Pediatrics Pt. 2
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
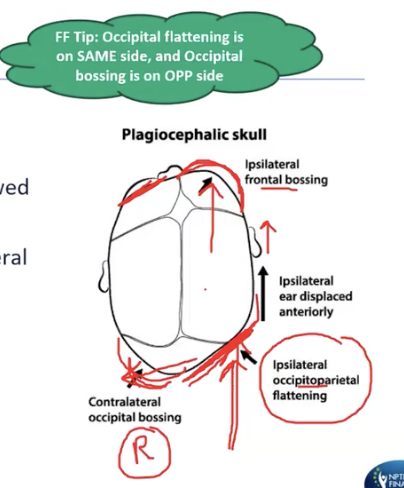
Plagiocephaly:
what does it result from?
creates what shaped when viewed from the vertex?
what is named after??
side of flattening and bossing?
side of frontal bossing and ear displacement?
assess what 2 aspects, educate parents on what 4 things?
results from prolonged asymmetrical pressure on the premature skull
creates a parallelogram shape when viewed from the vertex (top-down)
named after the side of the flattening
occipitoparietal flattening and contralateral occipital bossing
bossing is if you push on the back of the head, it will push out on the front side of the head, same side on the front
ipsilateral frontal bossing and anterior displacement of the ear
assess C/S ROM and strength, educate parents on positioning, exercises, helmet, and tummy time
If a patient has R plagiocephaly/occipital flattening, what side would torticollis be on?
L torticollis
L SCM sidebends L, rotates R
rotation leads to plagiocephaly

analyze this pic:
head position
torticollis
plagiocephaly
other possible related condition
treatment/stretching
head position
L sidebend, R rotation
torticollis
L torticollis, L SCM
plagiocephaly
R plagio
other possible related condition
baby may be too big/long for mother’s uterus / torso
foot deformities
hip dysplasia
baby is jammed up, trying to curl themself up
joint contractures
arthrogryposis
joint/limb contractures at birth
treatment/stretching
opposite sidebend/rotation
R SB, L rot, extension because SCM does flexion when actions are together
Practice Question 3
A 4-month-old infant with right congenital torticollis is being treated in a pediatric physical therapy clinic. Which of the following is MOST APPROPRIATE intervention?
A. Educate parents on keeping objects of interest on the baby’s right side in supine
B. Hold the baby in a “football hold” facing forward and in left side lying in the arms
C. Promote cervical flexion by drawing the baby’s attention caudally while in supported sitting
D. Perform gentle massage to the left sternocleidomastoid muscle
A. Educate parents on keeping objects of interest on the baby’s right side in supine
RATIONALE: With a right torticollis, the right SCM is affected and the head is positioned in right side flexion and left rotation. Treatment should promote right rotation, left side flexion, and cervical extension via tummy time. Keeping objects of interest on the right side in supine will promote right rotation. A football hold in left side lying promotes right side bending via the head righting reaction/reflex. Bilateral function of the SCMs is cervical flexion, cervical extension should be promoted to stretch the affected SCM. Gentle massage of the affected (right SCM) can be beneficial.
Cerebral Palsy (CP) is classified on what 3 things?
according to movement disorders
1. spastic
2. ataxia
3. dyskinetic
What is spastic depending on?
what are 4 examples/functional movements you would see spasticity?
velocity dependent resistance of a muscle to stretch
synergy patterns, contractures, crouched gait, toe walking
crouched gait = LE flexion of hip and knee, add hip/scissoring, PF
Ataxia is disorder of what 3 things and associated with what?
What are 5 other impairments/functional disabilities you would see with this?
disorder of coordination, force, and timing, associated with cerebellar involvement
low tone, tremor, poor balance, wide base of support, nystagmus
Dyskinetic means it is disorder of what type of movements and associated with what?
4 impairments/functional disabilities?
disorder of involuntary movements that are slow and writhing (athetosis), associated with basal ganglia involvement
poor stability, hand tremor, fluctuating tone, hypo becomes hyper
Practice Question 4
A clinician is examining a patient diagnosed as level 2 on the Gross Motor Function Classification System. According to the diagnosis, what is the MOST LIKELY ambulation status of this patient?
