PD Exam 3: Female Genitalia/Rectum/MSK/Behavioral Health
1/515
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
516 Terms
the rectal wall has 3 inward foldings called?
valves of houston
internal anal sphincter
smooth muscle, involuntary, vascular
external anal sphincter
skeletal muscle, voluntary
what is the external anal sphincter innervated by?
perineal branch of sacral nerve 4
anorectal junction
pectinate or dentate line; Serrated line marking change from skin to mucous membrane NOT palpable
squamocolumar junction
Squamous epithelial cells meet columnar cells
prostate gland
heart shaped organ that surround the urethra, two lateral lobes palpable during rectal exam
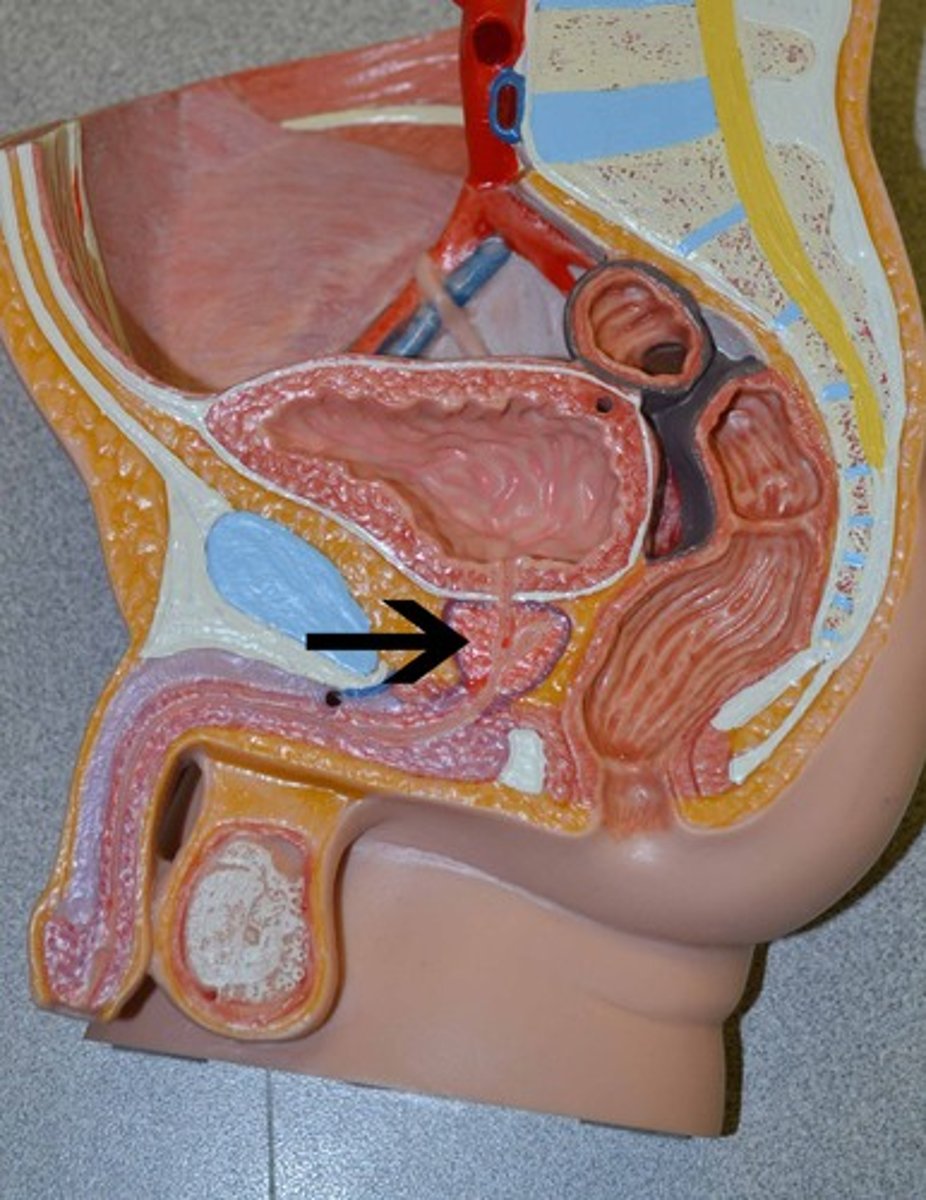
seminal vesicles
Saclike structure above prostate that are shaped like rabbit ears
Not palpable
Fluid component of semen production
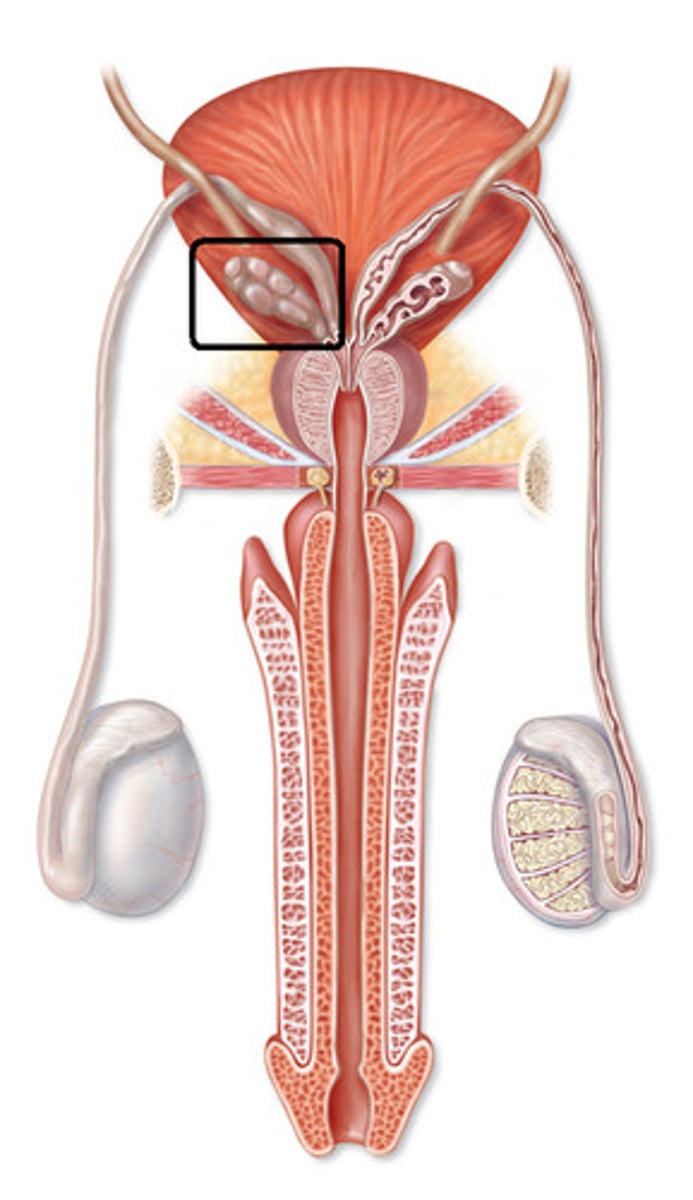
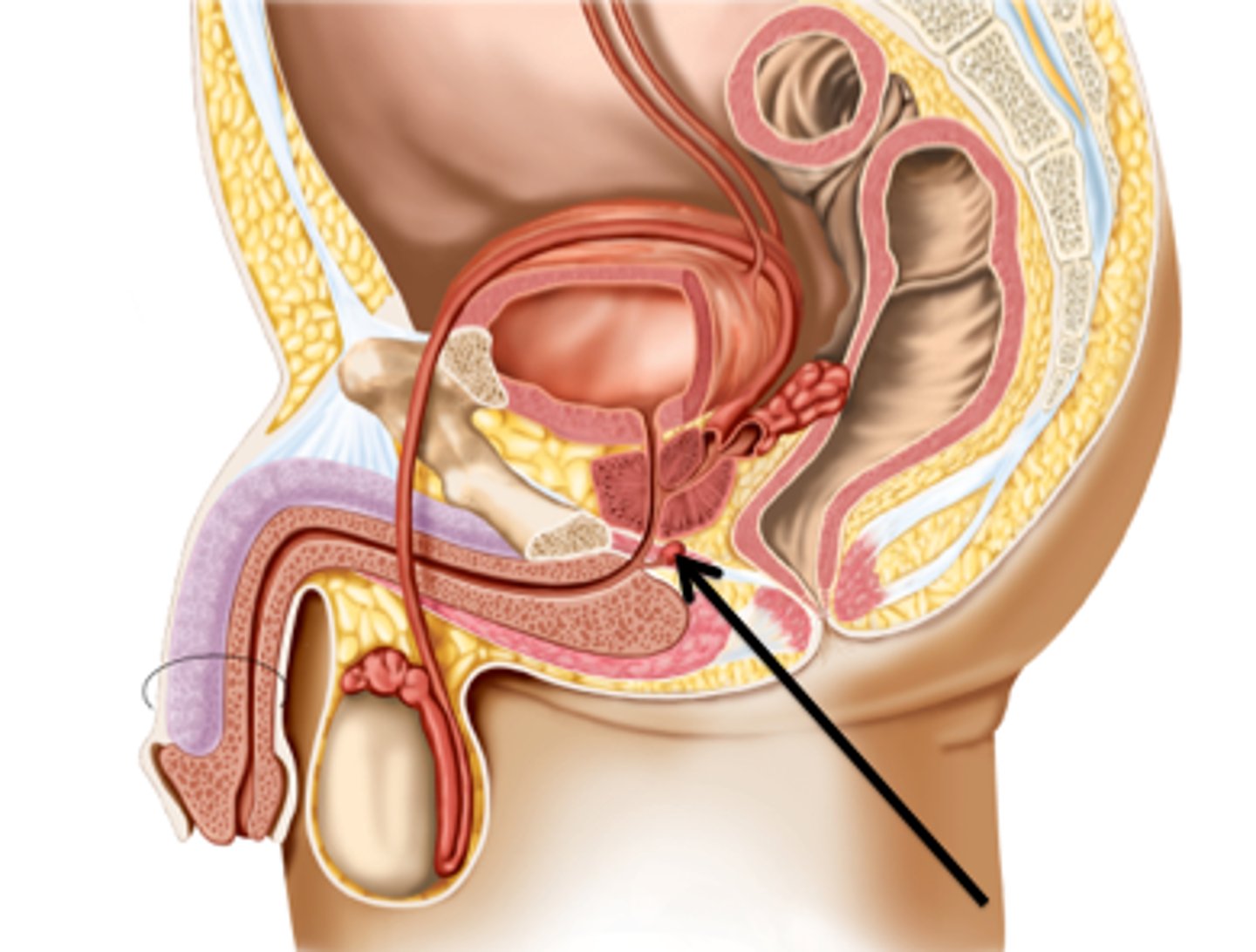
cowper's gland (bulbourethral glands)
Located at the base of the penis
Produces Pre-ejaculate and Prostate Specific Antigen (PSA)
what is the best position for a male rectal exam?
