ENS 265 Exam 4 Important concepts SDSU F19
1/120
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
121 Terms
1. Which area of the brain is responsible for coordination; balance; motor learning, control, and integration?
A. Brain Stem
B. Cerebellum
C. Frontal Lobe
D. Occipital Lobe
B. Cerebellum
2. Which of the following meninges is the outermost layer next to the skull?
A. Periosteum
B. Piamater
C. Duramater
D. Arachnoid
C. Duramater
3. This term identifies that a brain injury has been sustained on the same side of impact.
A. Coup
B. Contracoup
C. Intracoup
D. Intercoup
A. Coup
4. A Concussion may produce which of the following Signs and Symptoms?
1. Dizziness
2. Bruising behind the ears (battle sign) or eyes (raccoon eyes)
3. Headache
4. Increased blood pressure
A. 1, 2, & 3 B. 1 and 3 C. 2 and 4 D. 4 only E. all of the above
B. 1 and 3 (dizziness and headache)
5. Which of the following tests determines eye tracking?
A. H-test
B. PERL
C. Rhomberg test
D. SAC test
A. H-test
6. An athlete is following the Return to Play Guidelines after sustaining a concussion. He is performing sport specific exercise as part of Stage 3, and begins to show symptoms of headache and dizziness. What is the recommend next step?
A. Progress to Stage 4 immediately with Dr. supervision
B. Return to Stage 2 until symptom-free for 24 hours, then progress to Stage 3 again.
C. Rest for 48 hours, then begin Stage 4- regardless of symptoms
D. Skip Stage 4 and go to Stage 5
B. Return to Stage 2 until symptom-free for 24 hours, then progress to Stage 3 again.
7. Which heat illness is caused by the loss of fluid and electrolytes in sweat and presents with headache, moist-sweaty skin, weakness and fatigue?
A. Heat Rash
B. Heat Cramps
