CSDS 131 - Final Exam
1/218
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
219 Terms
Auricle
is the visible part of the ear that projects from the side of the head
consists of cartilage covered by skin and includes various structures: helix, antihleix, lobule, tragus
Helix
outer rim of the ear
Antihelix
a curved prominence parallel to the helix
Lobule
the fleshy lower part, commonly known as the earlobe
tragus
a small pointed eminence in front of the ear canal
Functions of the outer ear
sound collection
directionality
Sound collection
auricle gathers sound waves from the environment
Directionality
its unique shape helps localize sound sources by altering the intensity and timing of sound waves entering the ear canal
External auditory canal (EAC)
A slightly curved tube about 2.5cm long in adults
extends from the auricle to the tympanic membrane
Functions of the EAC
resonance
protections
Resonance
responds to sound waves by vibrating
Protection
Lined with hair and ceruminous glands producing earwax (cerumen) to trap dust and foreign particles
Tympanic Membrane (Eardrum)
a thin, semi-transparent membrane forming the boundary between the outer and middle ear
Composed of three layers—outer epithelial, middle fibrous, and inner mucosal.
Functions of the Tympanic Membrane
Vibration
Transmission
Vibration
responds to sound waves by vibrating
Transmission
transfers these vibrations to the ossicles in the middle ear, initiating auditory processing
Common Disorders of the Outer Ear
Congenital Malformations
Microtia
Anotia
Skin Cancer
EAC Disorders
Atresia
Stenosis
Foreign Bodies
Infections: Otitis Externa, Necrotizing Otitis Externa
Congenital Malformations
these are structural abnormalities present at birth
Microtia
Characteristics: an underdeveloped auricle, ranging from slight deformities to significant abnormalities
Associations: Can occur with syndromes like Down Syndrome or Treacher Collings Syndrome
Hearing Impact: may cause conductive hearing loss if the EAC or middle ear structures are affected
Treatment: otopasty (surgical reconstruction of the auricle), prosthetic auricles (for cosmetic enhancement and improved social interaction)
Anotia
Definition: complete absence of the auricle
Challenges: difficulty with sound localization due to the missing structure
Management: Prosthetic auricles (to improve appearance), hearing devices (bone-conduction hearing aids may be used if inner ear function is intact)
Skin Cancer
due to its exposure, the auricle is susceptible to skin cancers
Basal Cell Carcinoma
Prevalence: most common type of skin cancer on the auricle
Cause: Prolonged exposure to ultraviolet (UV) radiation
Role of Audiologists: early detection by recognizing suspicious lesions during examinations
Treatment: Surgical excision, radiation therapy, or topical medications
Atresia
Definition: Absence or closure of the EAC
Impact: leads to conductive hearing loss by blocking sound transmission
Treatment: Surgical Reconstruction (creating or opening the ear canal), Bone-conduction hearing aids (transmit sound directly to the inner ear)
Stenosis
Description: Narrowing of the EAC
Complications: can cause debris and cerumen buildup, increasing infection risk
Management: Regular cleaning (performed by healthcare professionals), surgical widening (in severe cases to restore normal canal size)
Foreign Bodies
Occurrence: commonly seen in children inserting objects into the ear
Symptoms: Pain, infection, or temporary hearing loss
Treatment: Professional removal to prevent damage to the ear canal or tympanic membrane
Otitis Externa (Swimmer’s Ear)
Cause: Bacterial or fungal infection from prolonged moisture exposure
Symptoms: itching, pain (especially when touching the ear), swelling, and discharge
Treatment: Topical Antibiotics/Antifungals (applied directly into the ear canal), Cleaning and Drying (keeping the ear cnaal dry to prevent recurrence)
Necrotizing Otitis Externa
Severity: a serious infection spreading to the skull base and surrounding bones
Risk factors: Diabetes, weakened immune system
Symptoms: Severe ear pain, especially at night, and possible cranial nerve involvement
Treatment: Systemic Antibiotics (often administered intravenously), hospitalizations (required for close monitoring and management)
Ossicular Chain
Components: malleus (hammer), incus (anvil), stapes (stirrup)
Function: amplify and transmit vibrations from the TM to the inner ear
Eustachian Tube