Stand leaning forward over examination table
what should you inspect the sacrococcygeal area and perineum for?
Lumps
Ulcers
Inflammation
Rashes
Excoriations
Fissures
how do you assess for sphincter tone of the anus?
have pt bear down and assess for..
Tenderness
Induration
Nodules/masses
Lesions
what structures are palpable anteriorly on a rectal exam in a male?
Full bladder
Urethra if catheterized
Bulbourethral glands
Prostate
what structures are palpable anteriorly on a rectal exam in a female?
Vagina
Cervix
Body of uterus when retroverted
Rectouterine fossa
what structures are palpable laterally on a rectal exam?
Ischial tuberosity and spine
Sacrotuberous ligament
what structures are palpable posteriorly on a rectal exam?
pelvic surface of sacrum and coccyx
Stool Guaiac Test Or Fecal Occult Blood Test Or Hemoccult (FOBT)
Detect blood invisible in the feces
Perform upon completion of physical exam
Occult blood testing is an adequate screen for colon CA t/f
false
1 multiple choice option
Pilonidal Cyst
Congenital cyst formation (part of newborn exam)

presentation of pilonidal cyst
Small tuft of hair surrounded by halo of erythema
May be asymptomatic with little drainage
Can complicate to abscess, and/or fistula formation. Often recurrent.
internal hemorrhoids
Enlargements of normal vascular cushions located above pectinate line
NOT painful

external hemorrhoids
Originate below pectinate line and covered with skin
Anal pain only if thrombosed

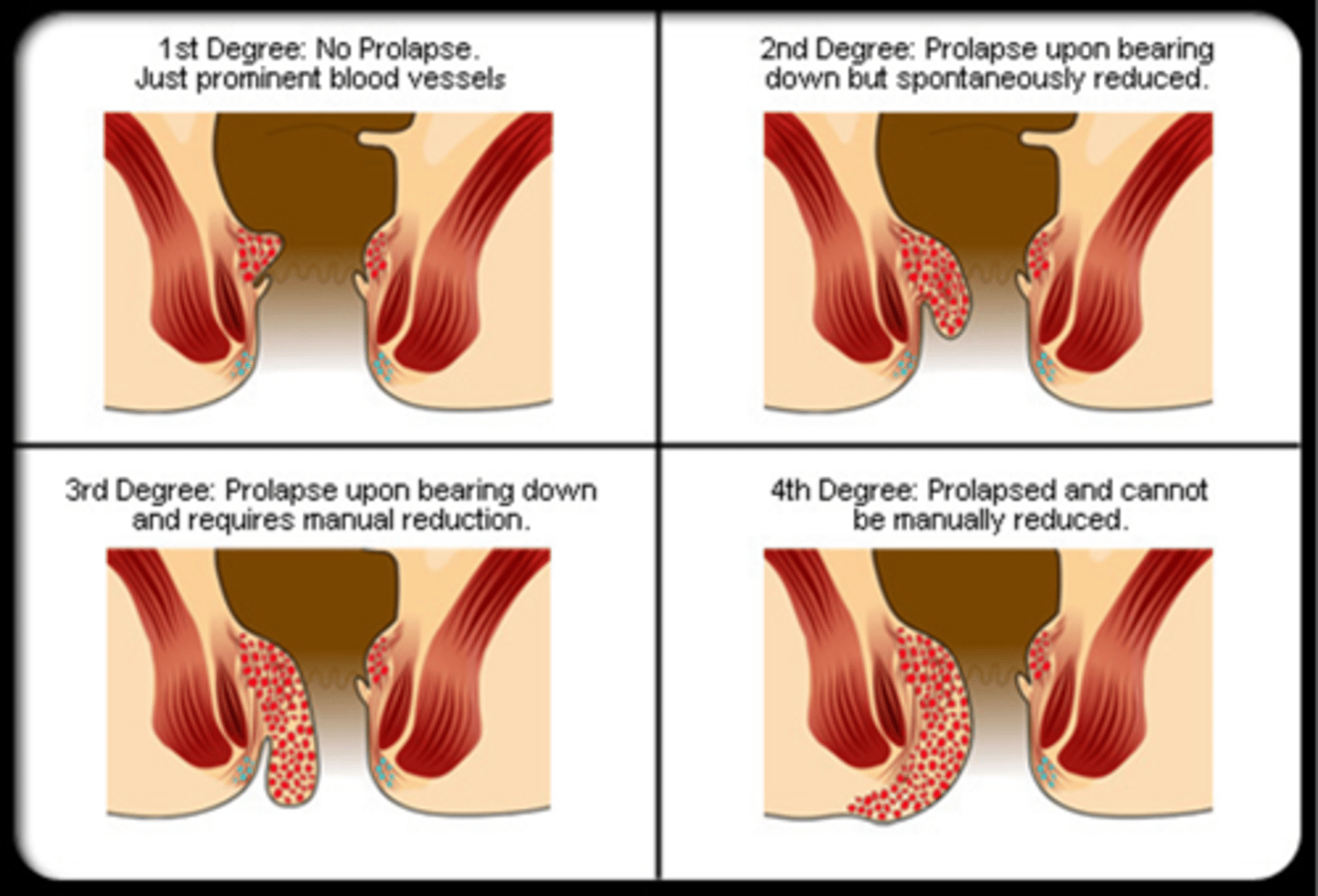
what are the 4 degrees of hemorrhoids?