C. Heat Exhaustion
D. Heat Stroke
C. Heat Exhaustion
8. What is the recommended IMMEDIATE treatment for Heat Exhaustion?
A. Stretch muscles
B. Move to cooler area and elevate feet
C. Ice bath
D. Ice burrito
B. Move to cooler area and elevate feet
9. As a lightning storm is passing through, at what point should the athletes and fans seek safe shelter?
A. When the "Flash-to-Bang" count is 30 seconds or less
B. When the "Flash-to-Bang" count indicates the storm is less than 30 miles away
C. 30 minutes after the last sound of thunder or lightning
D. 30 seconds after it starts raining
A. When the "Flash-to-Bang" count is 30 seconds or less
10. Which of the following elements must be present in order for a Negligence case to have merit?
1. Duty of care
2. Breach of duty (tort)
3. Causation
4. Harm
A. 1, 2, & 3 B. 1 and 3 C. 2 and 4 D. 4 only E. all of the above
E. all of the above
(1. Duty of care
2. Breach of duty (tort)
3. Causation
4. Harm)
11. TRUE or FALSE. When managing risk, preparation is KEY. Having an emergency action plan and established policies and procedures is essential for reducing risk.
True
12. Which of the following viruses is a blood borne pathogen that we have no vaccination for, but begins to die immediately outside the body, and is not viable in dried blood?
A. HIV- human immunodeficiency virus
B. AIDS- acquired immune deficiency syndrome
C. HBV- hepatits B virus
D. HAV- hepatitis A virus
A. HIV- human immunodeficiency virus
13. TRUE or FALSE. Hepatitis B and HIV may be found in blood or body fluids ONLY, and NOT in sweat, tears, saliva, vomit, and urine.
TRUE
14. Where should blood soiled/bloody gauze be discarded?
A. Biohazardous waste bag
B. Recycling trash container
C. Sharps container