Connection: Links the middle ear to the nasopharynx
Functions: Pressure equalization (balances air pressure on both sides of the TM), protection (prevents retraction and damage to the TM)
Common middle ear disorders
eustachian tube dysfunction (ETD)
Otitis Media (Acute, Chronic, and Serous)
Cholesteatoma
Mastoiditis
Eustachian Tube Dysfunction (ETD)
Mechanism: failure of the eustachian tube to open properly
Causes: Allergies, upper respiratory infections, anatomical blockages
Symptoms: ear fullness, discomfort, mild conductive hearing loss
Diagnosis: Type C Tympanogram (indicates negative middle ear pressure)
Treatment: Autoinflation techniques (valsalva-exhaling with closed mouth and nose, Toynbee maneuvers-swallowing with nose pinched), Medications (decongestants and antihistamines to reduce inflammation)
Acute Suppurative Otitis Media
Description: Bacterial infection with pus in the middle ear
Symptoms: Severe ear pain, fever, possible purulent dischange if TM ruptures
Treatment: Antibiotics (to eliminate infection), Myringotomy with PE Tube Placement (drains fluid and ventilates the middle ear)
Chronic Otitis media
Characteristics: persistent inflammation causing structural damage
Complications: Tympanosclerosis (scarring), ossicular erosion leading to hearing loss
Management: Surgical repair or reconstruction of the ossicles and TM
Serous Otitis Media (SOM)
Also known as: otitis media with effusion
Cause: Non-infecious fluid due to prolonged ET dysfunction
Treatment: medications (decongestants to reduce fluid buildup), PE Tube Insertion (allows continuous drainage and ventilation)
Cholesteatoma
Definition: abnormal skin growth in the middle ear behind the TM
Risks: Can erode ossicles and mastoid bone, leading to serious complications
Treatment: Surgical removal (complete excision is necessary), follow-up (regular monitoring to prevent recurrence)
Mastoiditis
Description: Infection of the mastoid air cells in the temporal bone
Complications: can lead to meningitis, brain abscess if untreated
Treatment: Antibiotics (high-dose to combat infection), Mastoidectomy (surgical removal of infected bone
Types of Hearing loss
Hypacusis
Dysacusis
Diplacusis
Hypacusis
Definition: General reduction in hearing sensitivity
Impact: sounds must be louder to be heard
Dysacusis
Description: Difficulty in processing sounds, especially speech
Symptoms: Distortion or muffling of sounds, making comprehension challenging
Diplacusis
Explanation: perception of a single sound as two different pitches
Causes: Often due to unilateral cochlear damage
Genetic Causes of Inner Ear Disorders
Autosomal Dominant: only one defective gene needed; often a family history
Autosomal Recessive: Two copies of the defective gene required; parents may be carriers
X-linked Conditions: Gene mutation on the X chromosome; more severe in males
Maternal Infection causes of Inner Ear Disorders
Rubella: can cause congenital hearing loss if contracted during pregnancy
Cytomegalovirus (CMV): leading cause of non-genetic hearing loss in infants
Zika Virus: associated with microcephaly and potential auditory deficits
Ototoxic Medications during Pregnancy
Aminoglycosides: antibiotics like gentamicin can damage fetal inner ear structures
Specific Disorders that cause inner ear disorders
Ménière’s Disease
Presbycusis
Noise-Induced Hearing Loss (NIHL)
Ménière’s Disease
Symptoms: Vertigo, fluctuating low-frequency hearing loss, tinnitus, aural fullness.
Pathophysiology: Excessive endolymph fluid causing inner ear pressure.
Management: Dietary Changes (Low-sodium diet to reduce fluid retention), Medications (Diuretics, anti-vertigo drugs), Surgical Options (Endolymphatic shunt, vestibular nerve section in severe cases)
Presbycusis
Definition: Age-related sensorineural hearing loss.
Characteristics: Bilateral, gradual loss, especially of high-frequency sounds.
Management: Hearing Aids (Amplify sounds to aid hearing), Assistive Devices (Telephone amplifiers, alerting systems), Communication Strategies (Lip-reading, visual cues)
Noise-Induced Hearing Loss (NIHL)
Cause: Prolonged exposure to loud noises or sudden intense sounds.
Prevention: Use of ear protection like earplugs or earmuffs.
Audiogram Findings: “Acoustic trauma notch” at 3000–6000 Hz, indicating specific frequency loss
Central Auditory System
Functions: Processing complex auditory information—localization, discrimination, comprehension.
Components: Neural pathways from the cochlea to the auditory cortex in the brain.