1st Degree – confined to anal canal
2nd Degree – Mucosal prolapse during straining with spontaneous reduction
3rd Degree – Manual reduction required
4th Degree – Chronic protruding mucosa
rectal procidentia
rectal prolapse

symptoms of rectal prolapse
Fecal incontinence
Rectal bleeding
Mucous discharge
anal fissure
Oval ulceration of anal canal
Associated with constipation, diarrhea, infection, perianal trauma, Crohn's disease

where are anal fissure most commonly location and what may they have just below?
midline - posterior; sentinel skin tag
symptoms of anal fissure
Anal pain
Irritation
Mild hematochezia
anorectal fistula
Inflammatory tract which opens at one end into the anus or rectum and at the other end onto the skin surface
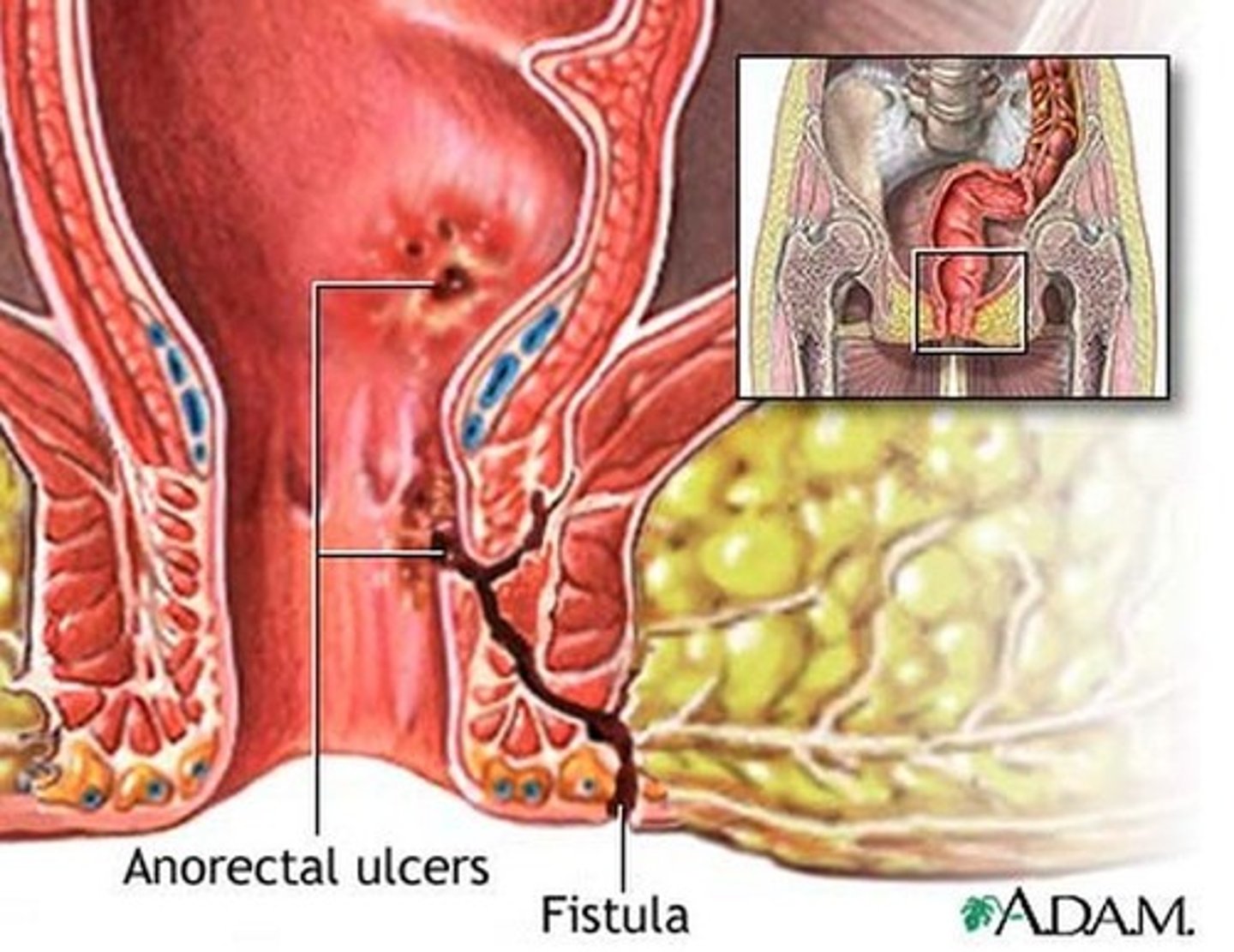
what are 10% of anorectal fistulas associated with?