D. Paper sack
E. Garbage disposal
A. Biohazardous waste bag
15. Which of the following is an ADVANTAGE of paper medical records?
A. Expensive
B. Requires little to no training
C. Allows for immediate document sharing and viewing across systems
D. Provides for ease of access and on-screen comparisons of medical data
B. Requires little to no training
Concussion the movie
· Dr. Bennet Nigerian forensic pathologist
· First discovered Chronic Traumatic encephalopathy (CTE) in an American FB player in 2002
· During autopsy reported on Mike Webster, steelers, after he committed suicide
· Led to publication in 2005 in journal of neurosurgery
· NFL called for retraction of paper as falsification
· 2009 when NFL finally acknowledged the connection
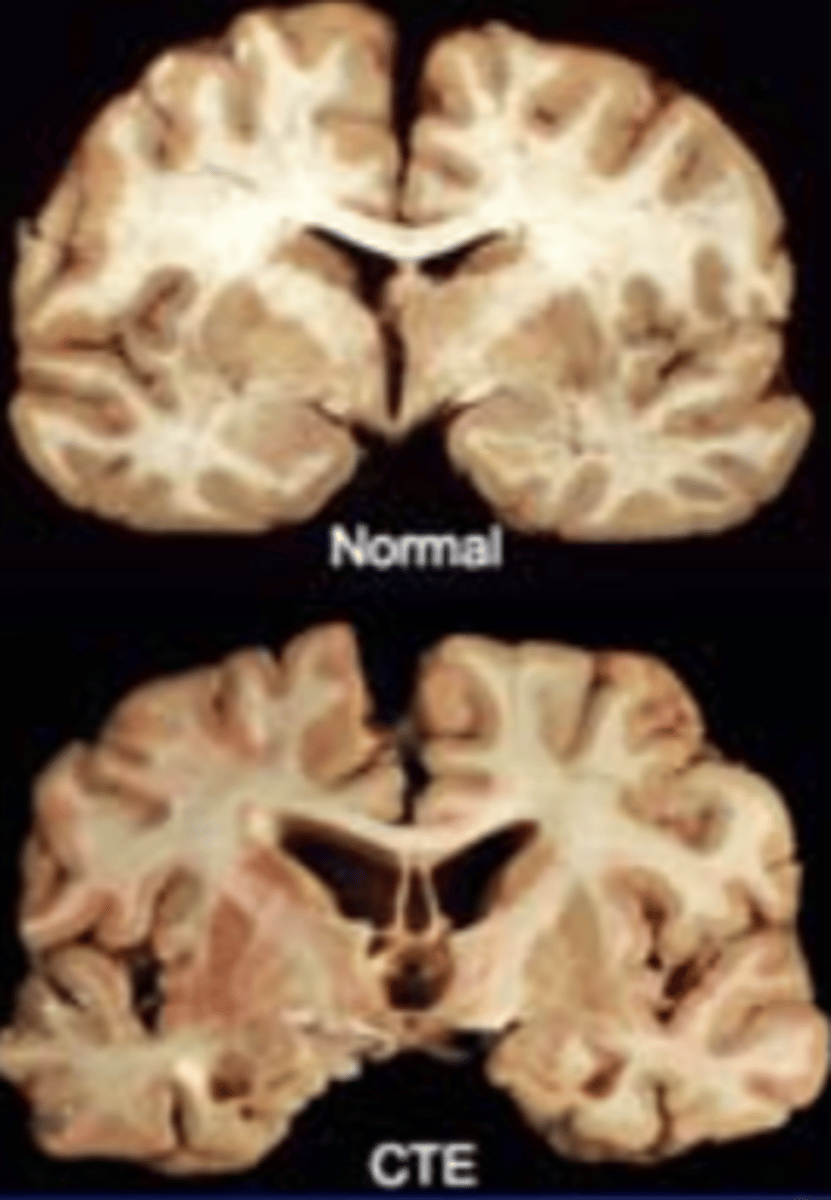
What is CTE?
· Chronic Traumatic Encephalopathy- Multiple mild traumatic brain injuries (mTBI = concussions)
o "A progressive neuro-degenerative disease of the brain found in athletes (& others) with a history of repetitive brain trauma, including symptomatic concussions as well as asymptomatic sub-concussive hits to the head."
· First reported and cited in Boxers in late 1920's
o "Punch Drunk Syndrome"
Other documented cases of CTE
• 2011 article on CTE in War Veterans
• 2007 study reported 17% of British boxers in 1930-50's show evidence of CTE
• NHL- 28 y/o Derek Boogard- accidental overdose of alcohol & oxycodone following several documented concussions.
• NHL- 27 y/o Rick Rypien- known as "pound for pound- best fighter". Battled depression for 10 yrs, then suicide
• Several other former NHL players showed strong link between concussions and mental illness, i.e. depression, anxiety, drug/alcohol abuse, dementia, suicide