Central Auditory Disorders
Auditory Neuropathy Spectrum Disorder (ANSD)
Auditory Processing Disorders (APD)
Acoustic Neuromas
Auditory Neuropathy Spectrum Disorder (ANSD)
Definition: Normal outer hair cell function but impaired neural transmission.
Diagnosis: ABR-Auditory Brainstem Response (Absent or abnormal responses), OAEs-Otoacoustic Emissions (Present, indicating normal cochlear outer hair cells)
Management: Hearing Aids/Cochlear Implants (May improve hearing by enhancing neural synchrony), Auditory Training (To improve processing skills)
Auditory Processing Disorder (APD)
Symptoms: Difficulty understanding speech, especially in noisy environments.
Diagnosis: Specialized auditory tests assessing different processing skills.
Management: Auditory Training Programs (Exercises to improve specific auditory abilities), Classroom Accommodations (Preferential seating, use of FM systems), Therapy (Speech-language therapy to develop compensatory strategies)
Acoustic Neuromas or vestibular schwannomas
Symptoms: Progressive unilateral hearing loss, tinnitus, balance problems.
Diagnosis: MRI (Imaging to detect tumors), ABR Testing (May show delayed neural responses)
Treatment: Surgical Removal (Via microsurgery), Radiation Therapy (For smaller tumors or when surgery isn’t an option)
Importance of Early Detection
Prevention of Delays: Early identification prevents speech, language, and cognitive delays.
Critical Development Window: The first three years are essential for auditory development
Newborn Screening Process
Universal Newborn Hearing Screening (UNHS):
Methods: Otoacoustic Emissions-OAEs (Tests cochlear function), Automated Auditory Brainstem Response-AABR (Assesses neural pathways up to the brainstem)
Follow-up Protocols:
By 1 Month: Initial screening completed.
By 3 Months: Diagnostic confirmation if screening is not passed.
By 6 Months: Intervention services initiated
Intervention
Hearing Aids: Fitted as early as possible for infants with hearing loss.
Cochlear Implants: Considered for severe to profound losses unresponsive to hearing aids.
Speech-Language Therapy: To support communication development.
Family Education: Involving parents in the intervention process enhances outcomes
Types of Hearing Aids
Behind-the-Ear (BTE): Components housed in a case behind the ear; suitable for most types of hearing loss.
Receiver-in-Canal (RIC): Similar to BTE but with the receiver placed in the ear canal.
In-the-Ear (ITE): Custom-made to fit the outer ear; less visible than BTE.
Completely-in-Canal (CIC): Fits deep inside the ear canal; nearly invisible
Advanced Features of Hearing Aids
Bluetooth Connectivity: Allows pairing with smartphones and other devices.
Noise Reduction: Reduces background noise for clearer hearing.
Tinnitus Masking: Provides relief by generating white noise or soothing sounds
Cochlear Implants (CIs)
Suitable For: Individuals with severe to profound sensorineural hearing loss.
Components:
External Processor: Captures and processes sound.
Internal Electrode Array: Surgically implanted to stimulate the auditory nerve.
Post-Surgical Needs:
Mapping: Customizing settings for optimal hearing.
Rehabilitation: Auditory training to interpret new sounds
Bone Anchored Hearing Aids (BAHA)
Indications: For conductive or mixed hearing loss and single-sided deafness.
Advantages: Bypasses Middle Ear-Directly stimulates the cochlea through bone conduction, Improved Clarity-Reduces distortion from middle ear pathology
Tinnitus Management
Sound Therapy: Uses background noise to mask tinnitus.
Tinnitus Retraining Therapy (TRT): Combines sound therapy with counseling to habituate the patient to tinnitus.
Cognitive-Behavioral Therapy (CBT): Addresses the emotional response to tinnitus
Vestibular Disorders Rehabilitation Techniques
Balance Retraining: Exercises to improve balance and coordination.
Gaze Stabilization: Enhances control of eye movements during head motion.
Specific Maneuvers:
Epley Maneuver: Repositions displaced ear crystals in BPPV patients.
Brandt-Daroff Exercises: Performed at home to reduce vertigo symptoms
Hearing conservation
Purpose: Prevent Noise-Induced Hearing Loss (NIHL) in hazardous noise environments.