IBD
symptoms of anorectal fistula
Throbbing pain
Drainage- may increase with defecation
Firm mass
rectal polyps
Pedunculated or Sessile, Soft, Usually asymptomatic but patient may have:
Blood in the stool
Pain, diarrhea, constipation
what are risk factors for colorectal carcinoma?
family hx, diet
what are symptoms of colorectal carcinoma?
May be asymptomatic
Insidious blood loss- symptoms of iron def. anemia (fatigue, palpitations)
Can manifest as an obstruction
Abdominal cramping
Hematochezia, tenesmus, change in stool caliber (pencil thin stools)
Weight loss
Firm, nodular mass on exam
where does an anal carcinoma occur?
between anorectal ring to halfway between the pectinate line and the anal verge
what are anal carcinomas often related to and what are symptoms?
HPV;
Bleeding
Anal pain
Annular mass
Pruritus
prostatits
inflammation of the prostate
symptoms of acute bacterial prostatits
Fever
Urinary symptoms (frequency, urgency, dysuria, incomplete voiding)
Low back pain
Rectal pain
PE of acute bacterial prostatitis
Gland is tender, swollen, boggy and warm on palpation
symptoms of chronic bacterial prostatitis
Asymptomatic
Dysuria or mild pelvic pain
Chronic low grade pelvic/urinary pain/problems
PE of chronic bacterial prostatitis
Normal prostate exam
what is chronic bacterial prostatitis associated with?
recurrent urinary tract infections
symptoms of chronic non bacterial prostatitis (chronic pelvic pain syndrome)
Irritative voiding symptoms
Similar to chronic bacterial prostatitis but show no evidence of prostate infection or UTI
PE of chronic pelvic pain syndrome
Assess for prostate induration or asymmetry to R/O carcinoma
Generally no abnormality appreciated on prostate exam
benign prostatic hyperplasia (BPH)
Nonmalignant enlargement of prostate gland
symptoms of irritative BPH
urgency, frequency, nocturia
symptoms of obstructive BPH
Hesitancy
Decreased force and caliber of the stream
Sensation of incomplete bladder emptying
Post void dribbling
Straining