--> Boston Brain Bank established in 2008- of the donated/examined 14 brains of deceased NFL players, 13 were diagnosed with CTE
What can we do to spot/prevent CTE?
• Recognize the signs & symptoms of repeated concussions (TBI) AND brain degeneration:
• Memory loss
• Confusion
• Impaired judgment
• Impaired cognitive processing & concentration
• Impulse control
• Aggression/Irritability
• Paranoia
• Depression
• Dementia
• Properly prevent and manage concussions
• Follow return to play guidelines
• ATHLETE/COACH EDUCATION CAMPAIGNS
• Heads Up
• Speak Up
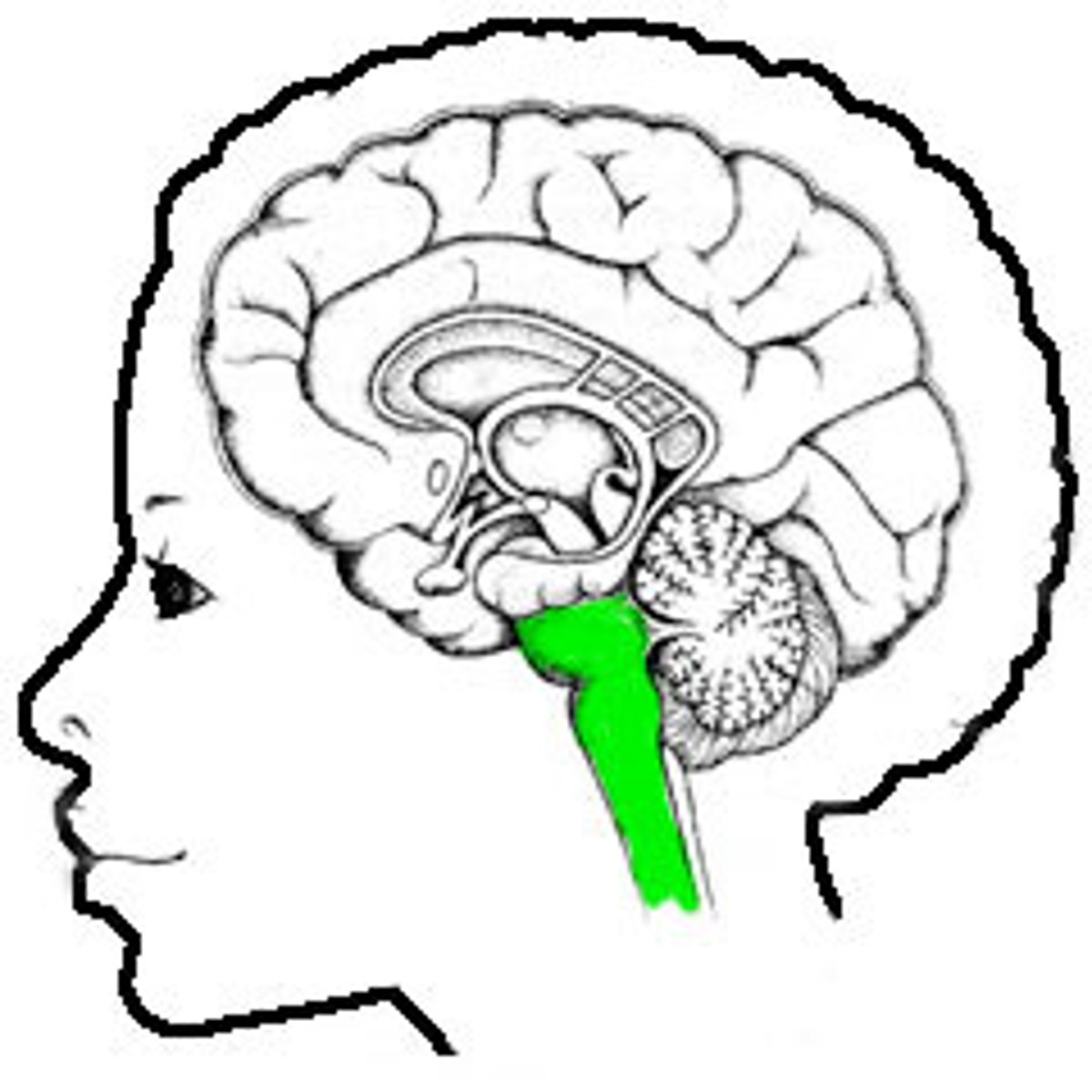
brain stem
respiration, heart rate and vital center
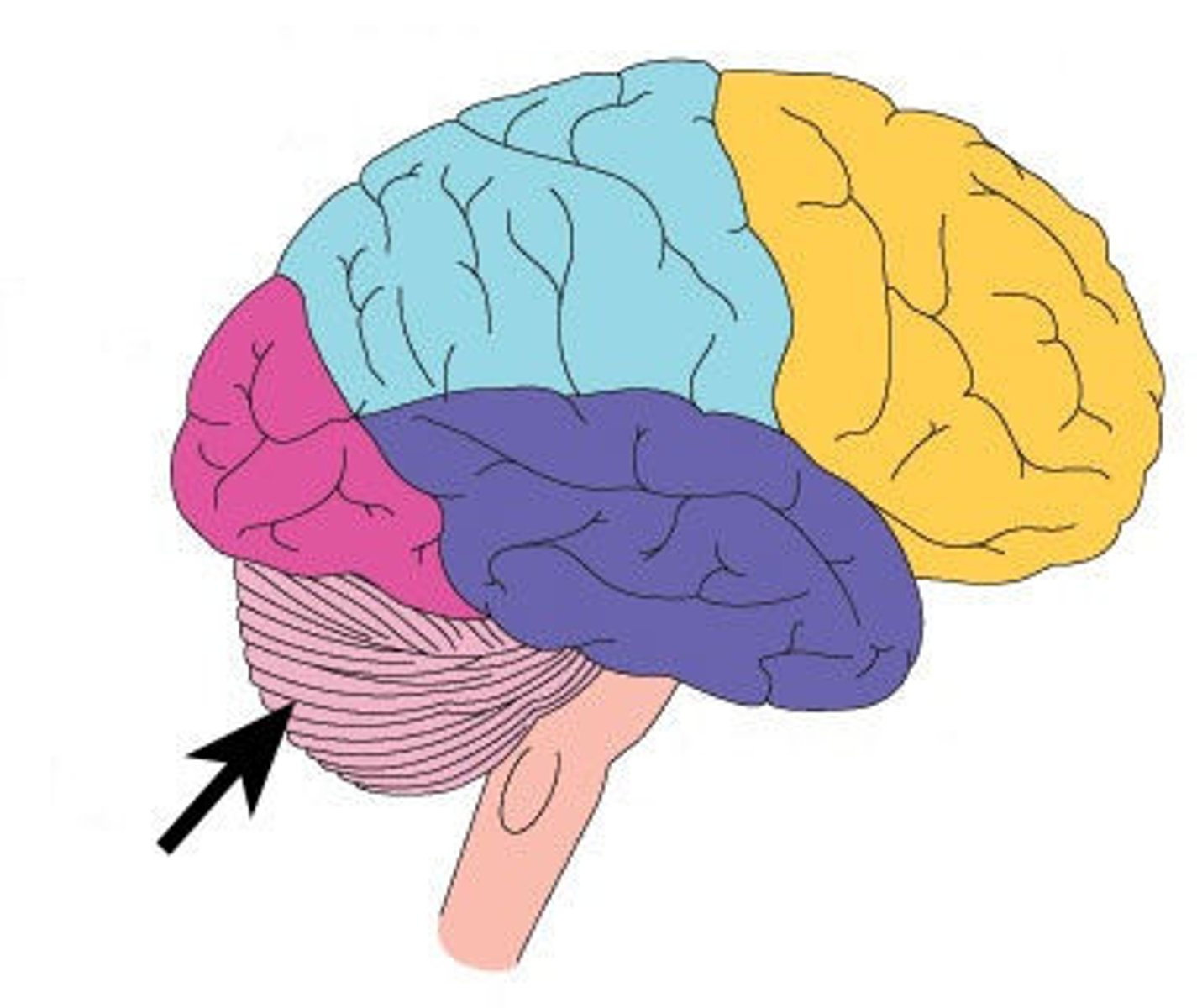
Cerebllum
- coordination; balance; motor learning, control, and integration
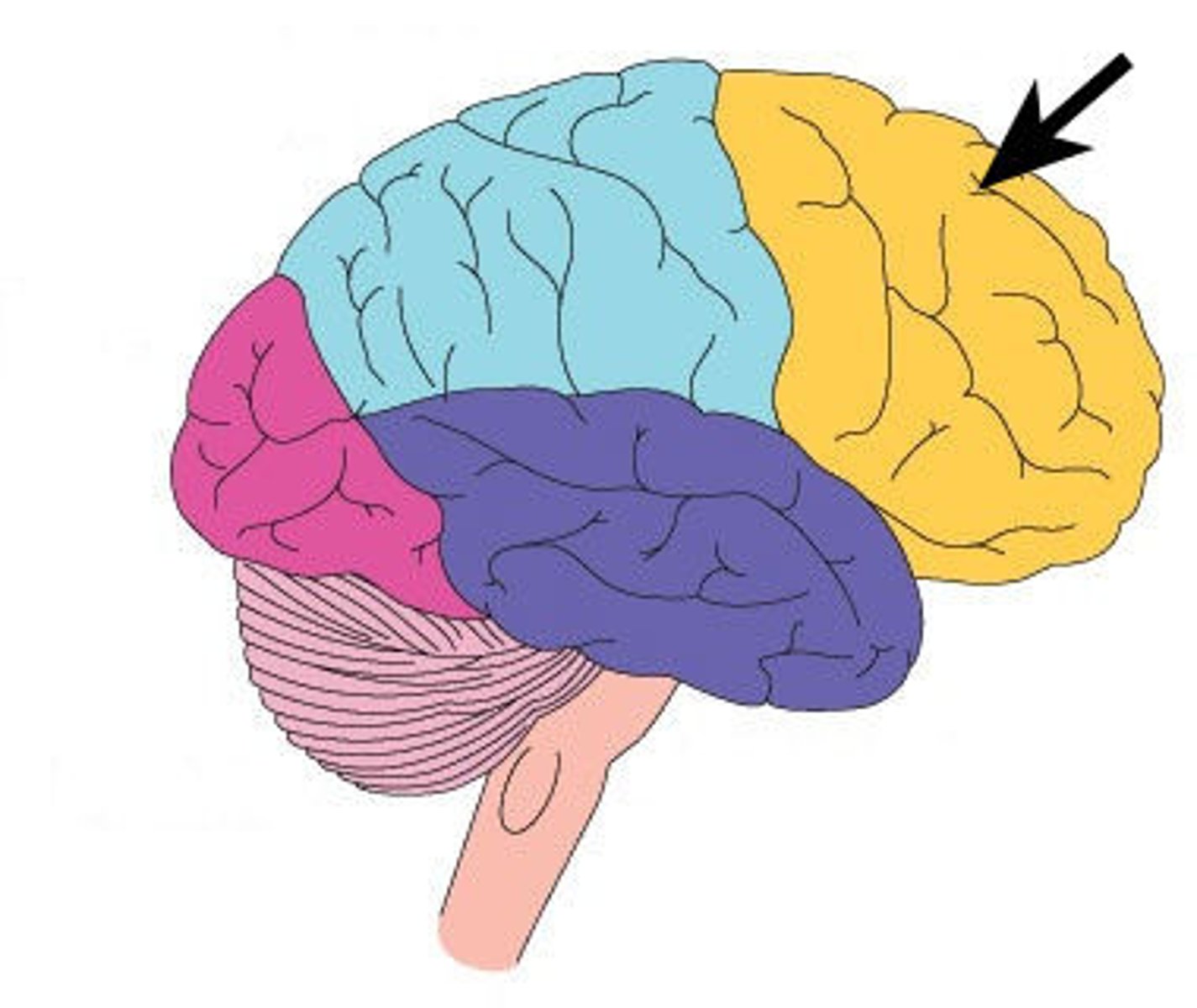
frontal lobe
- emotional control; personality; language; judgment; impulse control
parietal lobe
• sensation; visual sensory input; perception
occipital lobe
• visual center
temporal lobe
auditory; long-term memory; language; sexual behavior
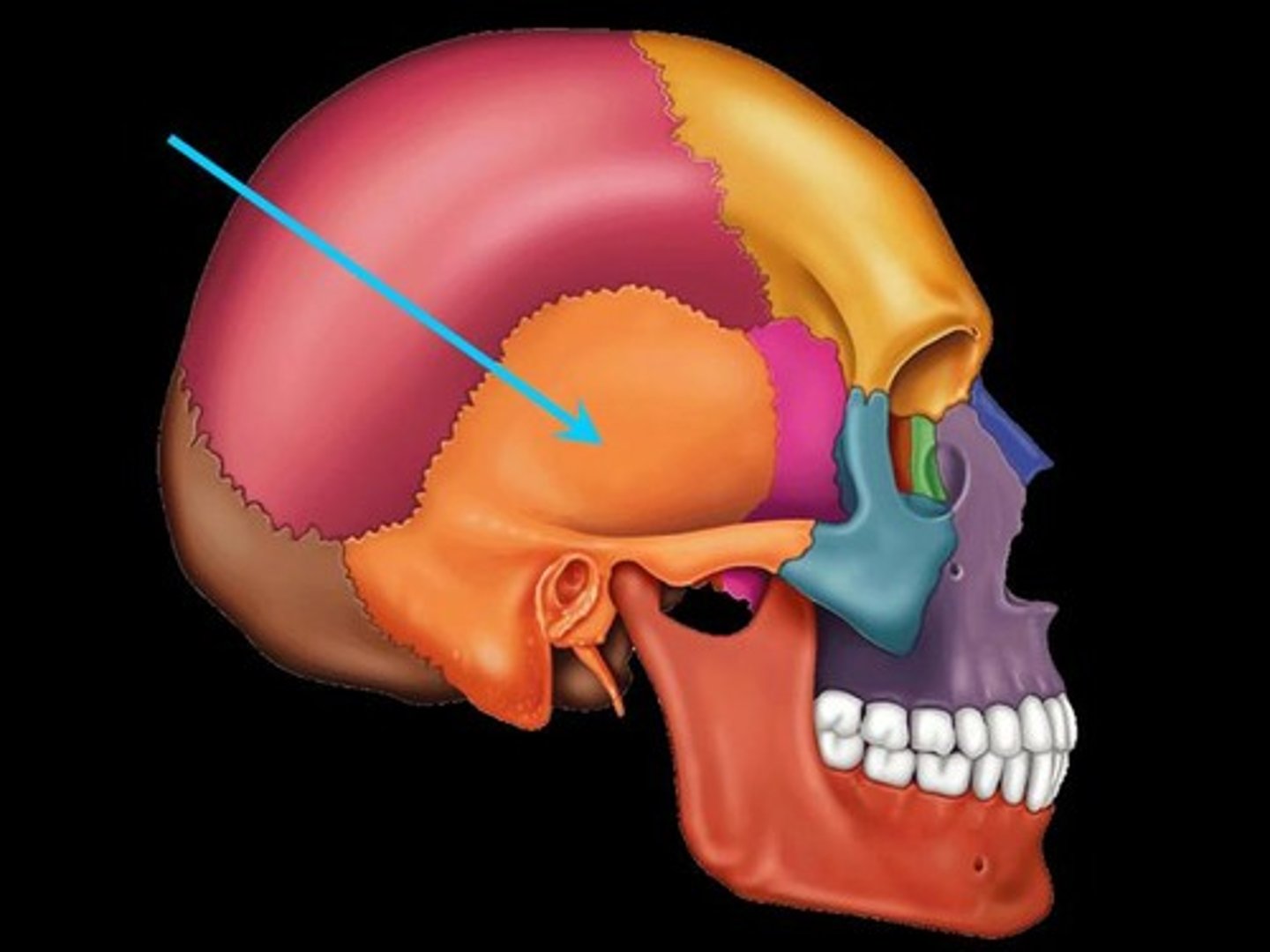
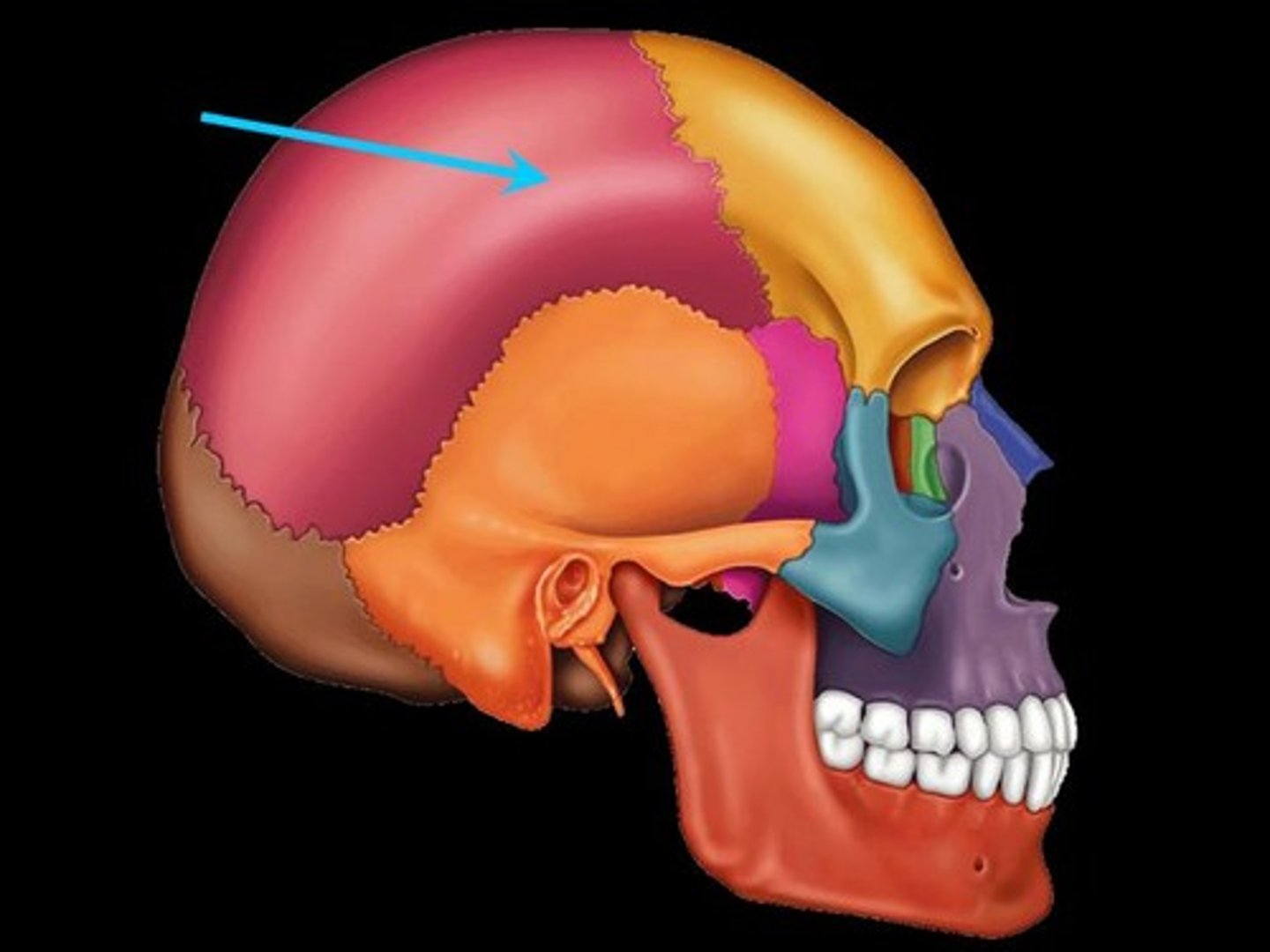
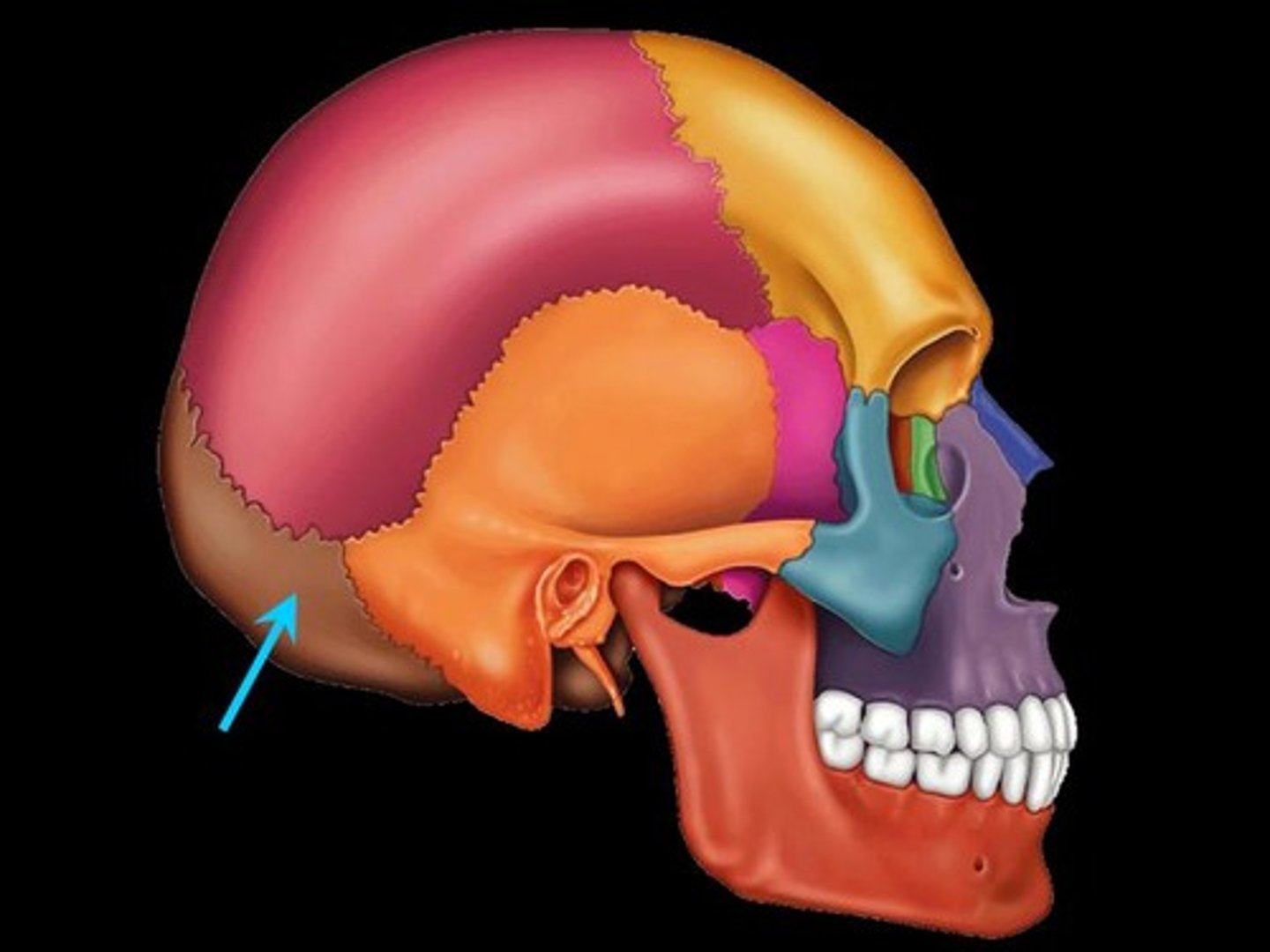
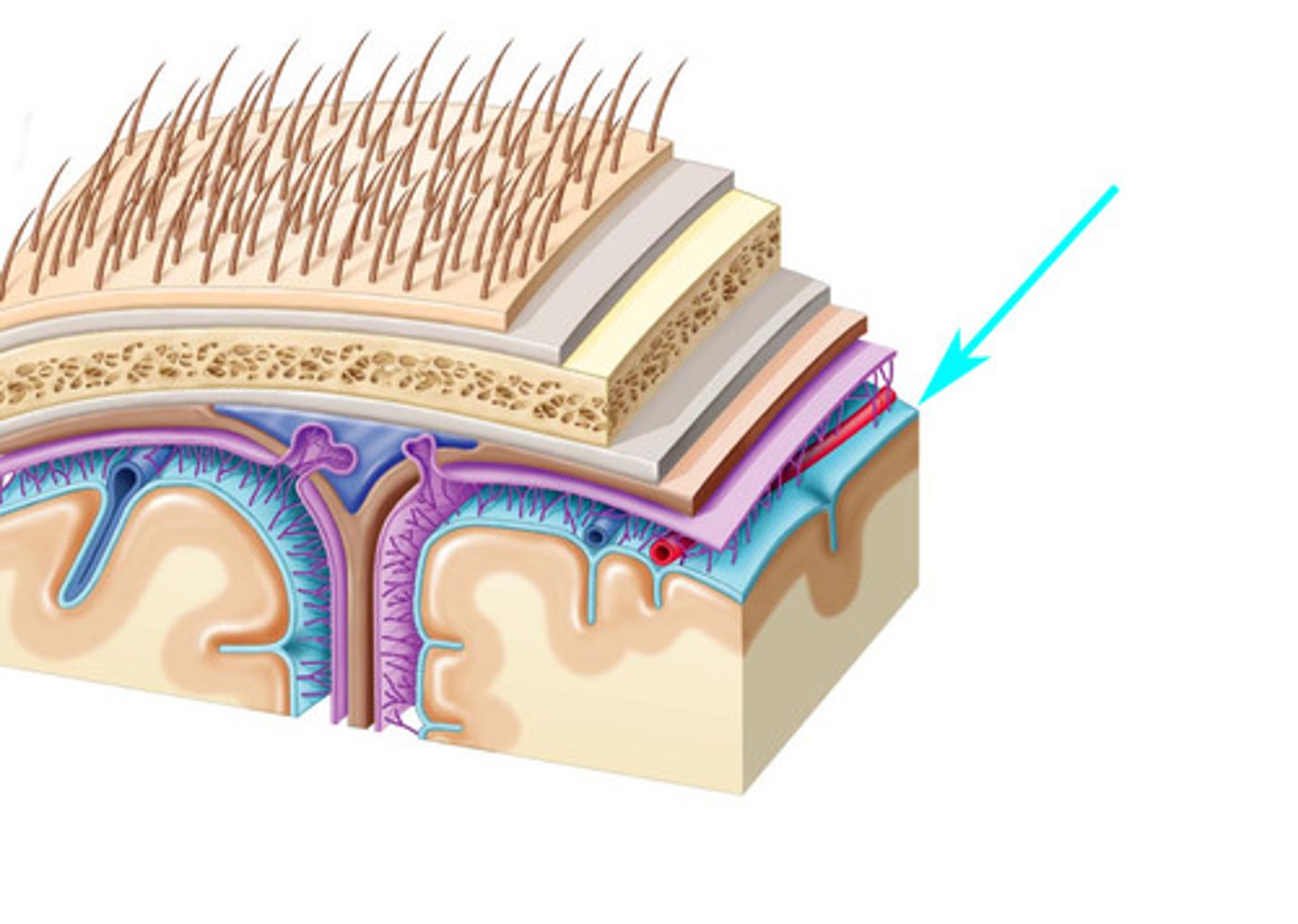
Menenges
dura mater, arachnoid mater, pia mater. Cover brain and spinal cord
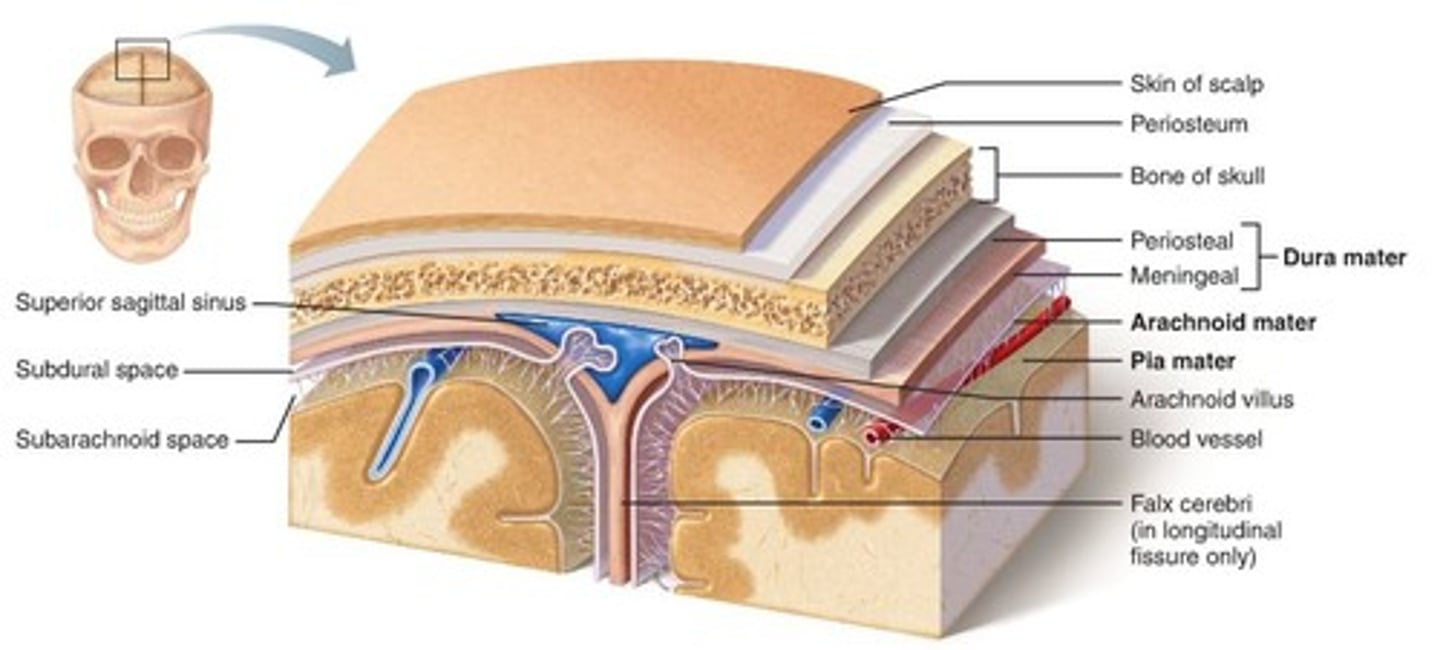
epidural space
space between the dura mater and the wall of the vertebral canal
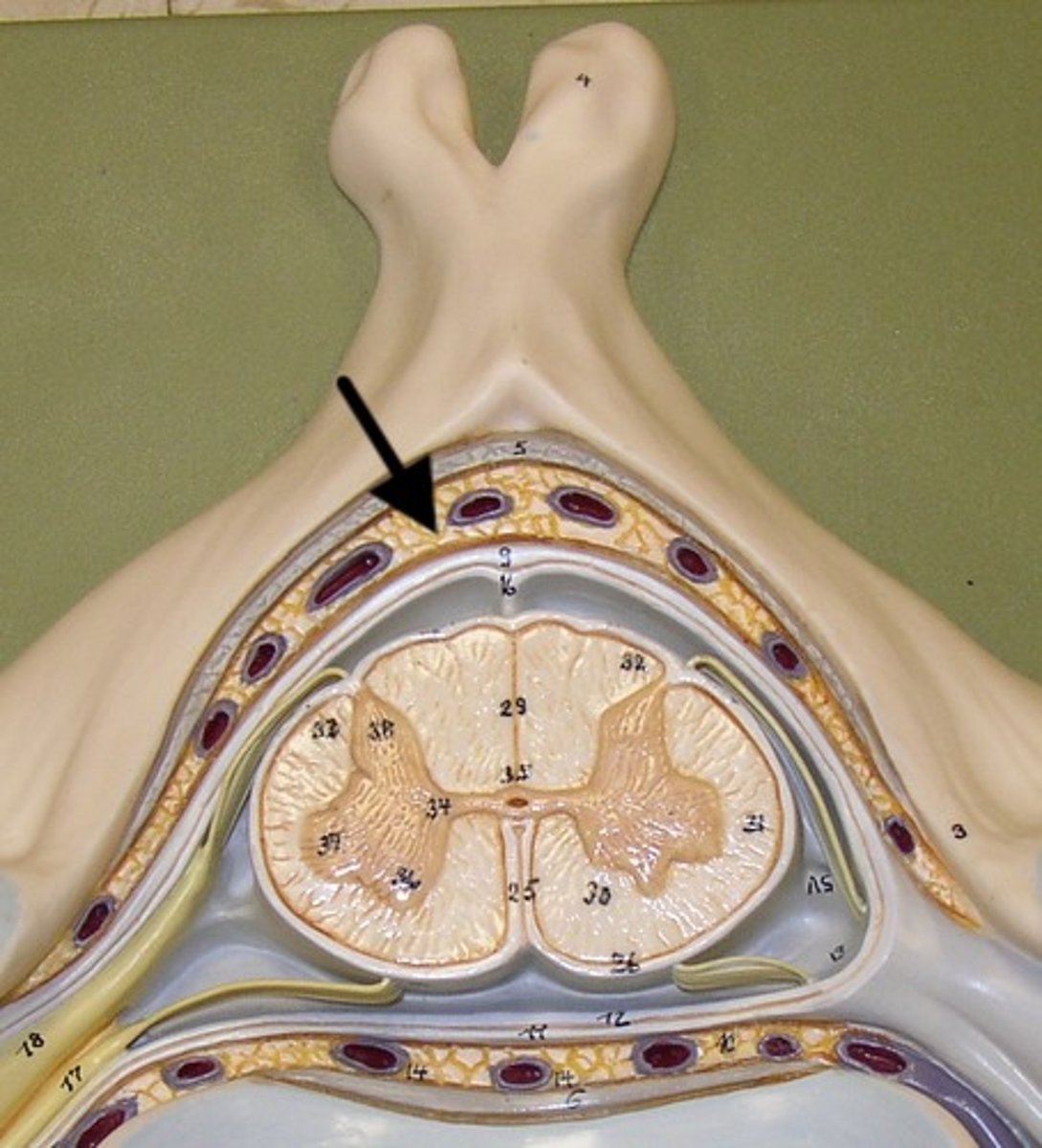
Duramater
Outermost layer of the meninges. Subdural space
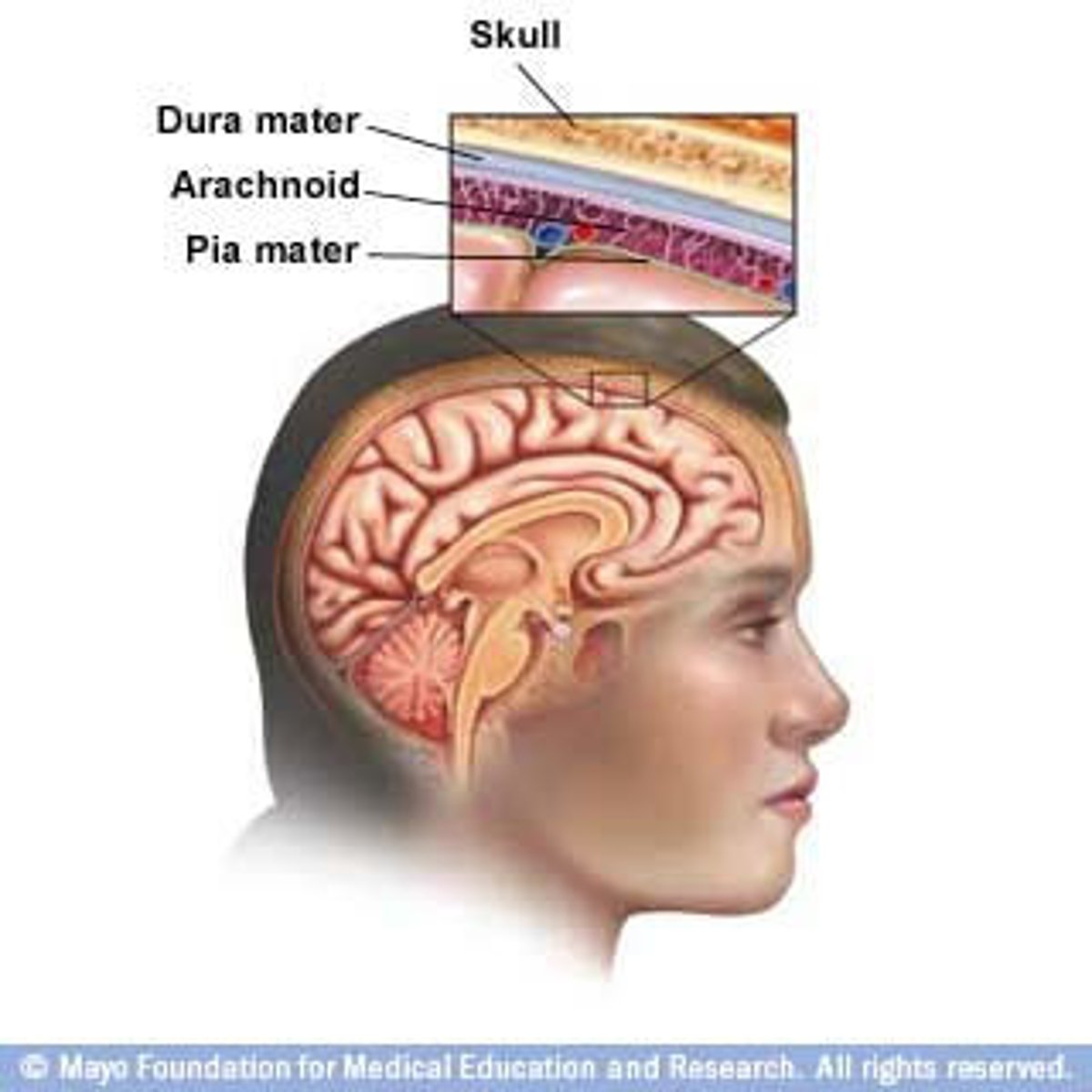
arachnoid mater
middle layer of the meninges. Subarachnoid space CSF
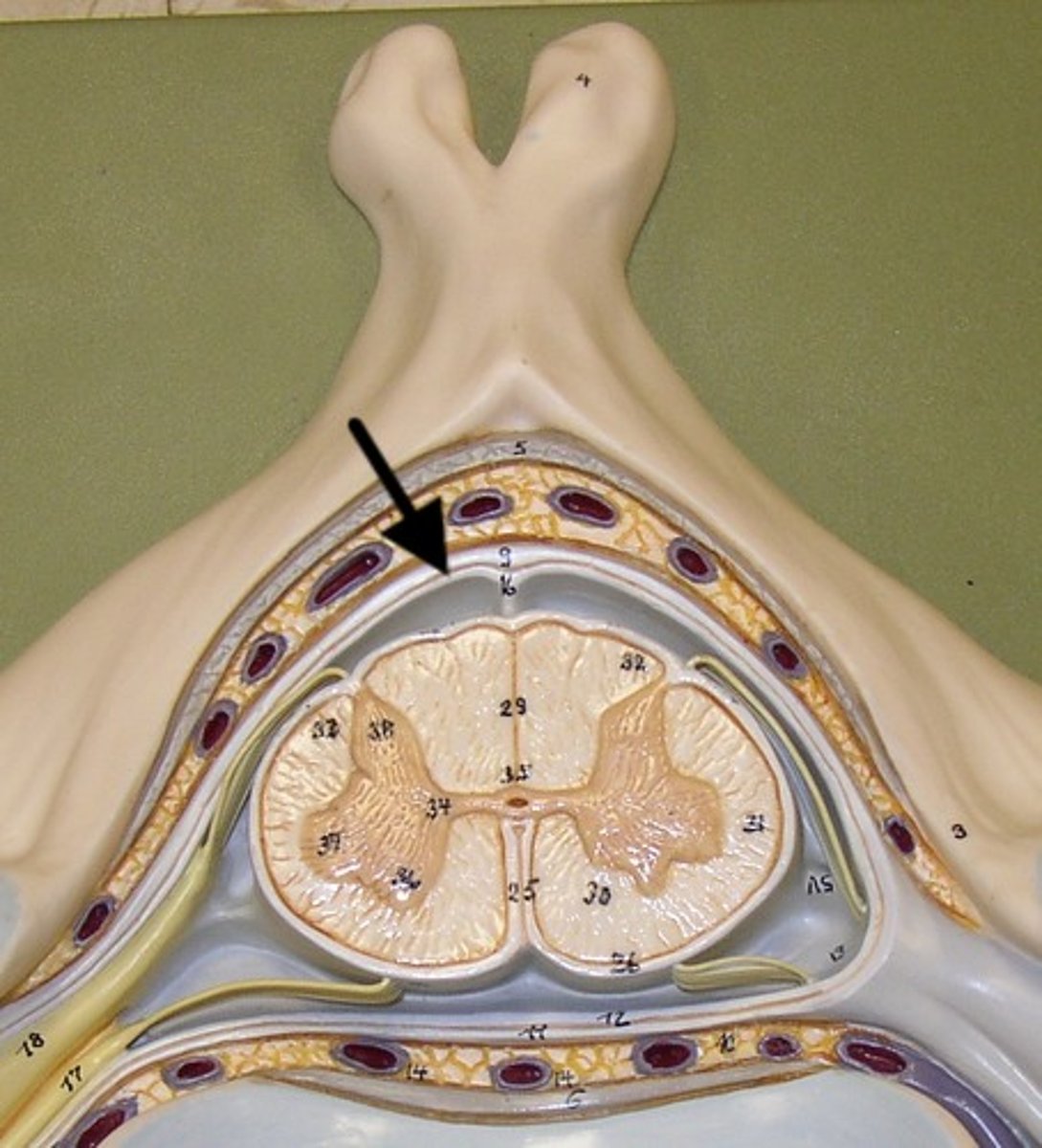
Piamater
the inner layer of the meninges that is attached firmly to the brain