California Regulations: Governed by Cal/OSHA to enforce workplace safety standards
Hearing Conservation Regulatory Framework
Key Cal/OSHA Sections (Title 8, Sections 5096–5100):
5096: Noise exposure limits (5 dBA exchange rate halves exposure time).
5097–5100: Cover Hearing Conservation Programs, Hearing Protectors, Training, and Recordkeeping.
Exposure Limits:
Permissible Exposure Limit (PEL): 90 dBA over 8 hours.
Action Level (AL): ≥85 dBA requires conservation measures.
California standards exceed federal OSHA enforcement rigor.
Components of Hearing Conservation Program
Noise Monitoring: Regular assessments; results must be communicated to employees.
Audiometric Testing: Baseline within six months; annual tests to track hearing thresholds.
Hearing Protection Devices (HPDs): Provided for noise above AL; training on proper use required.
Training and Education: Annual instruction on noise effects, HPDs, and audiometric testing.
Recordkeeping: Noise data retained for two years; audiometric results for the duration of employment.
Engineering Controls: Noise barriers, quieter machinery.
Administrative Controls: Shift rotations to reduce exposure
Implementation Challenges
Diverse Workforce: Multilingual and multi-ethnic workplaces require tailored outreach.
Enforcement: Cal/OSHA inspections ensure compliance; non-compliance risks fines or restrictions.
Innovative Solutions: Adoption of advanced noise control technologies prioritizes employee wellness