A. Patient will walk without restrictions but will have limitations in more advanced gross motor skills
B. Patient will walk with an assistive device with limitations in walking outdoors and in the community
C. Patient self mobility will be severely limited, even with the use of assistive technology
D. Patient will walk without assistive device with limitations in walking outdoors and in the community
D. Patient will walk without assistive device with limitations in walking outdoors and in the community
RATIONALE: A patient that is a level 2 on the Gross Motor Function Classification System (GMFCS) will walk without assistive device with limitations in walking outdoors and in the community. Option A is level 1, option B is level 3, option C is level 5, and option D is level 2 on GMCFS.
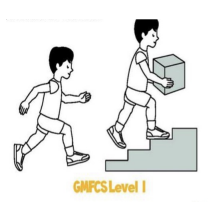
Gross motor classification of CP:
level I
patient mobility, restrictions, limitations?
level I
patient will walk without restrictions but will have limitations in more advanced gross motor skills
Gross motor classification of CP:
level II
patient mobility, restrictions, limitations?
level II
patient will walk without assistive device with limitations in walking outdoors and in the community

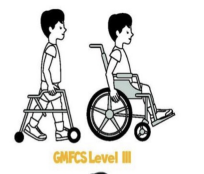
Gross motor classification of CP:
level III
patient mobility, AD, restrictions, limitations?
level III
patient will walk with assistive device with limitations in walking outdoors and in the community
Gross motor classification of CP:
level IV
patient ID/mobility, restrictions, limitations, transportation?
level IV
patient self mobility will be severely limited
children are transported or use power mobility outdoors and in the community

Gross motor classification of CP:
level V
patient ID/mobility, AD, restrictions, limitations?
level V
patient self mobility will be severely limited, even with the use of assistive technology, requires caregiver

What functional capability assessment do you use for children 6 months to 7.5 years, or children that function at a level in this range?
This also rates the level of what assistance/activity?
What are the 3 domains?
What is the normal score compared to age matched peers?
Which patients could it be used for?
pediatric evaluation of disability index (PEDI)
also rates level of caregiver assistance or activity modifications/equipment needed
three domains:
self care, mobility, social function
normal score
50 ± 10 points
population
CP, ASD, TBI
The WeeFIM is an adaptation of the Functional Independence Measure for children what ages?
Measures development and monitors what as a child ages through when?
Three domains?
What are the rates of level of assistance?
Mean score?
WeeFIM = children 6 months to 7 years, or children that function at a level in this range
measures development and monitors disability as a child ages through preschool and elementary school
three domains
self care, mobility, cognition
rates level of assistance from 1 (total assistance) to 7 (complete independence)
higher number = higher independence
mean score varies from 18-120 dependent upon age
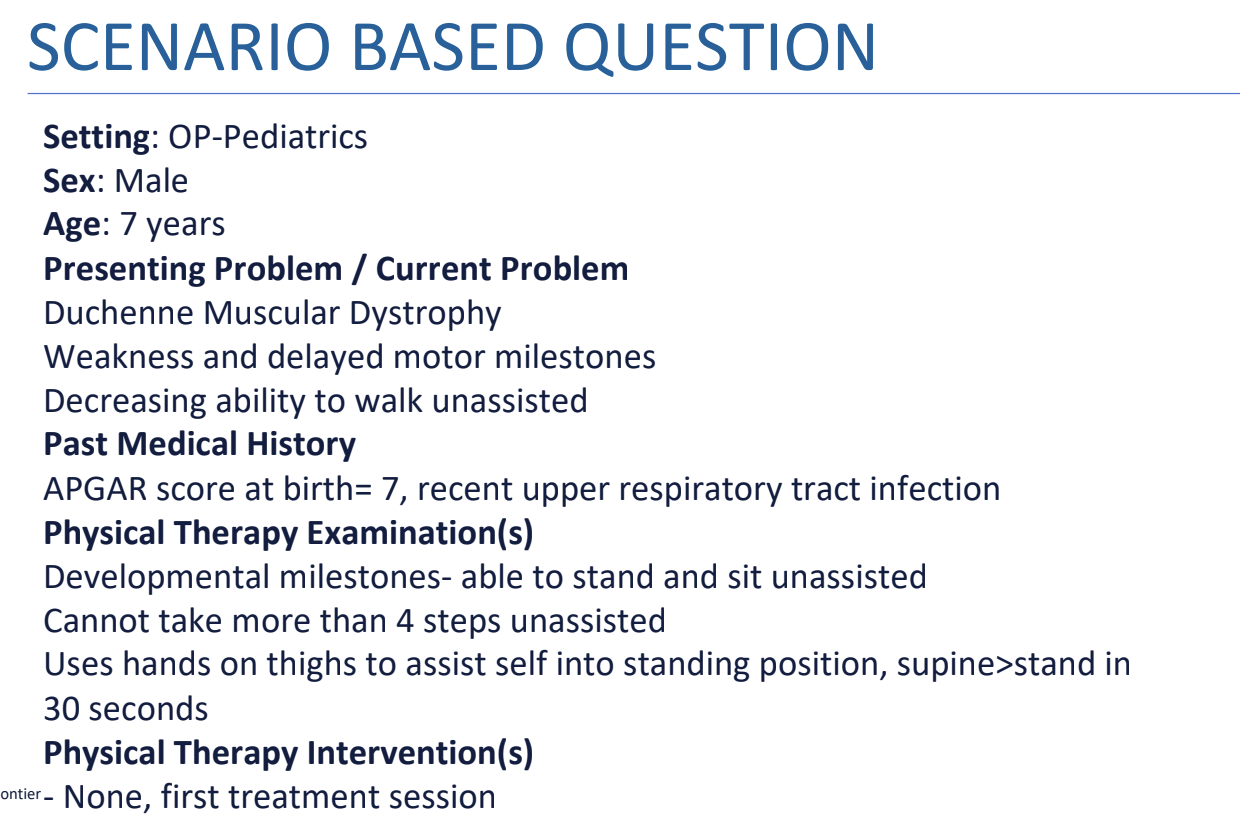
Practice Question 5.1
Which of the following is the MOST APPROPRIATE physical therapy goal for this patient?