Diffuse concussion mechanism
• mTBI or TBI
• Second Impact Syndrome
• Post-Concussion Syndrome
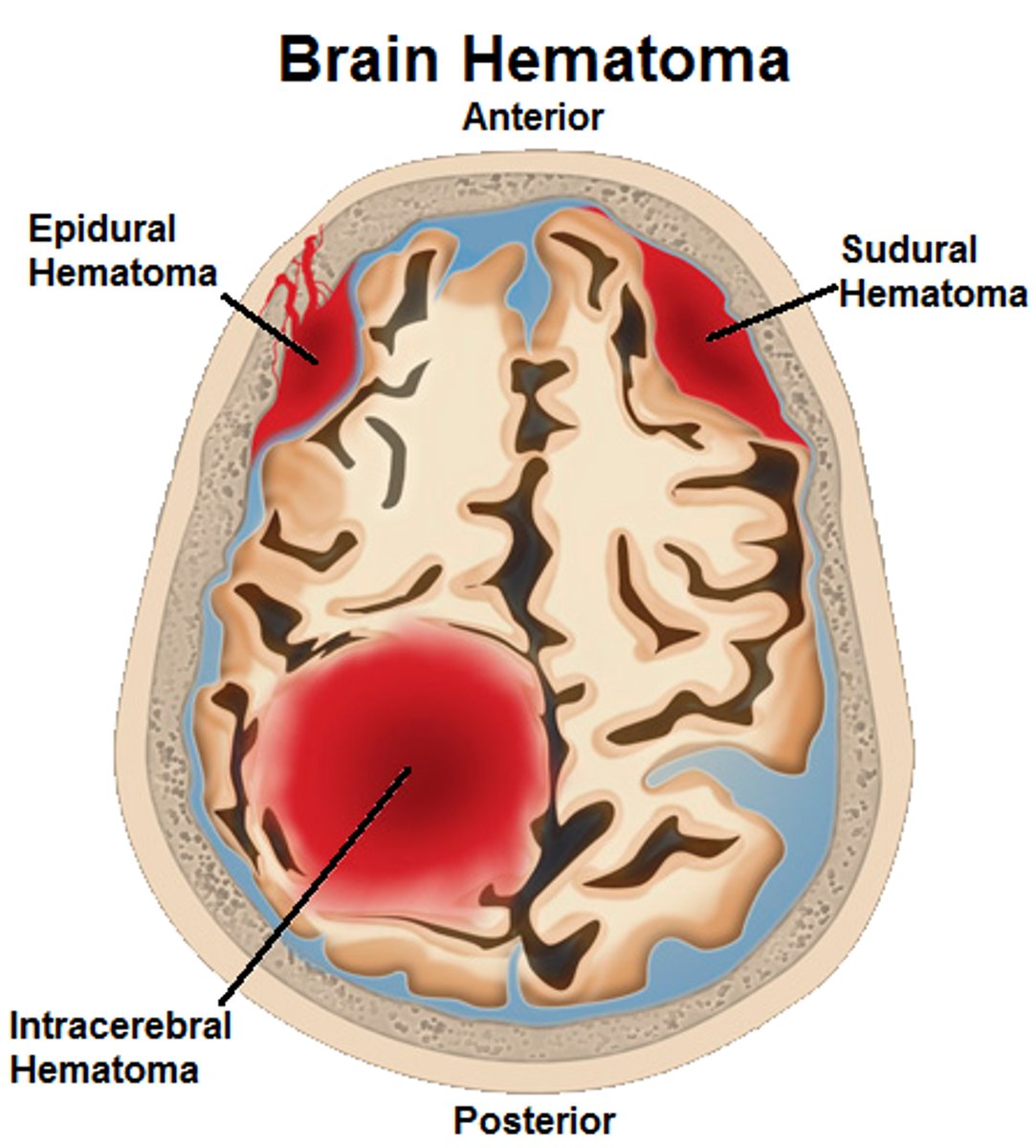
Focal Serious Head Trauma Mechanism
• Skull Fracture
• Contusion
• Intracranial/cerebral Hemorrhage
• Epidural Hematoma
• Subdural Hematoma
coup injury
Injury directly below the point of impact
countercoup injury
Injury on opposite side of impact
Concussion can result from a
• Jarring
• Rotational Acceleration
• Coup (Same) and Contrecoup (Opposite)
blow
Concussion prevention
• NATA Position Statement on Head-Down Contact & Spearing in Tackle Football
• http://www.nata.org/Heads-Up
• Helmets & Mouthguards: The Role of Personal Equipment in Preventing Sport-Related Concussions
• Read & Review- Blackboard Handouts
• On-the-Field Management- Helmet Sensors
• Reduces under-reporting of head injuries & risk for second impact syndrome
• NOCSAE- New Standards
• Player & Coach Education- NATA & NCAA-DOD initiatives
• Limited contact play, fair play, rule enforcement
Signs of concussion
Loss of consciousness, disorientation, Incoherent speech, confusion, memory loss, dazed or vacant stare.
symptoms of concussion
Headache/dizzy, confusion, light sensitivity, ringing in ears, fatigue and vomiting

skull fracture
a fracture of the bony structure of the head
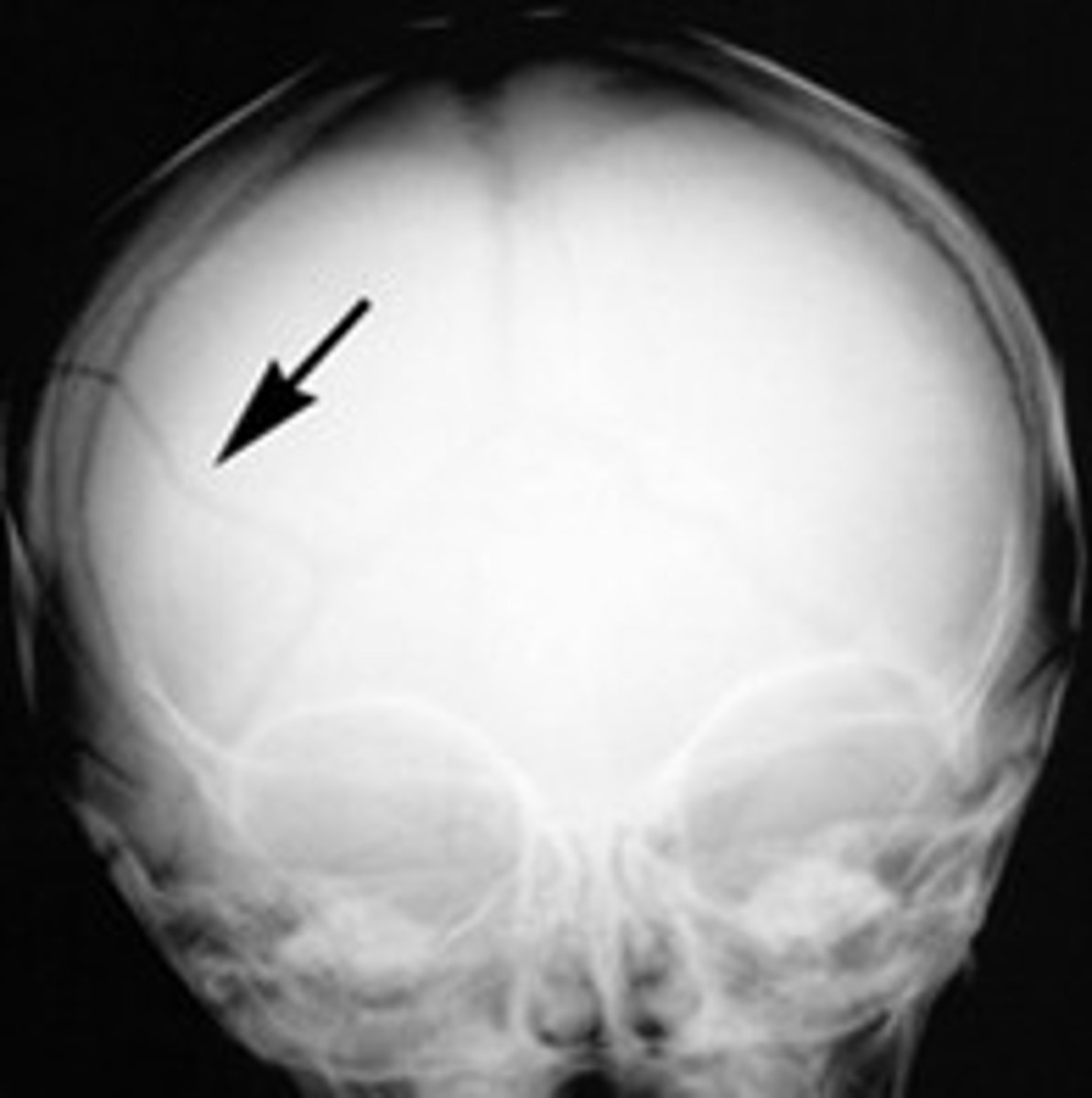
Skull fracture immediate signs and symptoms
• Headache
• Increased blood pressure
• Decreased pulse
• Decreased respiration
• Dizziness
• Pale, clammy skin
Skull fracture late signs and symptoms
battle sign and raccoon eyes
"Battle sign" is an indication of a:
skull injury- A bruise behind the ear of a trauma patient is called Battle sign, and is an important sign of a skull injury.

