Anatomy and Physiology II - Section 4, Lesson 5
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
What is Glomerular Filtration Rate (GFR)?
the speed at which fluid passes out of the blood and into the glomerular capsule. All renal corpuscles in the kidneys contribute to GFR.
how is GFR measured/estimated?
measured as the amount of glomerular filtrate produced (fluid entering the glomerular capsule) per minute.
What may influence GFR?
Changes in various physiological parameters, especially blood pressure
Changes in various physiological parameters, especially blood pressure, can influence GFR. Can a fairly constant GFR be maintained?
through a variety of mechanisms, the kidneys are able to adapt to maintain a fairly constant GFR even in the face of large variations in mean arterial blood pressure (MABP) between around 80 and 180 mmHg.
through a variety of mechanisms, the kidneys are able to adapt to maintain a fairly constant GFR even in the face of large variations in mean arterial blood pressure (MABP) between around 80 and 180 mmHg. What are some ways of this?
1. Blood flow into and out of the glomeruli
2. Surface area of the glomerular capillary
through a variety of mechanisms, the kidneys are able to adapt to maintain a fairly constant GFR even in the face of large variations in mean arterial blood pressure (MABP) between around 80 and 180 mmHg. One way is Blood flow into and out of the glomeruli. how is this?
Constriction and dilation of the afferent and efferent arterioles can alter the flow of blood into the glomeruli, thus regulating GFR. Constriction of the afferent arterioles decreases the flow of blood and thus decreases GFR, whereas dilation of the afferent arterioles increases the flow of blood, thus increasing GFR.
through a variety of mechanisms, the kidneys are able to adapt to maintain a fairly constant GFR even in the face of large variations in mean arterial blood pressure (MABP) between around 80 and 180 mmHg. One way is Surface area of the glomerular capillary. What does this mean?
Filtration occurs more efficiently over a larger surface area. Therefore, if the surface area of the glomerular capillaries is increased, GFR will also increase, and vice versa.
What are glomeruli
blood vessels that filter waste and extra fluids from blood
how is GFR maintained?
Blood flow to the kidney is kept at a fairly constant level
How is the continued production of urine, the cleansing of the blood, and the maintenance of the blood salt and waste concentrations allowed, regardless of intake?
The balance between filtration, reabsorption, and secretion
What is is the collective name given to the internal mechanisms of the kidney that help maintain constant GFR?
Renal regulation (intrinsic control)
There are two mechanisms involved in renal autoregulation. What are they?
myogenic autoregulation (or the “myogenic mechanism”) and tubuloglomerular autoregulation (or “tubuloglomerular feedback”)
There are two mechanisms involved in renal autoregulation: myogenic autoregulation (or the “myogenic mechanism”) and tubuloglomerular autoregulation (or “tubuloglomerular feedback”). Which is faster?
The myogenic mechanism acts much more quickly than the tubuloglomerular mechanism.
It is vital that the flow of blood through the kidney be at a suitable rate to allow for filtration. What does this rate determine?
how much solute is retained or discarded, how much water is retained or discarded, and, ultimately, the osmolarity of blood and the blood pressure of the body.
The kidneys are very effective at regulating the rate of blood flow over a wide range of blood pressures. What is an example of this?
Your blood pressure will decrease when you are relaxed or sleeping. It will increase when exercising. Yet, despite these changes, the filtration rate through the kidney will change very little.
The kidneys are very effective at regulating the rate of blood flow over a wide range of blood pressures. Why?
due to two internal autoregulatory mechanisms that operate without outside influence: the myogenic mechanism and the tubuloglomerular feedback mechanism.
What does myogenic mechanism regulating blood flow within the kidney depend on?
a characteristic shared by most smooth muscle cells of the body. When you stretch a smooth muscle cell, it contracts; when you stop, it relaxes, restoring its resting length. This mechanism works in the afferent arteriole that supplies the glomerulus. When blood pressure increases, smooth muscle cells in the wall of the arteriole are stretched and respond by contracting to resist the pressure, resulting in little change in flow. When blood pressure drops, the same smooth muscle cells relax to lower resistance, allowing a continued, even flow of blood.
What does the tubuloglomerular feedback mechanism involve
the JGA and a paracrine signaling mechanism utilizing ATP, adenosine, and nitric oxide (NO).