Benefits of Hearing Conservation
Prevents Hearing Loss: Reduces risks of NIHL, tinnitus, and related stress.
Economic Impact: Saves workers’ compensation costs and improves productivity.
Legal and Ethical Compliance: Protects employers from lawsuits and demonstrates commitment to safety
Case Study: Construction Site Compliance
Scenario: Noise levels exceeded 95 dBA.
Actions Taken: Engineering controls (quieter machinery) and audiometric testing detected hearing loss in 10% of employees, enabling early interventions.
Outcome: Improved compliance and employee safety.
Normal Hearing dB HL
-10 dB HL to 25 dB HL
Mild Hearing Loss dB HL
30 dB HL to 40 dB HL
Moderate Hearing Loss dB HL
45 dB HL to 55 dB HL
Moderately-Severe Hearing Loss dB HL
60 dB HL to 70 dB HL
Severe Hearing Loss dB HL
75 dB HL to 90 dB HL
Profound Hearing Loss dB HL
90 dB HL+
Tympanogram AS
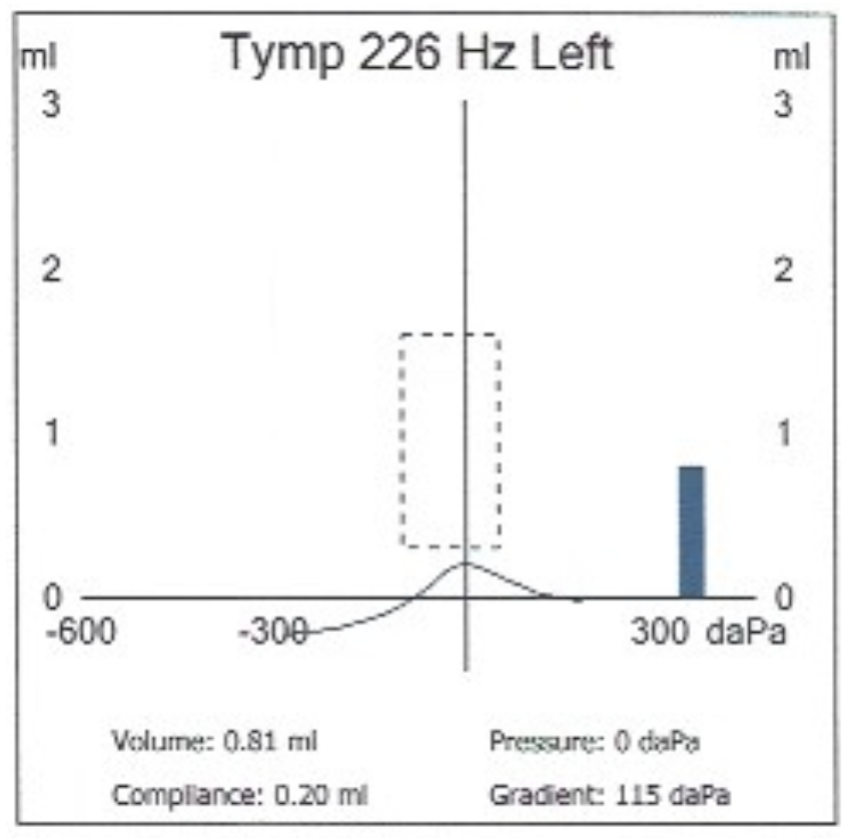
Shallow peak → stiff system (otosclerosis)
Tympanogram A
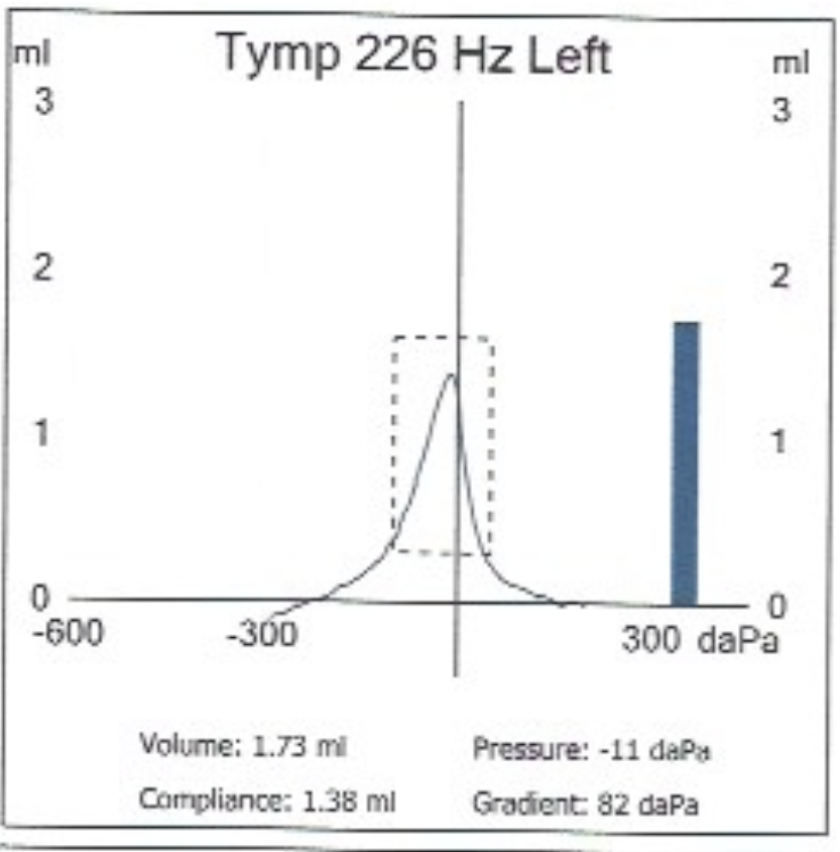
Normal compliance and pressure
Tympanogram AD
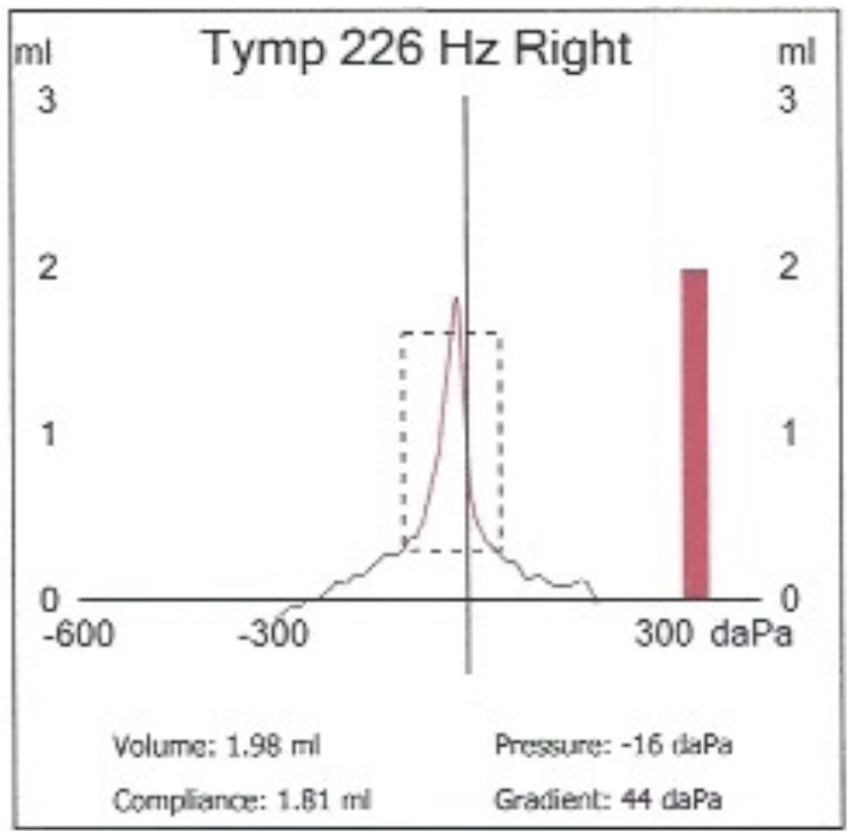
Deep peak → hypermobile membrane or ossicular discontinuity
Tympanogram B
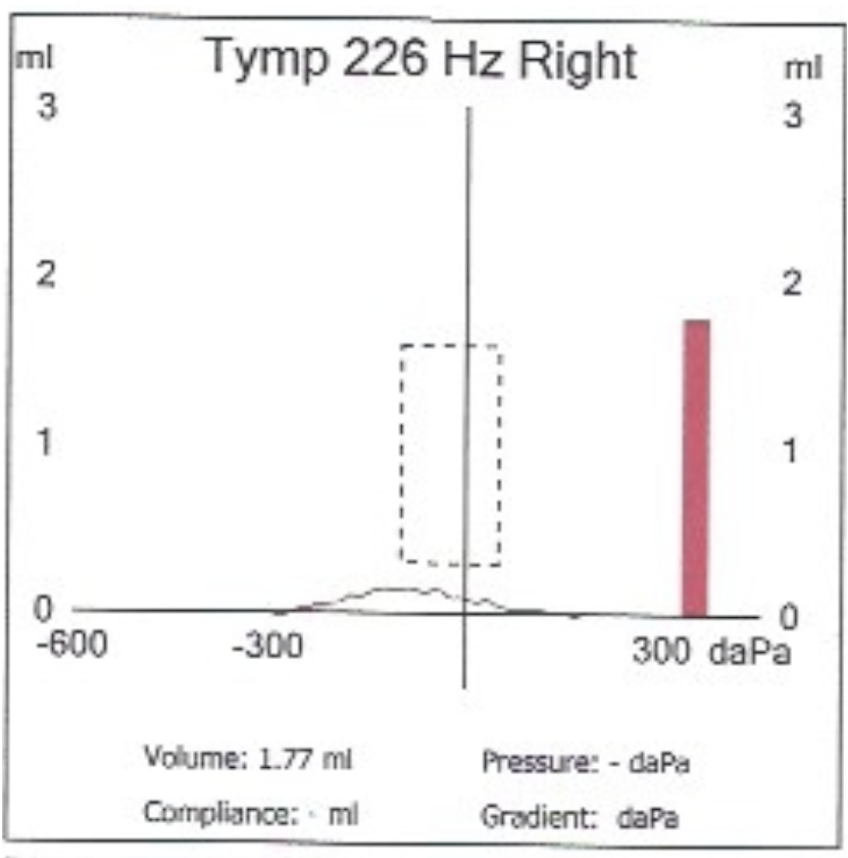
Flat → fluid, perforation, or wax occlusion
Tympanogram C
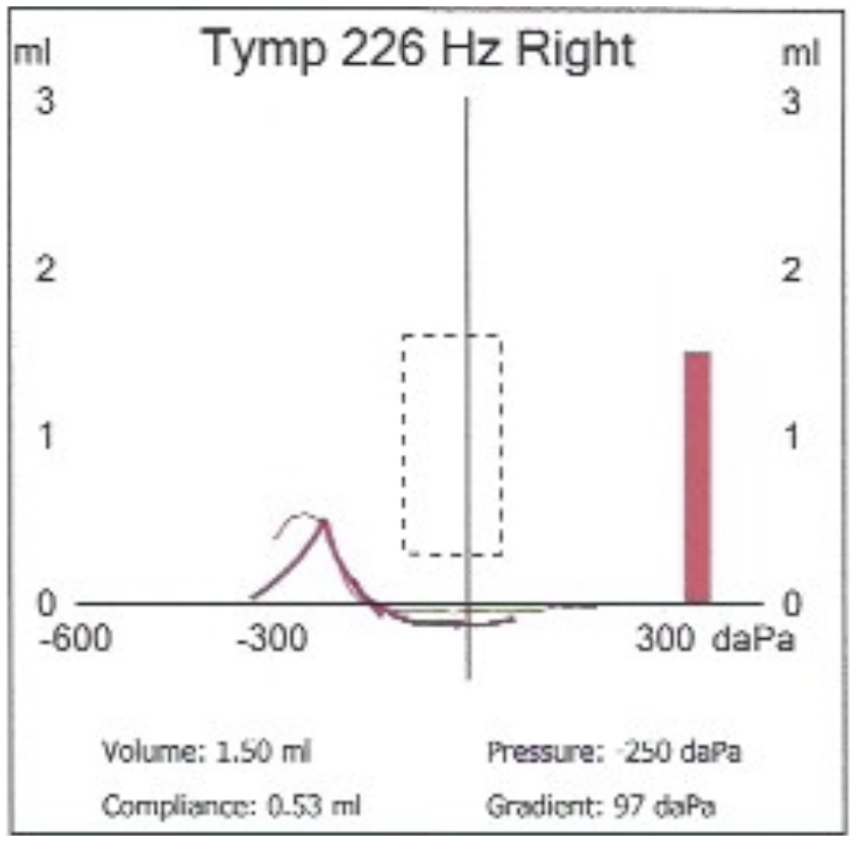
Negative pressure → eustachian tube dysfunction
How to straighten the ear canal in Otoscopy for adults
Pull ear back and up