raccoon eyes
Bruising around the eyes, indicative of a basilar skull fracture

epidural hematoma (EDH)
a mass of blood that forms between the skull and the dura mater as a result of the brain colliding against the skull, such as from a head injury or a fall
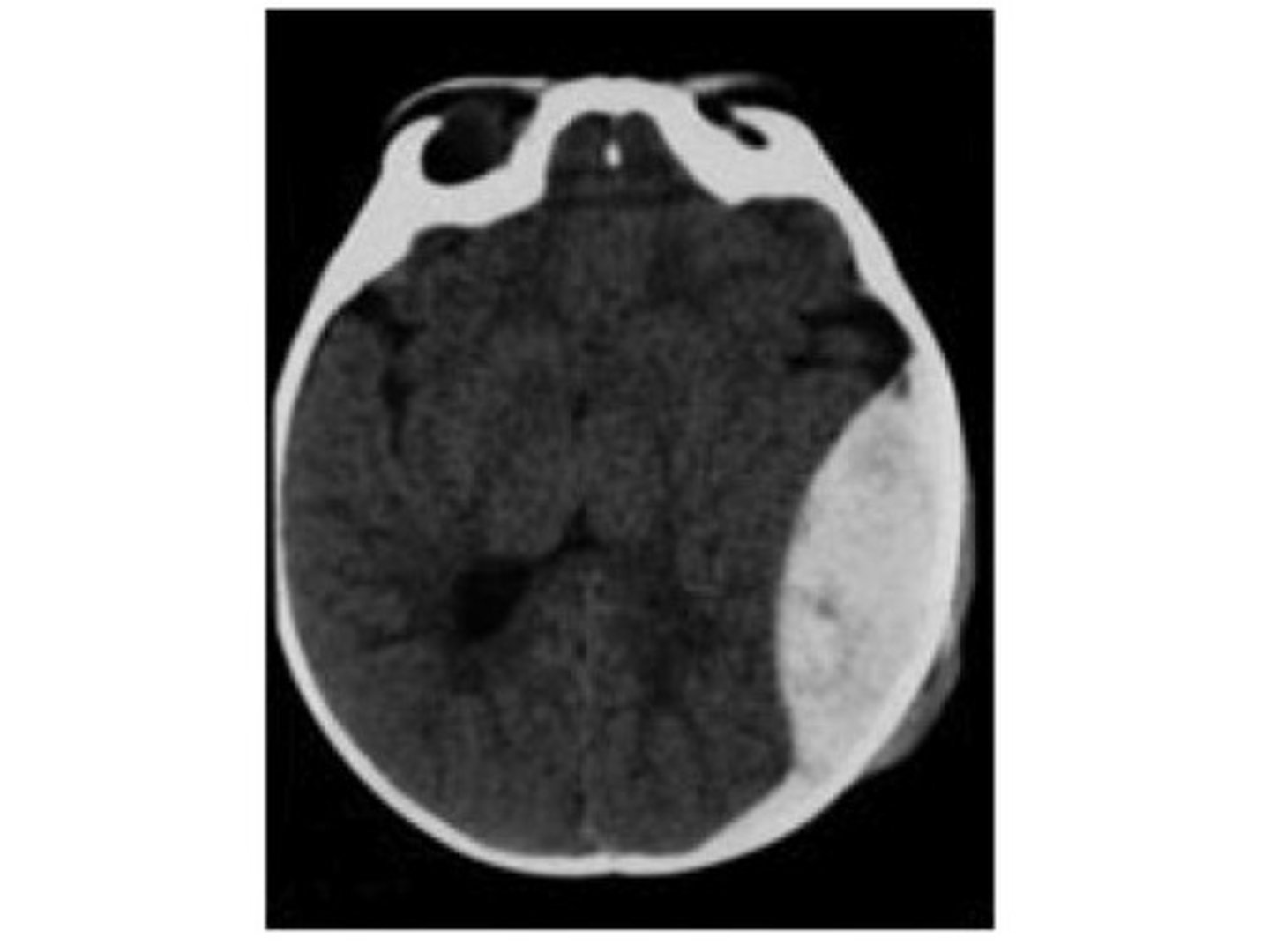
subdural hematoma
collection of blood under the dura mater
Cognitive Concussion Symptoms
mentally foggy, difficulty concentrating/remembering, repeats question, feeling mentally slow, forgetful of recent info, confused about recent events, answers questions slowly
Physical Concussion Symptoms
- headache, blurry vision, dizziness
-Visual issues
-Numbness/tingling
-Dazzed or stunned
- nausea, vomiting
- balance problems
- sensitivity to noise and light
- feeling tired, no energy
Emotional concussion symptoms
- irritability
- sadness
- more emotional
- nervousness or anxiety
Sleep Concussion Symptoms
-Sleeping more than usual
-Sleeping less than usual
-Trouble falling asleep
-Drowsiness
PEARL test
pupils are equal and reactive to light
H test
clinical test for normal eye movement. Eye tracking
nystagmus
repetitive rhythmic movements of one or both eyes
Romberg test
-ask client to stand with feet at comfortable distance apart, arms at sides, and eyes closed
-expected finding: client should be able to stand with minimal swaying for at least 5 seconds
-Balance test
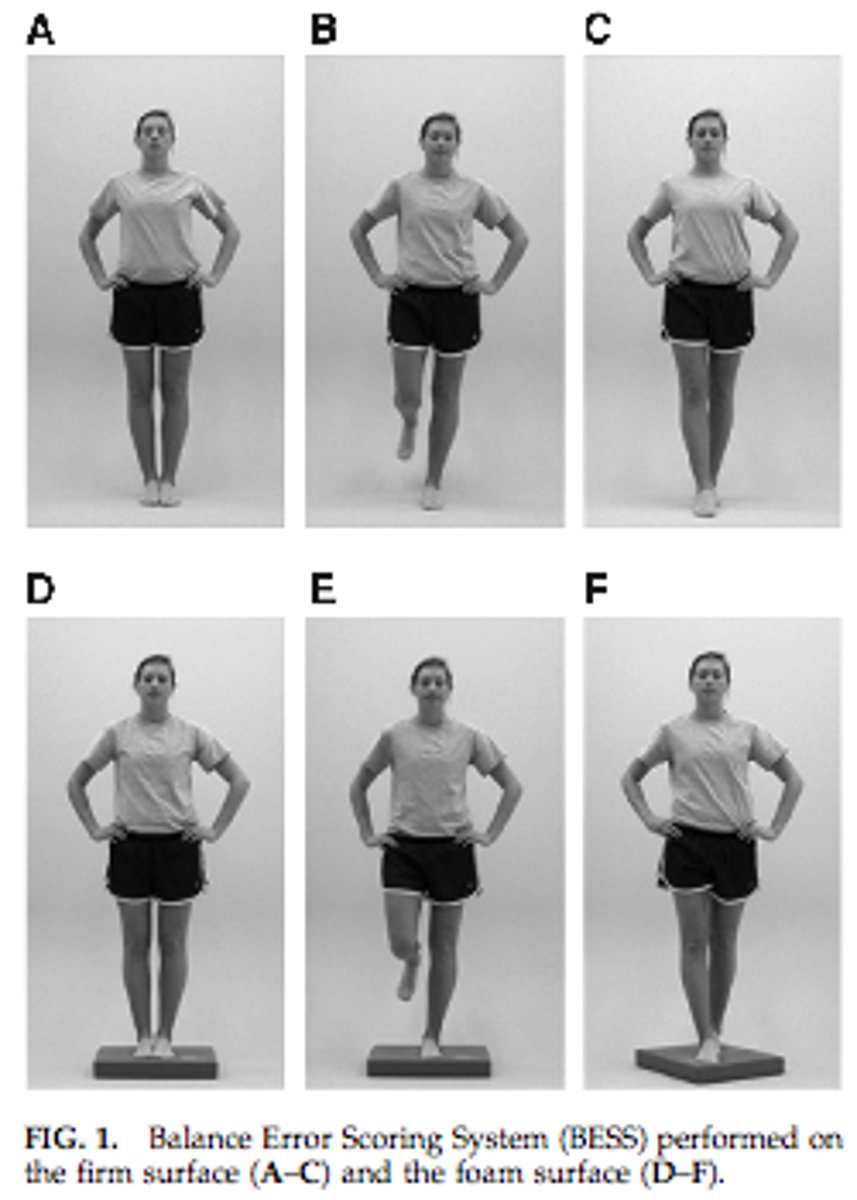
BESS (balance error scoring system)
is a balance assessment protocol that was developed specifically for assessing sports concussions
Coordination testing
Finger-to-nose testing - clients touch the clinician's finger and then their own nose as the clinician's finger varies in location

SAC test
Standardized assessment of Concussion. Cognitive test on sideline
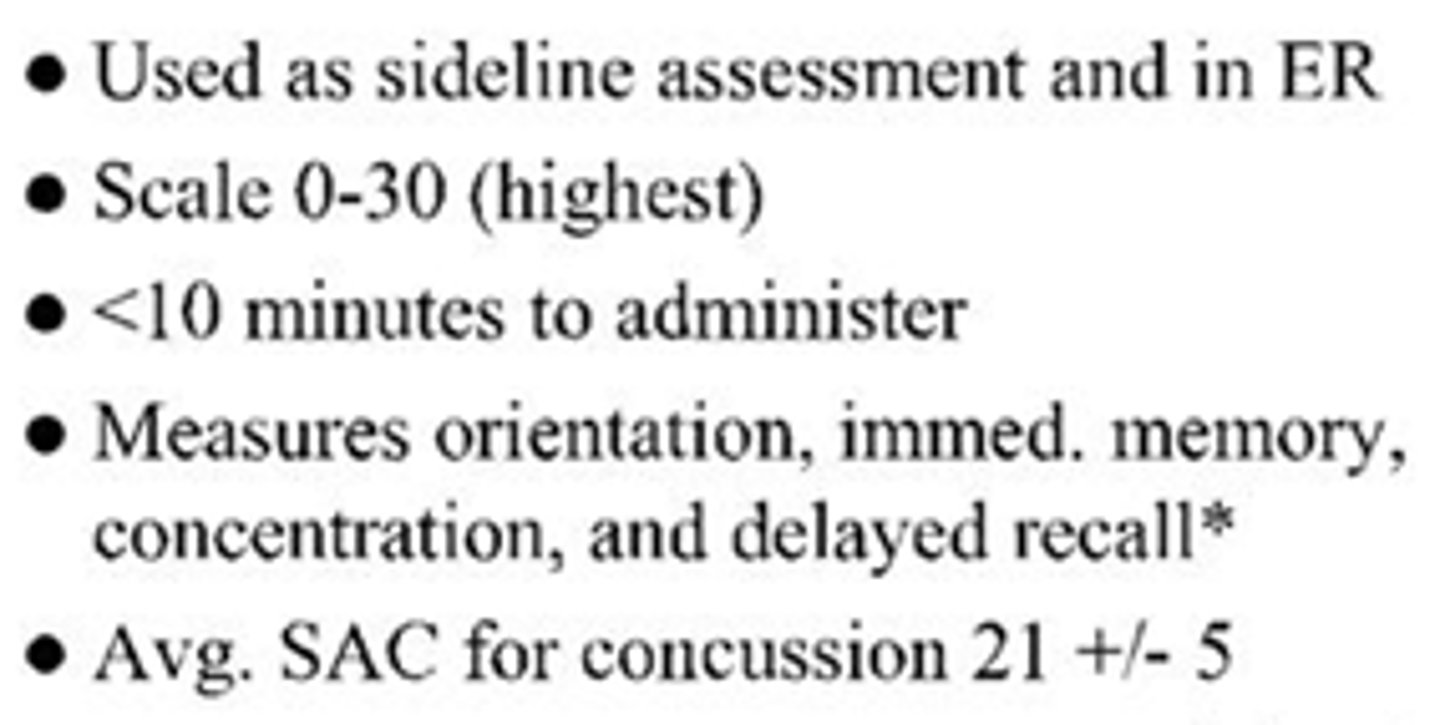
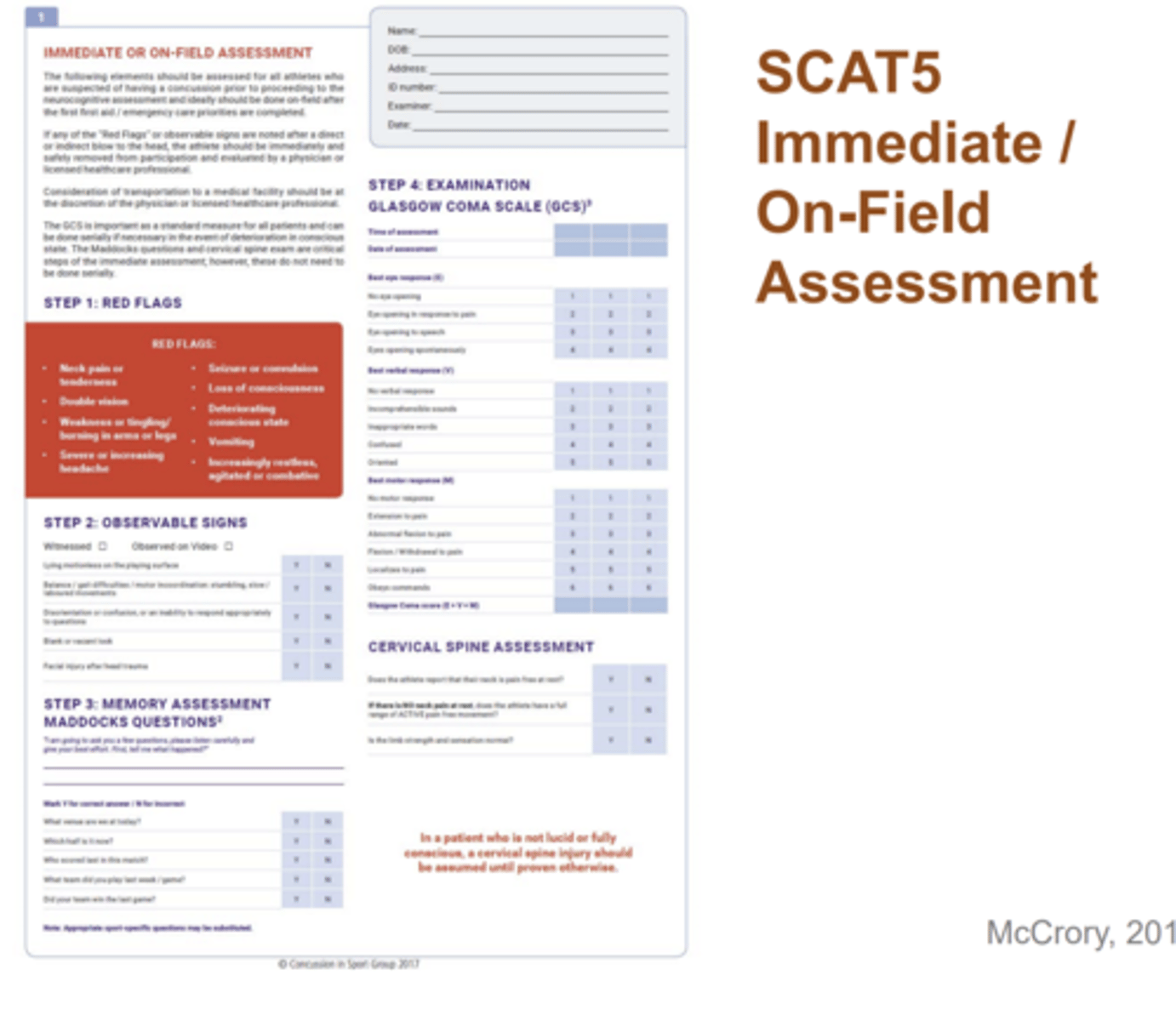
SCAT5
More comprehensive and inclusive
concussion treatment
• Patient/Parent/Coach/School Education
• Cognitive & Physical Rest
• Return-to-Play Guidelines
• Return-to-Learn Guidelines
• Neurocognitive Rehabilitation
• Attention Processes- best evidence
• Medication
• Anti-depressants- more to treat symptoms
• Vestibular/Ocular Motor Screening (VOMS)
• Vestibular Therapy
• Balance
• Motor control
• Reading & change gaze focus
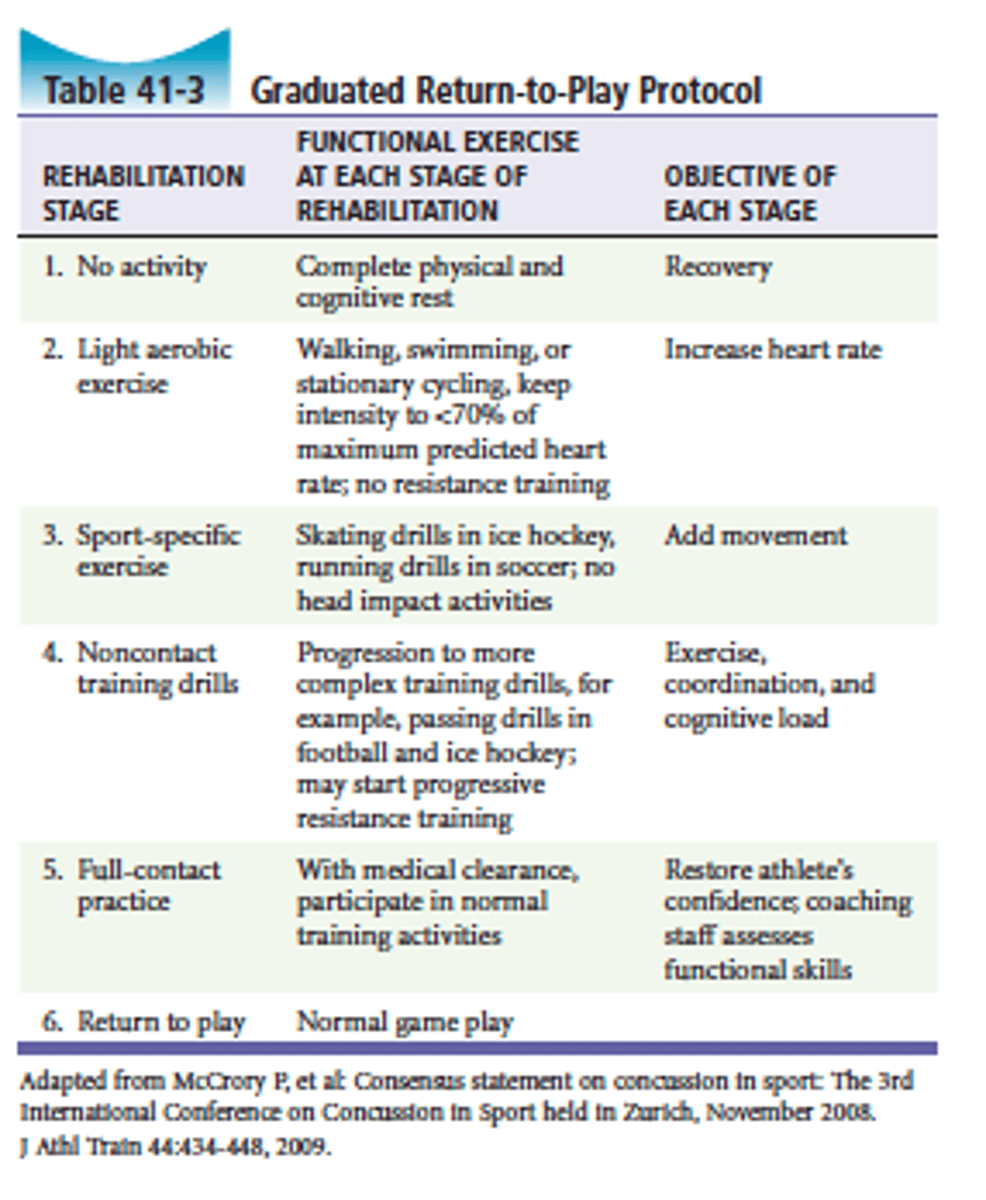