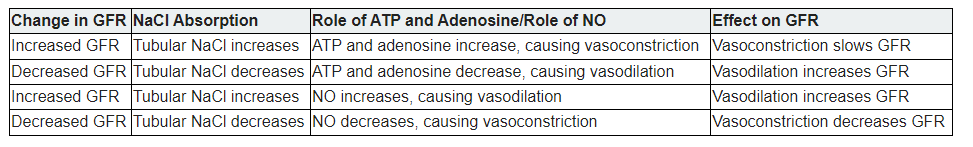
The tubuloglomerular feedback mechanism involves the JGA and a paracrine signaling mechanism utilizing ATP, adenosine, and nitric oxide (NO). What does this mechanism stimulate
either contraction or relaxation of afferent arteriolar smooth muscle cells
tubuloglomerular feedback mechanism :As GFR increases, there is less time for NaCl to be reabsorbed in the PCT. What type of osmolarity does this result in?
higher osmolarity in the filtrate
tubuloglomerular feedback mechanism: the DCT is in intimate contact with the afferent and efferent arterioles of the glomerulus. How does the fluid flow rate and Na+ concentration affect
Specialized macula densa cells in this segment of the tubule respond to changes in the fluid flow rate and Na+ concentration affect
Q: Tubuloglomerular feedback mechanism – What structure senses Na⁺ concentration and flow rate in the DCT?
A: The macula densa cells.