A. Inhibition of abnormal muscle tone and reflexes
B. Improvement of strength and muscle tone
C. Assessment of an appropriate ambulatory assistive device
D. Use of a standing frame for therapeutic standing
C. Assessment of an appropriate ambulatory assistive device
RATIONALE: PT goals include preservation (not increased in) strength, positioning and stretching to prevent the development of contractures, and assessment of adaptive equipment to prolong function. The PT would also play a role in determining the appropriate use of assistive devices that could help maintain the child’s mobility such as walkers and orthoses. Muscle tone is low in patients with DMD and does not need to be further inhibited. Strength may be preserved for a time, but is not expected to make a clinically significant increase due to the progressive nature of the disease, we will only maintain!!. The patient is able to stand unassisted at this time and does not need a standing frame.

Practice Question 5.2
Which of the following observations is MOST LIKELY in this patient?
A. Decreased lumbar lordosis
B. Atrophy and decreased girth of the lower extremities
C. Toe drag during gait
D. Distal weakness more significant than proximal weakness
C. Toe drag during gait
RATIONALE: Typical observations in a patient with DMD include increased lordosis of the lumbar spine and kyphosis of the thoracic spine.
The calves can be observed to be enlarged due to increased adipose tissue replacing muscle tissue, termed pseudohypertrophy.
Proximal weakness is first noted, as early as approximately 3 years of age.
Toe drag may be observed related to a tendency to have plantarflexion contractures due to pseudohypertrophy.
Practice Question 5.3
Which of the following additional assessments would be MOST IMPORTANT to consider with the patient’s diagnosis?
A. Forced Vital Capacity
B. Sensory screening
C. Vision screening
D. Atlantoaxial stability
A. Forced Vital Capacity
RATIONALE: During the progression of muscular dystrophy, respiratory muscles are likely to be affected, and respiratory failure is a common cause of death. Usually have respiratory tract infections. Forced vital capacity can be used to assess and track respiratory function.
Sensory screening can be done but is not as imperative to the patient’s life expectancy and is not specific to DMD.
Visual disturbances are not typical of DMD.
Atlantoaxial instability is a trademark symptoms of Down Syndrome.
What is the inheritance for Duchenne Muscular Dystrophy?
What gene is missing?
this causes what symptom?
x-linked recessive, inherited by boys
Dystrophin gene missing - destruction of muscles’ cells
causes pseudohypertrophy
collagen and adipose tissue or fat replace where the muscle once was
usually in the calves
have enlarged calves, but just lumpy weak adipose tissue
For DMD, what things are included in the examination? (6)
look at what alignment, function, needs?
strength
ROM
functional testing
skeletal alignment
cardiopulmonary function
assess need for adaptive equipment
PT interventions for DMD:
maintain what 3 things?
do not do what?
maintain mobility and preserve strength
maintain joint ROM actively/passively
DO NOT OVERFATIGUE
may increase muscle breakdown
What is most seen in Duchenne Muscular Dystrophy?