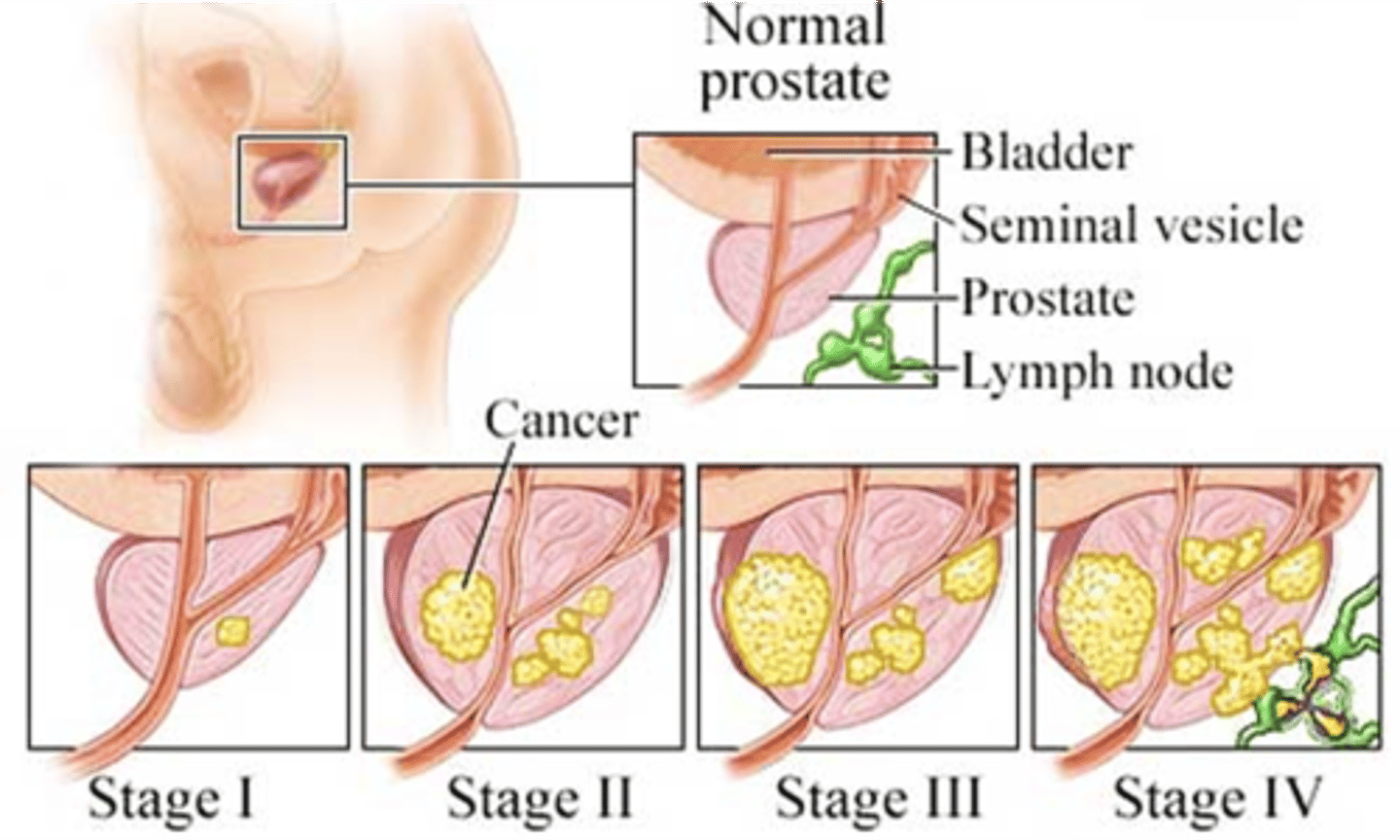
prostate cancer
Suggested by an area of hardness/nodule in the gland
Distinct hard nodule that alters the contour
Rarely presents with signs of urinary retention
what is the most common site of metastasis in prostate cancer?
axial skeleton
as prostate cancer enlarges...
Feels irregular
Extend beyond confines of gland
Median sulcus obscured
what are the stages of prostate cancer?
Stage I: Small and only in prostate
Stage II: Still within prostate but larger and may involve both sides of the prostate
Stage III: Cancer has spread beyond the prostate to nearby tissues
Stage IV: Cancer has spread to distant parts of the body such as lymph nodes
what are prostate cancer risk factors?
age, ethnicity, family hx, meds, environmental, diet
how far does breast tissue expand?
Extends from the inferior clavicular line to the inframammary fold, and from mid sternum to the axilla
anatomy of the areola and nipple
Pin-point openings
Small bumps
Smooth muscle
Sensory Innervation
Montgomery gland
aveoli
glandular tissue that makes milk
excretory duct
lactiferous duct that transports the milk; "highways"
lactiferous sinuses
storage of milk; "holding tanks"
what are 4 chains of axillary lymphatic's and how do they drain?
Central (deep in axilla)
Pectoral (anterior)
Lateral (proximal humerus)
Subscapular (posterior)
Pectoralis/Lateral /Subscapular → Central → Infraclavicular/Supraclavicular
what are the 5 tanner stages of breast development?
Stage 1 - preadolescent
Stage 2 - breast bud
Stage 3 - further enlargement, elevation of areola and breast
Stage 4 - projection of areola and nipple, secondary mound
Stage 5 - Mature stage. Projection of only, areola recedes to general contour of breas
what are the recommendations for clinical breast exams?
20-40 - at least every 3 years
40 and up - annually
CBE replace mammography t/f
false
1 multiple choice option
when doing a CBE, you notice your patient has a inversion nipple, should you be concerned?