Q: Tubuloglomerular feedback mechanism – What happens to NaCl reabsorption in the PCT when GFR increases?
A: There’s less time for reabsorption, so more NaCl reaches the DCT.
Q: Tubuloglomerular feedback mechanism – How do macula densa cells respond to high NaCl and fast flow?
A: They release ATP and adenosine.
Q: Tubuloglomerular feedback mechanism – What do ATP and adenosine do to the afferent arteriole?
A: They cause it to constrict, reducing GFR.
Q: Tubuloglomerular feedback mechanism – What happens when GFR is too low?
A: Less Na⁺ reaches the macula densa → less ATP and adenosine → afferent arteriole dilates → GFR increases.
Q: Tubuloglomerular feedback mechanism – What role does nitric oxide (NO) play in this feedback?
A: NO causes the afferent arteriole to relax, fine-tuning the effect of ATP and adenosine.
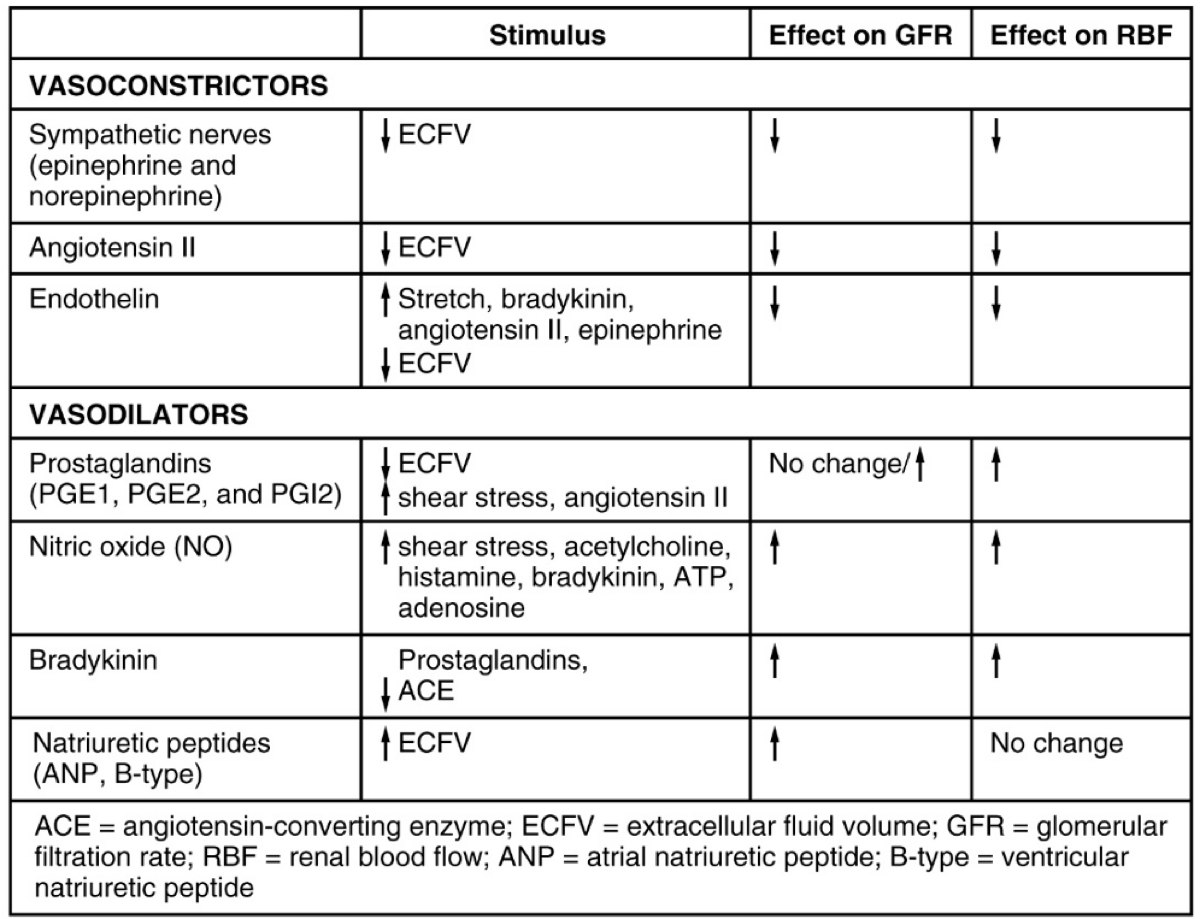
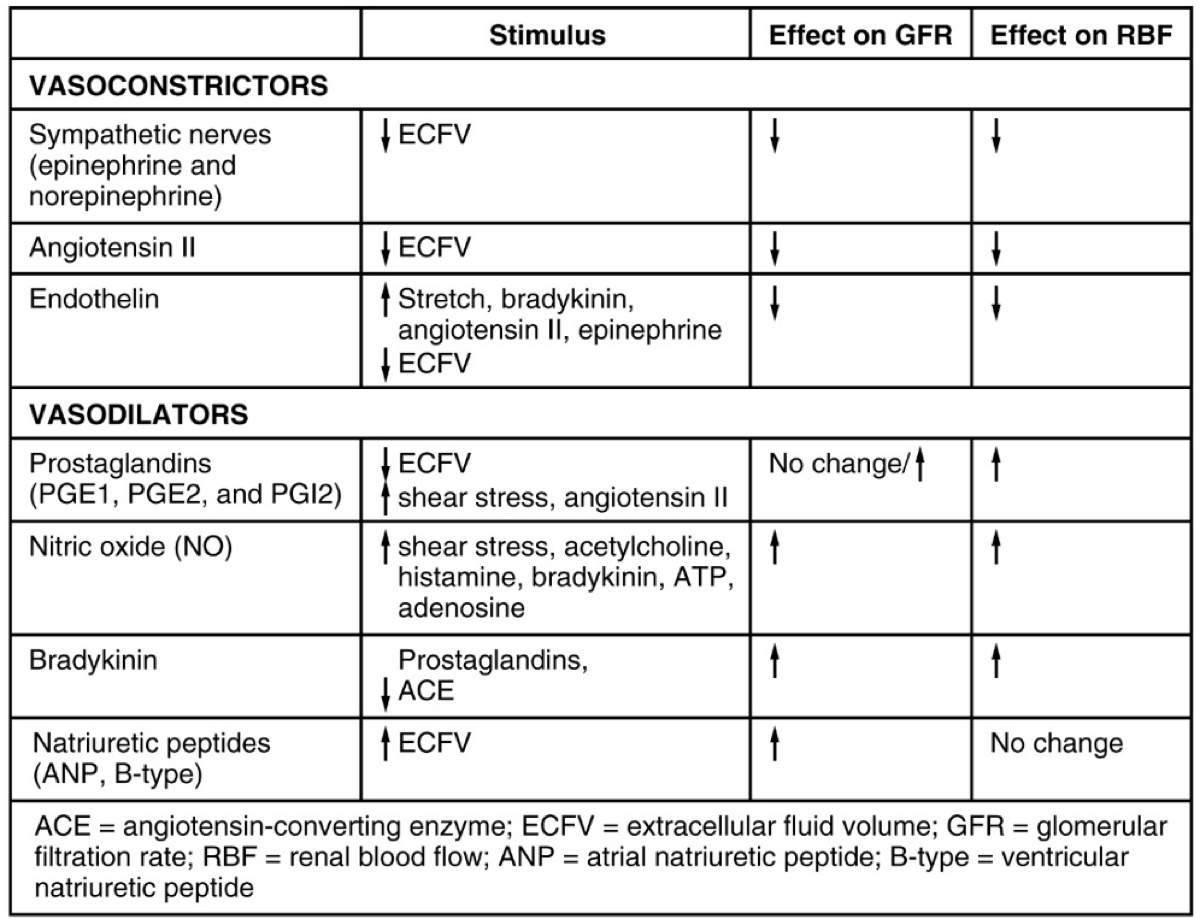
Q: What are the two major hormones involved in the extrinsic regulation of glomerular filtration rate (GFR)?