posture, tone, movements, life expectancy
Gower’s sign
when standing up from the floor, they will walk their hands up their legs
due to weak LEs/quads, lock their knees out with their hands and put a different pressure against their knees
plantarflexion contractures —> toe drag during gait
contractures not only meaning high tone, but also seen in low tone patients
posture
exaggerated S-curve, protruding belly, increased lordosis/kyphosis
life expectancy
late childhood, early adulthood

Down Syndrome:
results from presence of full or partial extra copy of what?
increased risk with what?
which forceful activities/movements should be limited and due to what characteristic of the odontoid ligament? and potential for a subluxation of what joint?
encourage what function and avoid hyperextension of what two joints during WB activities?
copy of the 21st chromosome; trisomy 21
increased risk with increased age of the mother
forceful neck flexion and rotation activities should be limited due to laxity of odontoid ligament and potential for a subluxation of atlanto-axial joint
encourage motor function and avoid hyperextension of elbows and knees during weight bearing activities
pts have low tone, don’t want them to be locking out
Practice Question 6
A child with Down’s Syndrome has moderate developmental delay, hypotonia, and incoordination, and can walk with assistance. What is the MOST APPROPRIATE physical therapy treatment for this patient?
A. Standing and pushing a cart full of toys
B. Sit-to-stands to build strength
C. Rolling and somersault activities
D. Rhythmic stabilization of postural extensors in sitting
A. Standing and pushing a cart full of toys
RATIONALE: Pushing the toy cart while standing. Patients with Down’s syndrome have hypotonicity and should be encouraged to perform weight bearing exercises along with developing gross and fine motor skills. Pushing the toy cart is more functional than sitting and will help in improving the tone and strength. It will also help the child to avoid hyperextension in standing as they will be flexing forward to push the cart.
Somersault activities are contraindicated due to atlantoaxial joint instability.
A two-year-old patient will not likely focus on sit to stands and sit to stand does not focus on a functional activity for a child (playing).
Encourage maximal level- body weight support decreases Wbing
Postural extensors in sitting would cause hyperextension/locking out
Symptoms of Down Syndrome:
___-tonia, ligamentous laxity
delayed ___ milestones (which 2 are most delayed?)
deficits in memory and ___ language
impairments in ___ control and coordination
decreased strength in what 2 LE muscles?
inefficient ___ strategies due to ___
hypotonia, ligamentous laxity
delayed motor milestones (running and jumping most delayed)
deficits in memory and expressive language
impairments in postural control and coordination
decreased quadriceps and hip abductor strength
inefficient movement strategies due to hypotonia
Autism spectrum disorder:
which 2 skill limitations and especially which skills?
repetitive behaviors such as? (3)
what processing issues?
difficulty developing what?
hypo-/hyper-reactive to what?
sensory seeking or what?
dyspraxia?
social/communication skill limitations, especially non-verbal skills
repetitive behaviors such as routines, highly focused interest, spinning of hands
sensory processing issues
difficulty developing relationships
hypo-/hyper-reactive to sensory input
sensory seeking or sensory avoiding
dyspraxia = inability to imitate movement
Interventions for ASD:
controlled, ___-sensory input
give specific __
what interventions?
encouraging ___ development
what component?
visual supports such as?
using first, ___ or what?
consistency
controlled, multi-sensory input
give specific instructions
behavioral interventions
encouraging motor development
coordination
visual supports such as lines on the floors for gait
using first, then or sequencing
consistency
Practice Question 7
A 16-year-old male presents to physical therapy with mid-back pain and a hyperkyphotic posture. X-rays show anterior wedging of the thoracic spine. Which of the following exercises is MOST APPROPRIATE for managing this condition?
A. Thoracic extension exercises on a stability ball
B. Thoracic flexion exercises in a seated position
C. Stretching of the thoracic extensors
D. Strengthening of the pectoral muscles
A. Thoracic extension exercises on a stability ball
RATIONALE: Scheuermann's kyphosis involves excessive thoracic flexion, so the focus is on improving thoracic extension and strengthening the back extensors to correct posture.
Thoracic extension exercises on a stability ball specifically target this goal.
Flexion exercises or strengthening the pectoral muscles would further promote forward rounding, worsening the condition.
Stretching the thoracic extensors would also be counterproductive, as these muscles need strengthening, not lengthening.
Scheuermann Disease - Examination:
Schmorl’s nodes and angled/wedged what??
pain with what movements?
aggravation with long periods of what (2)?
what posture?
what population?