no, only concerning if happens out of the blue/not normal for the patient
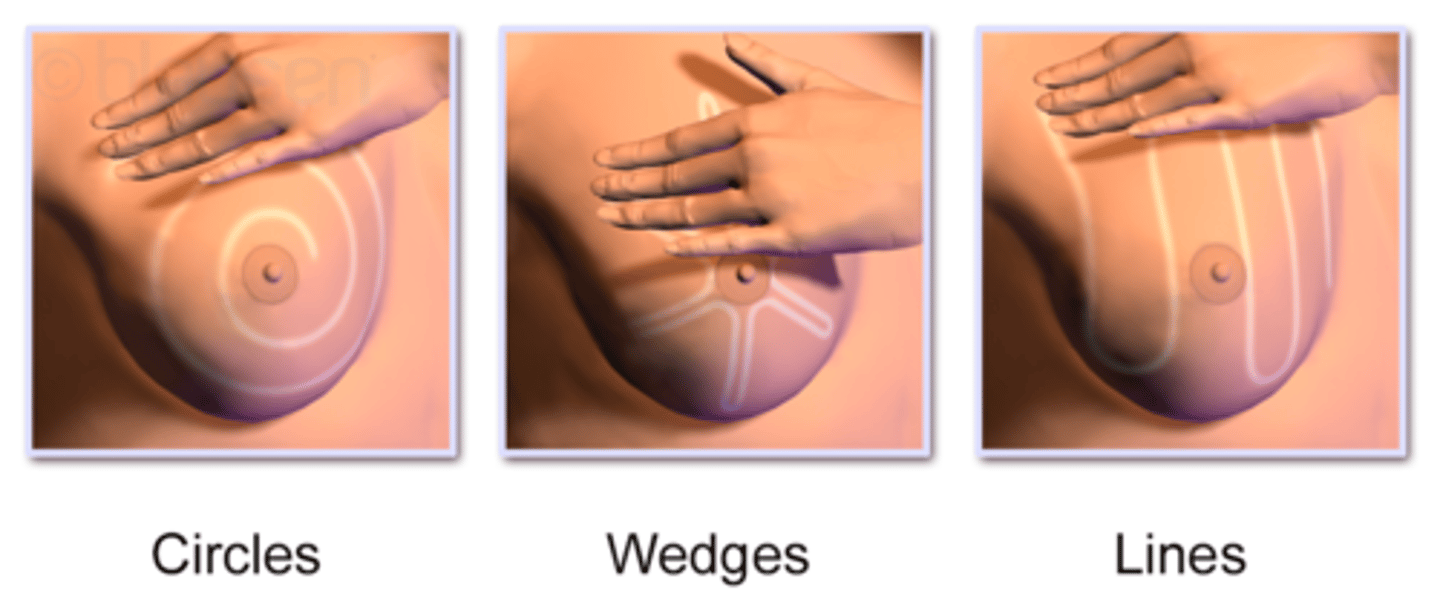
what are the methods of palpation for a CBE?
Circles
Wedges
Lines
why is noting the consistency of tissue during a CBE important?
Physiologic nodularity
+/- inframammary ridge
what are you accessing during palpation for tenderness in a CBE?
Premenstrual fullness
Fibrocystic tissue
what lymph nodes are you palpating during an axillae exam?
Central
Pectoral
Lateral
Subscapular
Supra/infraclavicular
what are some types of breast surgies?
Mastectomy
Lumpectomy
Augmentation
Reduction
Reconstruction
mastectomy
removal of all breast tissue
lumpectomy
removal of some/a lot or little tissue (not all)
aumentation
breast implants; normally will be no breast tissue
reconstruction
after mastectomy to rebuild shape/look of breast
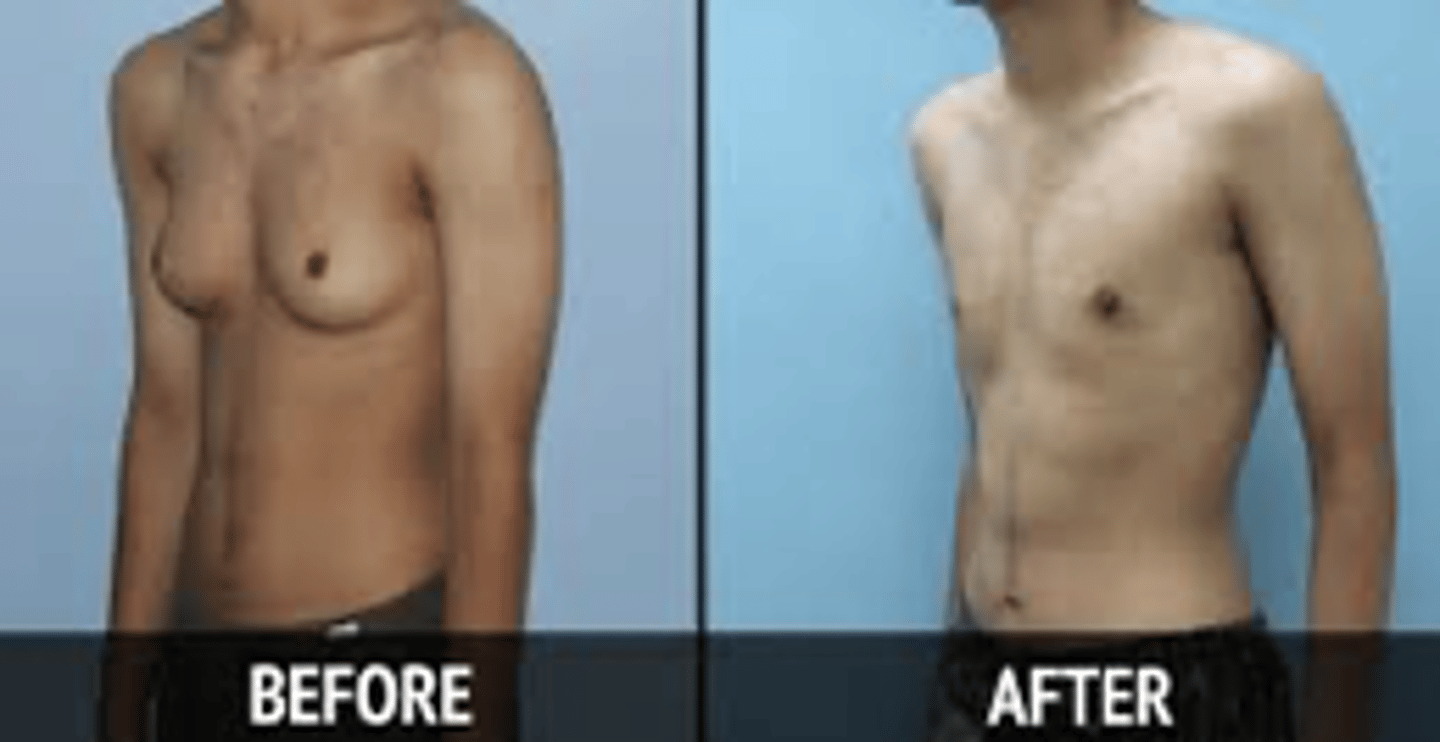
Gynecomastia
enlargement of breast tissue in males - harder to identify in larger men but will have other signs like the nipple
Self breast exam
no longer recommended however breast self-awareness is still important (Encourage patients to just be familiar with their bodies!)