How to straighten the ear canal in Otoscopy for kids
downward and back
Impedance (Z)
resistance to sound flow caused by stiffness (S), mass (M), and friction (R)
Determine stiffness
Admittance (Y)
ease of sound flow; inverse of impedance
Determine flaccidity
Compliance
mobility of the tympanic membrane and ossicular chain
Acoustic Reflex
a loud sound trigger stapedius muscle contraction, which stiffens the ossicular chain and protects the cochlea from overexposure
Absent or reflexes may suggest neural lesions or middle ear pathology
Acoustic Reflex Thresholds Ipsilateral Reflex
A sound in one ear triggers a reflex in the same ear
Acoustic Reflex Thresholds Contralateral Reflex
A sound in one ear triggers a reflex in the opposite ear, crossing over in the brainstem via the superior olivary complex
False Negatives in Pure Tone Audiometry
These occur when the patient fails to response to a sound they actually heard. This can be due to misunderstanding instructions, poor attention, or deliberate feigning (faking)
False Positives in Pure Tone Audiometry
These happen when the patient responds to a sound that wasn’t presented. Highly motivated patients or those with tinnitus may inadvertently give false-positive responses (trigger happy patients)
Stenger Principle
If I play the same tone in both ears you are only going to perceive the louder one
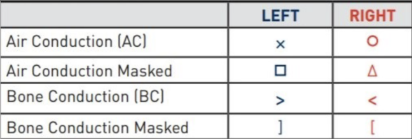
Audiogram Symbols
Air-bone gap (ABG)