Return to play protocol
View image
Return to learn protocol
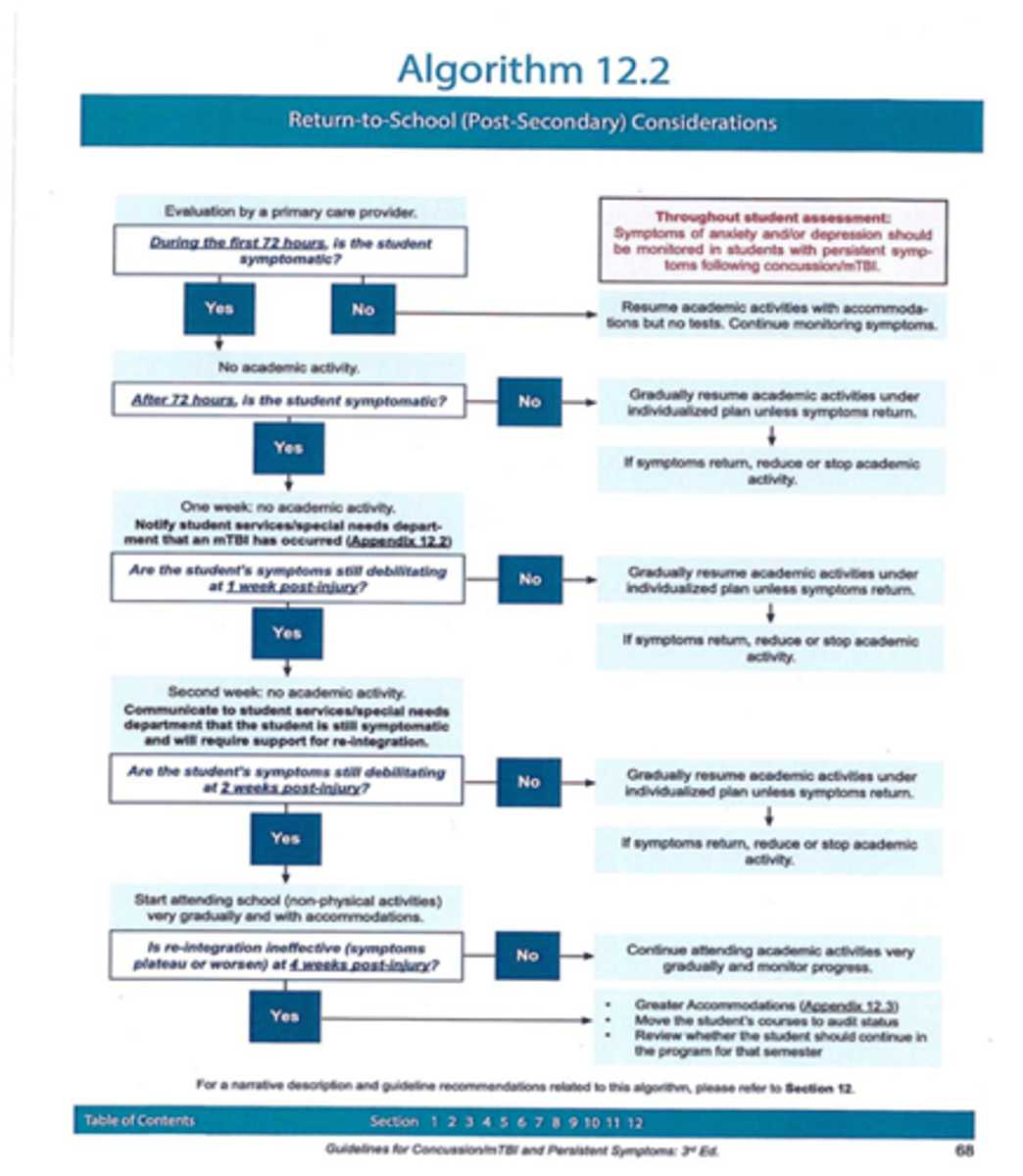
Consensus Statement of the Fourth International Conference on Concussion in Sport, Berlin, 2016British Journal of Sports Medicine (2017);51:838-847.
• Recognize (Definition & Sideline assessment)
• Removal from Play & Revaluate
• Rest
• Rehabilitation
• Refer
• Recovery (Adult vs. Adolescent vs. Child)
• Return to Sport
• Reconsider
• Residual Effects
• Risk Reduction
How we lose heat
• Radiation: 50%
• Convection & Conduction: 15%
• Evaporation: 30%
• Respiration: 5%
Heat Stress
• Motivation from peers/coaches to push to the point of collapse
• Accumulated fatigue
• Sleep loss
• Prolonged exercise bout on preceding day
• Prolonged heat exposure on preceding day
Heat injury in the athlete
• Heat Cramps
• Heat Exhaustion
• Exertional Heat Stroke
HEAT CRAMPS
• Muscle function requires balance of electrolytes & water
• Both are lost during exercise
• Present with painful contractions of skeletal muscles
• Calf mostly effected, but can be any
Heat cramps treatment
• Rx: best is PREVENTION
• Proper fluid ingestion
• Days and hours preceding exercise
• During exercise
• Through diet
• Electrolyte drinks, salting foods
• Rx: rest, stretch, ice, re-hydrate
Exertional Heat Exhaustion Symptoms
Headache, fatigue, weakness, skin moist/sweating, low BP, High HR, ANXIETY/Confusion. Body temp lower then 38.8 degrees celcius or 102 degrees f
Heat exhaustion causes
low fluid intake, high heat exposure and activity
Heat Exhaustion Treatment
• Best treatment = prevention
• Lying down in cool environment
• Elevate the extremities
• Hypotonic fluid replacement
• (0.25% saline triggers osmosis)
• I.V.?
• Monitor vitals
• Treat for shock
heat stroke symptoms
Anxiety/confusion, skin hot and dry, impaired sweating, NA/K depletion, body temp above 105 degrees F, Listlessness, Pulse and resp rate high, hypertension
Cerebral edema: Seizures, delirium and coma
Exertional heat stroke
• True medical emergency!!!
• If rapid cooling (20-30 min) is not effective mortality rate is 20-75%
• May develop as a progression of heat exhaustion but most often occurs suddenly without warning.
• A failure in the thermoregulatory system!
• Essential to recognize CNS changes
• Athlete may have a brief (10-15 minute) "Lucid Interval".
