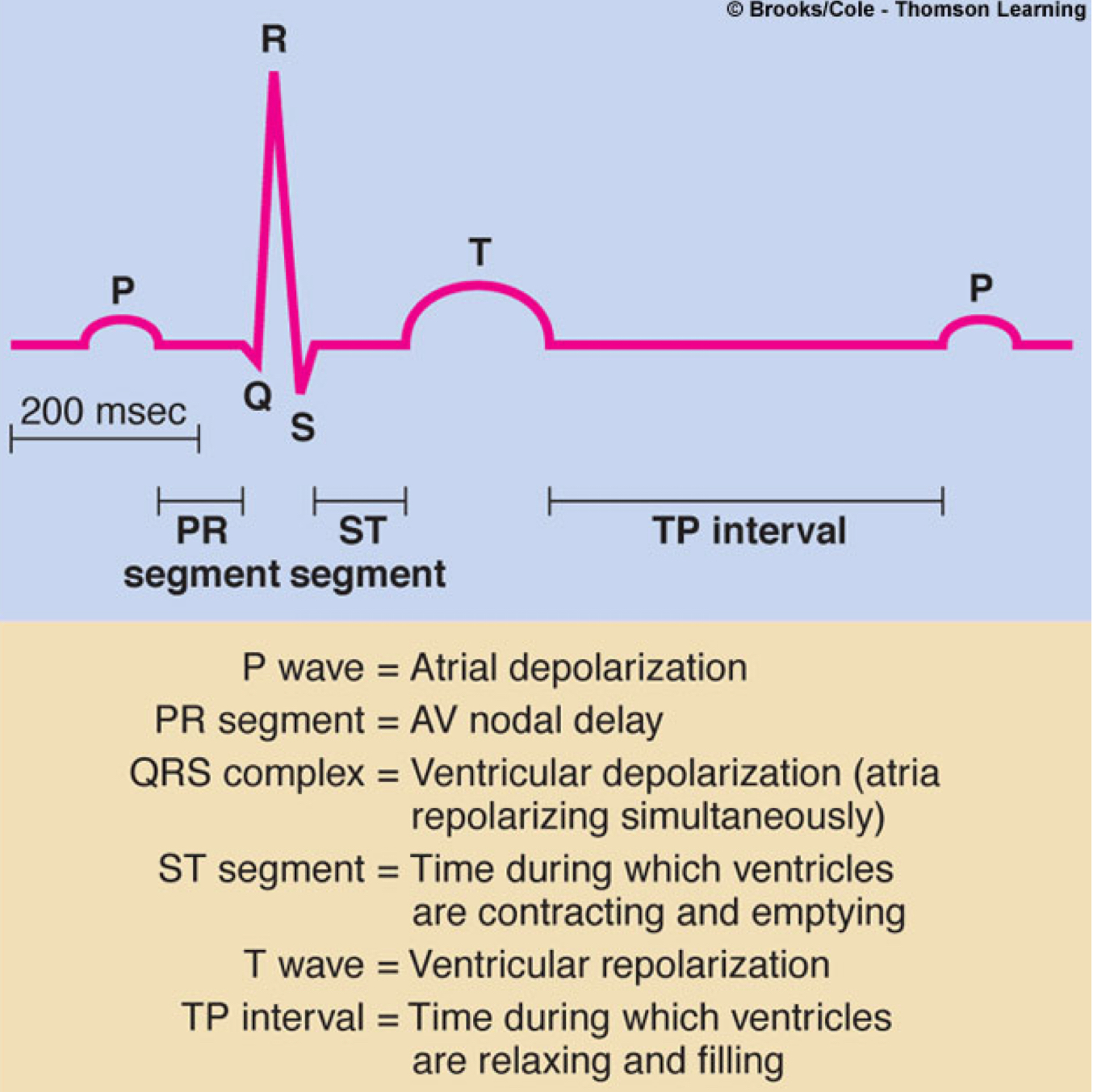
TP interval
time during which ventricles are relaxing and filling
How do electrical and mechanical events relate in the cardiac cycle?
Electrical signals trigger muscle contractions, coordinating blood flow through the heart.