A: Angiotensin II and atrial natriuretic peptide (ANP).
Q: How do angiotensin II and ANP function in relation to each other?
A: They are functional antagonists—angiotensin II increases GFR, while ANP decreases it.
Q: What nervous system provides input to the glomeruli?
A: The sympathetic nervous system.
Q: What is the difference between endocrine and paracrine hormone action in kidney regulation?
A: Endocrine hormones act from a distance via the bloodstream; paracrine hormones act locally near their site of release.
Q: What is the role of angiotensin II in kidney function?
A: It constricts efferent arterioles to maintain GFR and increases reabsorption of sodium and water.
Q: What is the role of atrial natriuretic peptide (ANP) in kidney function?
A: It dilates afferent arterioles, increases GFR, and promotes sodium and water excretion.
Q: What enzyme is produced by juxtaglomerular (JG) cells in response to low extracellular fluid volume?
A: Renin
Q: What does renin do in the bloodstream?
A: Converts angiotensinogen (from the liver) into angiotensin I.
Q: What enzyme converts angiotensin I to angiotensin II, and where is it primarily located?
A: Angiotensin-converting enzyme (ACE), primarily in the lungs and on endothelial surfaces.
Q: What are the main effects of angiotensin II?
A: Vasoconstriction, reduced GFR and renal blood flow, and stimulation of aldosterone release.
Q: What is aldosterone, and where is it produced?
A: A mineralocorticoid hormone produced by the adrenal cortex.
Q: What does aldosterone do in the kidneys?
A: Promotes Na⁺ reabsorption and K⁺ excretion in the nephron.
Q: What hormone is released by the posterior pituitary to conserve water?
A: Antidiuretic hormone (ADH)
Q: How does ADH promote water reabsorption?
A: By inserting aquaporins into collecting duct cells, allowing water to move by osmosis.
Q: What do diuretics do in terms of kidney function?
A: Increase urine output by inhibiting solute and water reabsorption.
Q: What are endothelins, and where are they produced in the kidney?
A: Powerful vasoconstrictors made by endothelial cells, mesangial cells, and DCT cells.
Q: What stimulates the release of endothelin?
A: Angiotensin II, bradykinin, and epinephrine.
Q: What is the effect of endothelin in diabetic kidney disease?
A: It causes sodium retention and reduces GFR by damaging podocytes and constricting arterioles.
Q: What is the function of natriuretic peptides like ANH and BNP?
A: Promote sodium and water excretion by inhibiting aldosterone and ADH.
Q: Where is atrial natriuretic hormone (ANH) produced and why?
A: In the atria of the heart in response to overstretching from high blood pressure or volume.
Q: How does ANH increase GFR?
A: By dilating afferent arterioles and constricting efferent arterioles.
Q: What hormone is a diagnostic marker of congestive heart failure and why?
A: BNP, due to its longer half-life and cardiac origin.
Q: What is parathyroid hormone (PTH) released in response to?
A: Low blood calcium levels.
Q: What does PTH do in the kidneys?
A: Stimulates calcitriol synthesis and promotes phosphate excretion to raise blood Ca²⁺.
Q: What effect does low sympathetic activity have on the kidneys?
A: It causes vasodilation of afferent arterioles, increasing renal blood flow and GFR.
Q: What neurotransmitter causes vasoconstriction of the afferent arterioles during stress?
A: Norepinephrine from sympathetic nerves.
Q: What hormone does the adrenal medulla release during stress and what is its effect on the kidneys?