• May be conscious, coherent, and conversant but likely feels out-of sorts
• Athletic Trainer and/or coach may recognize something is wrong
Heat stroke treatment
• Best treatment = prevention
• Activate EMS
• Cool QUICKLY!! (Primary Goal)
• Remove excessive clothing, respecting privacy as much as poss. (including socks and shoes)
• Cool: Shade, ice baths, towels, packs
• Monitor vitals until EMS arrives
• *Cool first, Transport second*
Preventing Heat Illness
• Hydration
• Lemonade vs. clear colored urine
• Dehydration
• Unrestricted fluids
• Gradual acclimatization
• 7-10 days
• Identify susceptible individuals
• Appropriate clothing
• Monitor Weight-loss records
• 1 lb. wt. loss = 16 oz. fluid replacement
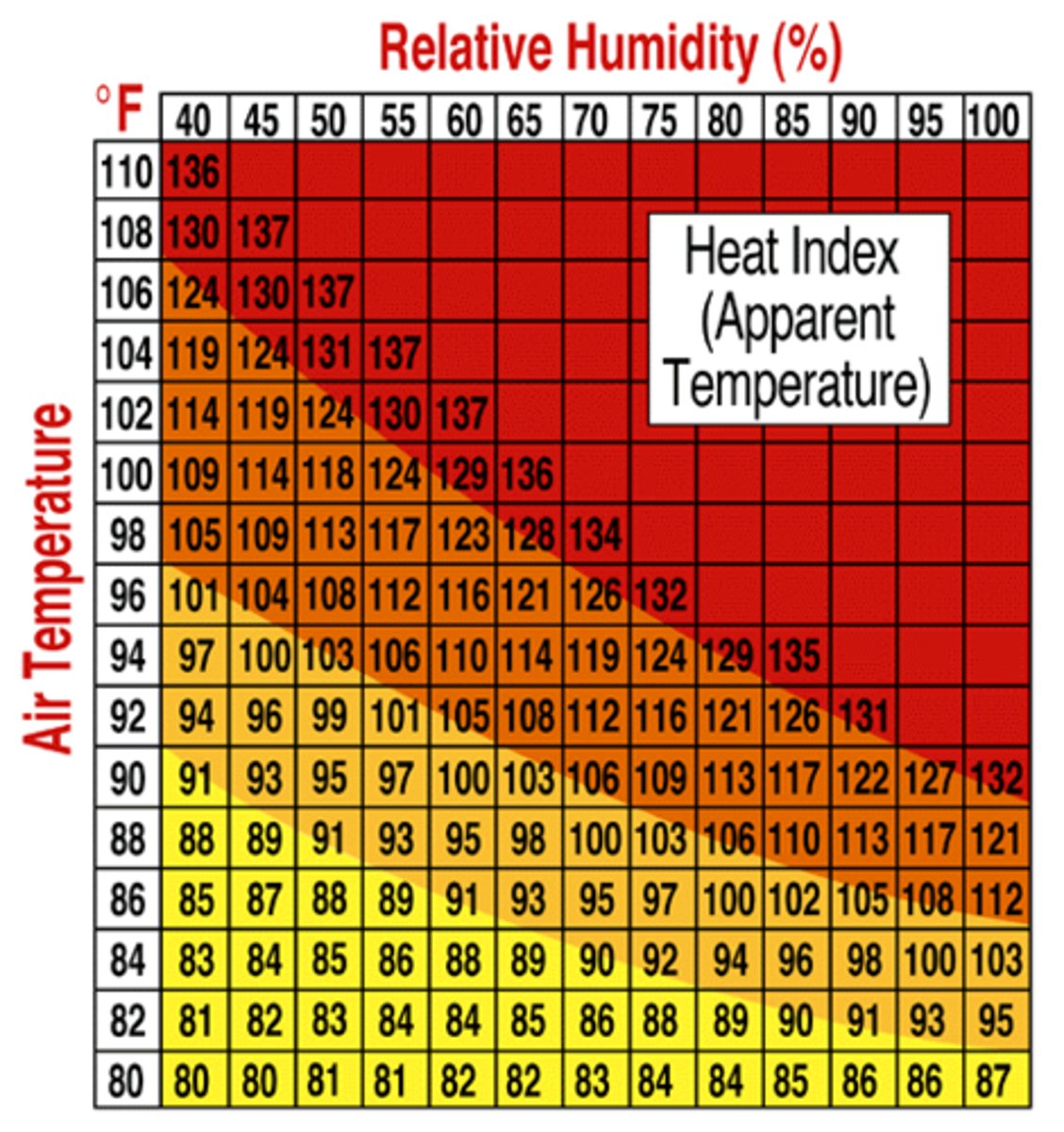
• Monitoring the heat index
Assessing Heat and Humidity à Via Sling Psychrometer
Heat Index Chart
• Heat Index Calculator using degrees F and relative humidity. (Link below)
• http://www.weatherimages.org/data/heatindex.html
• Green Zone: Full practice, Work/Ex intervals of 25-30 min. followed by 5-10 min rest period
• Yellow Zone: Limited equipment (FB shells only), Work/Ex interval of 20-25 min, 5-10 min rest period
• Red Zone: Shorts and light colored clothing only, no protective equipment, Work/Ex intervals of 15-20 min., 5-10 min rest period
Lightening
• Most consistent and significant weather hazard that may affect athletics.
• ~100 deaths/year (late spring to early fall)
Weather monitoring
• Local reports
• National Weather Services (NWS)
• Internet and Radio
• Lightning Detectors
Sheltering
Safe shelters
• A substantial building (one that is frequently inhabited...house, public building)
• Fully enclosed vehicle with a metal roof and windows closed.
à Areas to avoid
• light poles/ flag poles
• Wooden, vinyl or metal sheds
• Golf carts
• Metal bleachers
• Large trees
• Under canopy's
• Standing water i.e. pond, pool, puddle, wet field
When to seek safe sheltering"you are in danger of lightning if you can hear thunder"
flash to bang count
• Be aware of the first flash
• If the count from flash-to-bang is 30 seconds or less all individuals should already be inside or actively seeking shelter
• Begin counting at flash, stop at bang (thunder)
• If you divide by 5 = distance. So, if the flash-to-bang is 30 seconds, distance = 6 miles
"30-30" Rule
• If the flash-to-bang is < 30 seconds seek shelter & suspend activities
• Once suspended, wait at least 30 minutes after the last sound of thunder or lighting flash to resume activity.
• Be aware:
• It is possible to have lightning w/o thunder, but thunder never occurs without lightning.
• Blue sky and/or lack of rainfall are not a factor in your decisions.
• "Bolt out of the blue"- lightning can strike with a blue sky
LIGHTNING SAFETYWHAT IF...
• Avoid being in contact with or near the highest point in an open field
• Avoid showers and land-line phones
• If you feel hair stand on end or skin tingle or hear crackling noises: assume the "lightning safe position"
• Get out of water. It is a GREAT conductor of electricity
Lightening safe position
• Crouched, on ground
• Weight on balls of feet
• Feet together
• Head lowered
• Eyes closed
• Ears covered
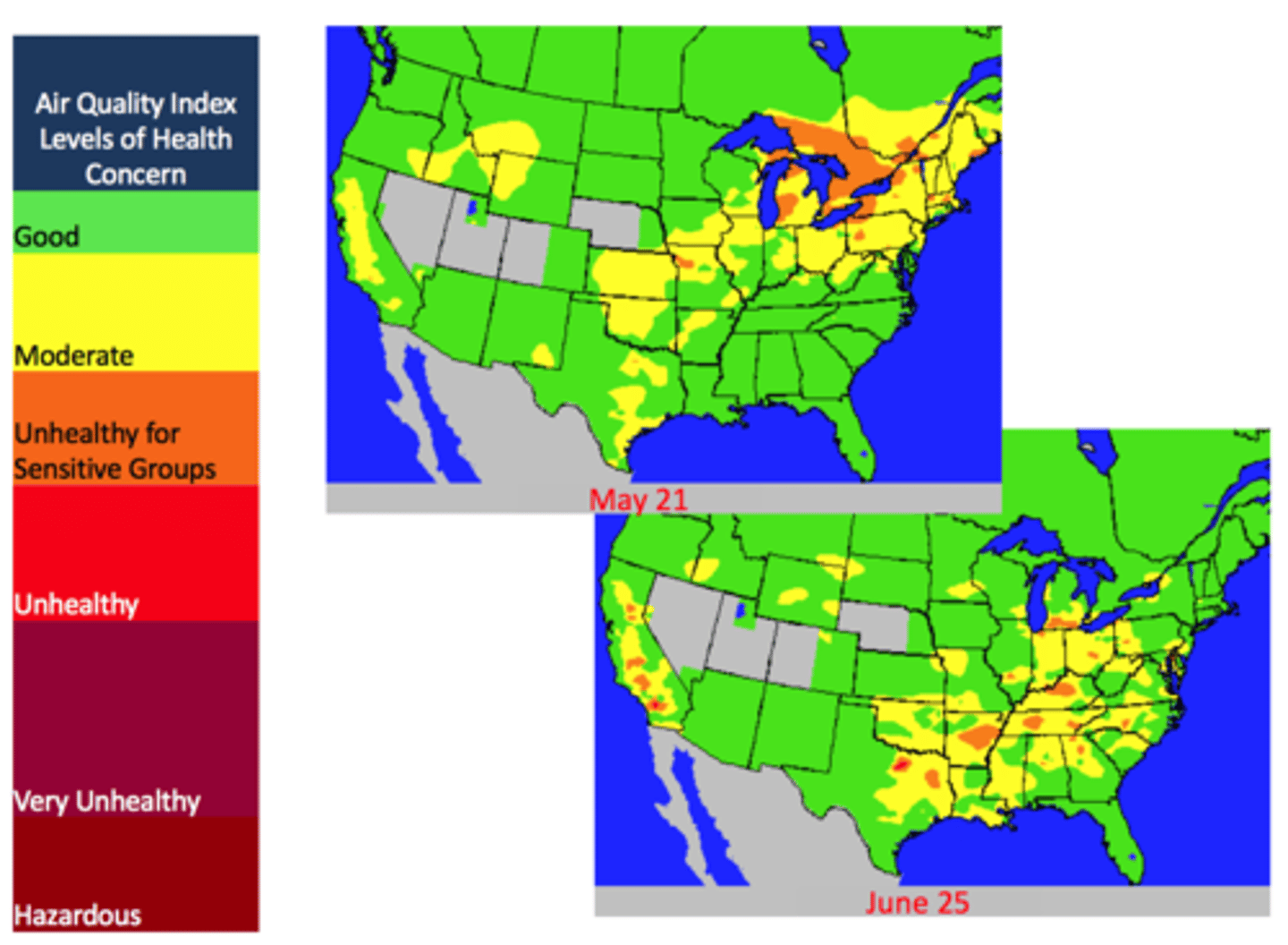
air pollution/quality
• Ozone
• Form of oxygen (O3)
• Sulfur Dioxide
• Colorless gas, by product of coal/ petroleum burning
• Particulate Matter (PM)
• Smoke, smog, ash, dirt, pollen (PM2.5/PM10)
• Carbon Monoxide
• Colorless, odorless gas
• Reduces hemoglobin's ability to transport oxygen
* Not only interferes with sports performance, also with behavioral & mental faculties.
Effects of poor air quality
Signs and Symptoms:
▪Cough
▪Trouble breathing deeply
▪Scratchy throat
▪Irritated sinuses
▪Headache
▪Runny nose and itchy eyes
People with conditions such as asthma or chronic bronchitis may find their symptoms worsening.
Air Quality- PM2.5 Reading
• PM2.5> 65- unhealthy for
• Sensitive groups
• AQI > 100- unhealthy for
• Sensitive groups
• www.sdapcd.org
Activity management
• Special Considerations for asthmatic athletes, or other respiratory disorders
• Modify outdoor activity based upon PM2.5 & AQI readings
• Avoid prolonged outdoor exposure > 1 hour
• Consider indoor alternatives
• Teams can travel to other areas to practice
• Be prepared to utilize indoor space- have a plan!!
• FOLLOW University mandates
Respiratory Emergency
• Always have rescue medications available:
• Inhalers, antihistamines, etc.(Insist on preventative use during poor AQI days)
• D/C activity and remove from location
• If treatment does not relieve the problem, the patient needs to be transported, without delay, to the nearest advanced healthcare facility.
• Calm athlete through distress
liability
Liability
◦ "(A) quality or state of being legally obligated or accountable; legal responsibility to another or to society" (Garner, 2004)
◦ A legal responsibility to provide a certain standard or quality of care
Example: Under state law, a patient may pursue a civil claim against physicians or other health care providers, called medical liability or medical malpractice, if the health care provider causes injury or death to the patient through a negligent act or omission. ... A compensable injury
◦
Negligence
◦ Failure to provide the standard of care that a reasonably prudent person would have provided.
◦ Examples: For example: Property owners who let steps to their house crumble and leave a railing unrepaired could be considered negligent if they invites friends over to their house and their friends trip on the railing and steps and hurt
4 elements of negligence
◦ Duty of Care
◦ Breach of Duty (Torts)
◦ Causation
◦ Harm
Duty of care
◦ A specific obligation to not harm others or their property
◦ Reasonable person = "ordinary adult without disabilities"
◦ May be dependent on location (rural vs. urban)
Breach of duty/torts
◦ Nonfeasance = act of omission
An act that should have been performed that was not
◦ Malfeasance = act of commission
An act that should not have been performed that was performed
◦ Misfeasance = an act improperly conducted
Causation
◦ Duty and breach must be fulfilled
◦ Proximate cause
Remove implicated actions from the fact pattern or sequence of events, and then see if the injury or damage would still be present
"but for" test = the injury would not have happened "but for" the actions of the defendant
◦ Harm
Actual damage must exist
Only liable for harm that is a foreseeable consequence of their actions.
standard of reasonable care
◦ Standard of Care
Can be influenced by many factors
The most prevalent and concrete factor is a
Position Statement
A publicized statement regarding a specific situation or issue from a learned society or group
risk assessment
evaluate risks and identify vulnerabilities to be addressed
Risk Mitigation
prevention of losses via education training
Risk analysis
evaluate data available looking for trends
Risk response
organizational response to events
practicing risk management
◦ The best way to deal with a risk is to avoid it!!
◦ A more practical approach is preparation to limit risk
◦ Two primary methods to limit risk:
◦ Emergency action plan (Monday 12/10)
◦ Policies and procedures
◦ Minimal criteria
◦ All venues
policies and procedures
Directed toward noninjury situations
Directs everyday actions
Examples
◦ Reduces risk by ensuring safe practices
◦ If not followed, it increases risk of litigation
◦ Resource for assistance in developing policies and procedures
◦ Collegiate Sports Medicine Foundation (www.csmfoundation.org)
How do we reduce risk?
Caution when distributing OTC medications
◦ Work within scope of practice
◦ Annual checks and maintenance of equipment
◦ Use appropriate protective equipment
◦ Follow direction of physician
◦ Purchase professional liability issuance
◦ Know state regulations
◦ Stay off social media with regards to clients/patients
◦ Use common sense
Practicing Risk Management
◦ http://www.hpso.com/individuals/professional-liability-insurance
◦ Professional Liability Insurance