Schmorl’s nodes and angled/wedged thoracic spine
pain with thoracic extension and rotation
aggravation with long periods of standing/sitting or physical activity
increased thoracic kyphosis/lumbar lordotic curve
younger male patients
PT Interventions for Scheuermann Disease:
what method?
stretch?
strengthen? (2)
Schroth method (also used for scoliosis)
stretch pecs
strengthen thoracic extensors and scapular stabilizers
Sch Sch Sch = scheuer, schmorl’s nodes, schroth method
Practice Question 8
A patient reports loss of sensation over the ulnar side of the hand. The patient has weakness in the intrinsic hand muscles leading to nonfunctional hand. Which of the following is the MOST LIKELY diagnosis?
A. Radial nerve palsy
B. Erb’s palsy
C. Klumpke’s palsy
D. C6 radiculopathy
C. Klumpke’s palsy
RATIONALE: C5-C6 nerve roots are involved in Erb’s palsy. Muscles of shoulder and elbow are affected due to injury at the Erb’s point. Muscles of the hand are spared. Where Klumpke’s paralysis leads to a non-functional hand. Loss of sensation is over the radial arm in case of erb’s palsy and over ulnar arm in case of Klumpke’s palsy.
C6 radiculopathy is radial side of the forearm and thumb
Radial nerve palsy: brachioradialis, finger extensors, wrist extensors, triceps will all be affected, drop wrist deformity
Erbs: waiter’s tip deformity C5-C6
Klumpke: C8-T1
Erb’s Palsy:
what are the nerve roots?
MOI?
loss of movements?
deformity?
Erb’s palsy C5-C6 - Erb = 5r6
MOI
stretching head downward
loss of movements
loss of abduction and lateral rotation of the shoulder
deformity
waiter’s tip deformity - forgot to tip waiter
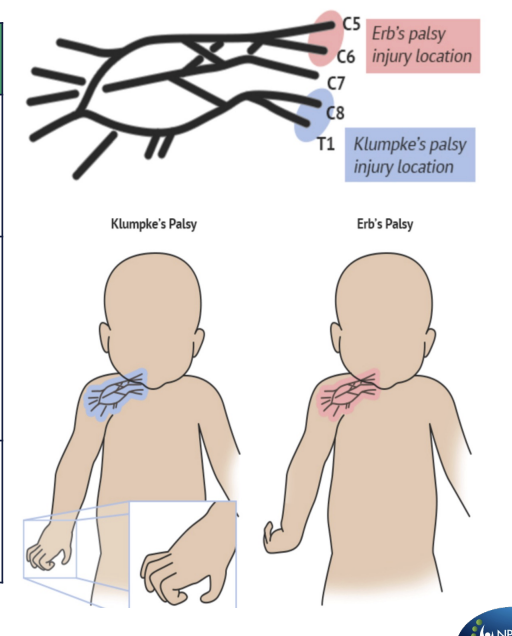
Klumpke’s palsy:
what are the nerve roots?
MOI?
loss of movements?
deformity?
Klumpke’s palsy C8-T1 - Kl = 81
MOI
stretching of arm overhead
loss of movements
paralysis of the intrinsic of the hand
deformity
claw hand - like pulling out a clump of grass
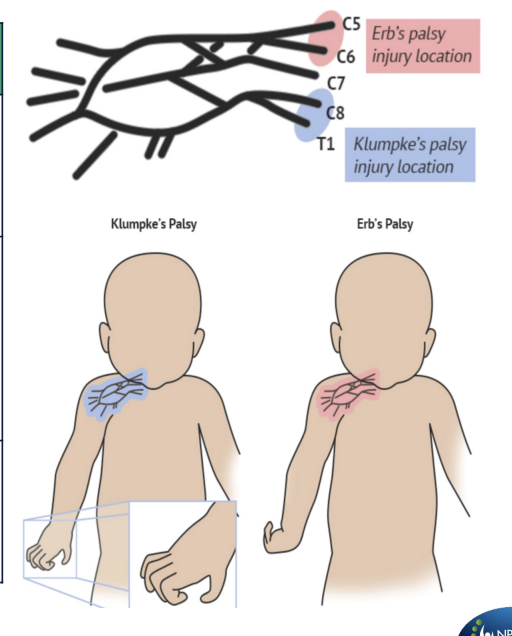
What is treatment for both Erb’s and Klumpke’s palsy?
immobilization then gentle ROM