A: Epinephrine; it causes generalized vasoconstriction, including of the afferent arterioles, reducing kidney blood flow
Q: Why does the body reduce blood flow to the kidneys during stress?
A: To redirect blood to more immediately vital organs like the brain and muscles.
Q: How do sympathetic nerves respond to a drop in blood pressure?
A: They stimulate renin release from juxtaglomerular cells.
Q: What are the downstream effects of renin release?
A: Renin converts angiotensinogen to angiotensin I, which is converted to angiotensin II by ACE.
Q: What are the effects of angiotensin II on the body and kidneys?
A: It causes vasoconstriction and stimulates aldosterone release to retain Na⁺ and water, increasing blood pressure.
Q: How much pressure across the glomerulus is needed to maintain normal GFR?
A: Only about a 10 mm Hg pressure differential.
Which statement about the Renin-Angiotensin-Aldosterone System is true?
Angiotensin I stimulates the release of atrial natriuretic peptide.
Aldosterone promotes water excretion.
Angiotensin II is a potent vasoconstrictor.
ACE converts angiotensinogen to angiotensin I.
correct
Angiotensin I stimulates the release of atrial natriuretic peptide. ANP is used by the body to combat high blood pressure and thus would not be released as part of the renin cascade.
Q: What is the osmolarity of glomerular filtrate?
A: 300 mOsm/L, the same as blood plasma.
Q: What is the osmolarity range of dilute urine?
A: As low as 65–70 mOsm/L.
Q: What is the osmolarity range of concentrated urine?
A: As high as 1200 mOsm/L.
Q: What hormone is absent when dilute urine is formed?
A: Antidiuretic hormone (ADH).
Q: Why does urine become dilute in the absence of ADH?
A: The collecting ducts are impermeable to water; water is not reabsorbed, and some solutes are.
Q: What hormone is present when concentrated urine is formed?
A: Antidiuretic hormone (ADH).
Q: What does ADH do to collecting duct cells?
A: Inserts aquaporin-2 channels, making them permeable to water.
Q: Why does urine become concentrated in the presence of ADH?
A: Water is reabsorbed into the interstitial fluid, increasing urine osmolarity.
Which actions would result in an increase in glomerular filtration rate?
Choose 2 answers.
Dilation of the afferent arterioles
Constriction of the afferent arterioles
Increased surface area of the glomerular capillaries
Sympathetic nervous stimulation
Dilation of the afferent arterioles
Reason: Dilation of the afferent arterioles increases blood flow into the glomerulus, increasing pressure and GFR.
Increased surface area of the glomerular capillaries
Reason: A larger surface area allows for more filtration to occur, which increases GFR.
Which hormone acts by inhibiting aldosterone release and inhibiting sodium ion recovery in the collecting ducts?
Endothelin
Renin
Natriuretic
Aldosterone
Natriuretic
What is the mechanism whereby macula densa cells monitor Na+ concentration in the terminal portion of the ascending loop of Henle and act to cause vasoconstriction or vasodilation of afferent and efferent arterioles?
Myogenic mechanism
Renin-aldosterone mechanism
Tubuloglomerular feedback mechanism
Atrial natriuretic mechanism
Tubuloglomerular feedback mechanism
Which hormone directly opposes the actions of natriuretic hormones?
Angiotensin II
Nitric oxide
Dopamine
Melatonin
Angiotensin II
Renin is released in response to which homeostatic imbalance?
ACE
Increased blood pressure
Diuretics
Decreased blood pressure
Decreased blood pressure
What would be a consequence of having no aquaporin channels in the collecting duct?
A person would retain excess Na+.
A person would develop systemic edema.
A person would suffer severe dehydration.
A person would lose vitamins and electrolytes.
A person would suffer severe dehydration.
Which hormone would be expected to increase with dehydration or low blood volume?
Aldosterone
ANH
Erythropoietin
ADH
ADH
What would be a consequence of renin secretion?
Urinary output would decrease
Urinary output would not change
Atrial natriuretic hormone would increase
Vasodilation would occur
Urinary output would decrease
How does an increase in renin secretion change urine concentration?
Renin has no effect on urine concentration.
Renin will stimulate release of aldosterone, and urine will be concentrated.
Renin will stimulate release of aldosterone, and urine will be diluted.
Renin will stimulate release of ADH, and urine will be diluted.
Renin will stimulate release of aldosterone, and urine will be concentrated.