is the difference in decibels (dB) between air and bone conduction thresholds. A significant ABG (≥ 15 dB) indicates a conductive component. No gap indicates sensorineural loss
Interaural Attenuation
loss of sound energy between ears
Supra-aural earphones have a minimum IA of 40 dB
Insert earphones: 60-75 dB
Bone conduction: 0 dB
Overview of Otoscopy
The process of visually examining the ear canal and tympanic membrane (eardrum) using an otoscope. It is one of the most fundamental diagnostic techniques in audiology and otolaryngology, used to assess ear health before any audiometric testing
Why does otoscopy matter?
The outer and middle ear are often the first places where pathologies can interfere with sound conduction.
Performing accurate otoscopy ensures that earwax impaction, infection, or perforation is identified before misinterpreting an audiogram or tympanogram.
Otoscope parts:
handle (power source), light source, magnifying lens, and speculum (disposable tip)
Traditional otoscope
handheld, commonly used in clinics
Video otoscope
projects a magnified image onto a screen for documentation or patient education
Speculum size
choose small for children, larger for adults to visualize the canal walls
Otoscopy Procedure Steps
1. Inspect the external ear for deformities, swelling, or discharge.
2. Straighten the ear canal
3. Gently insert the speculum and view the tympanic membrane.
4. Note color, cone of light, and any abnormalities