name 4 types of breast masses
fibroadenoma
cyst
fibrocystic disease
cancer
fibroademona
15-25 yo
Single or multiple
Round, disc or lobular
Usually firm
Well-demarcated
Mobile
Nontender
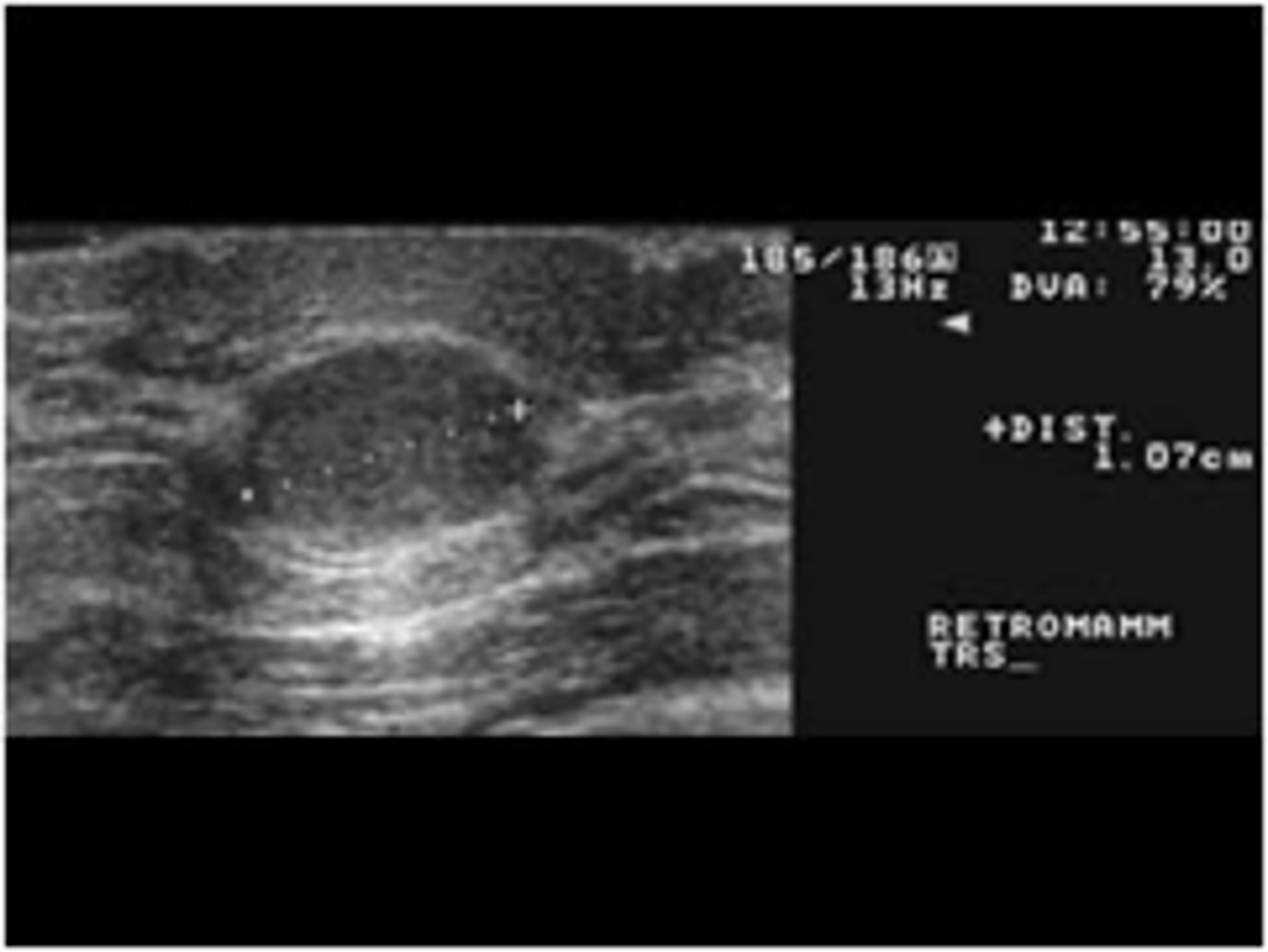
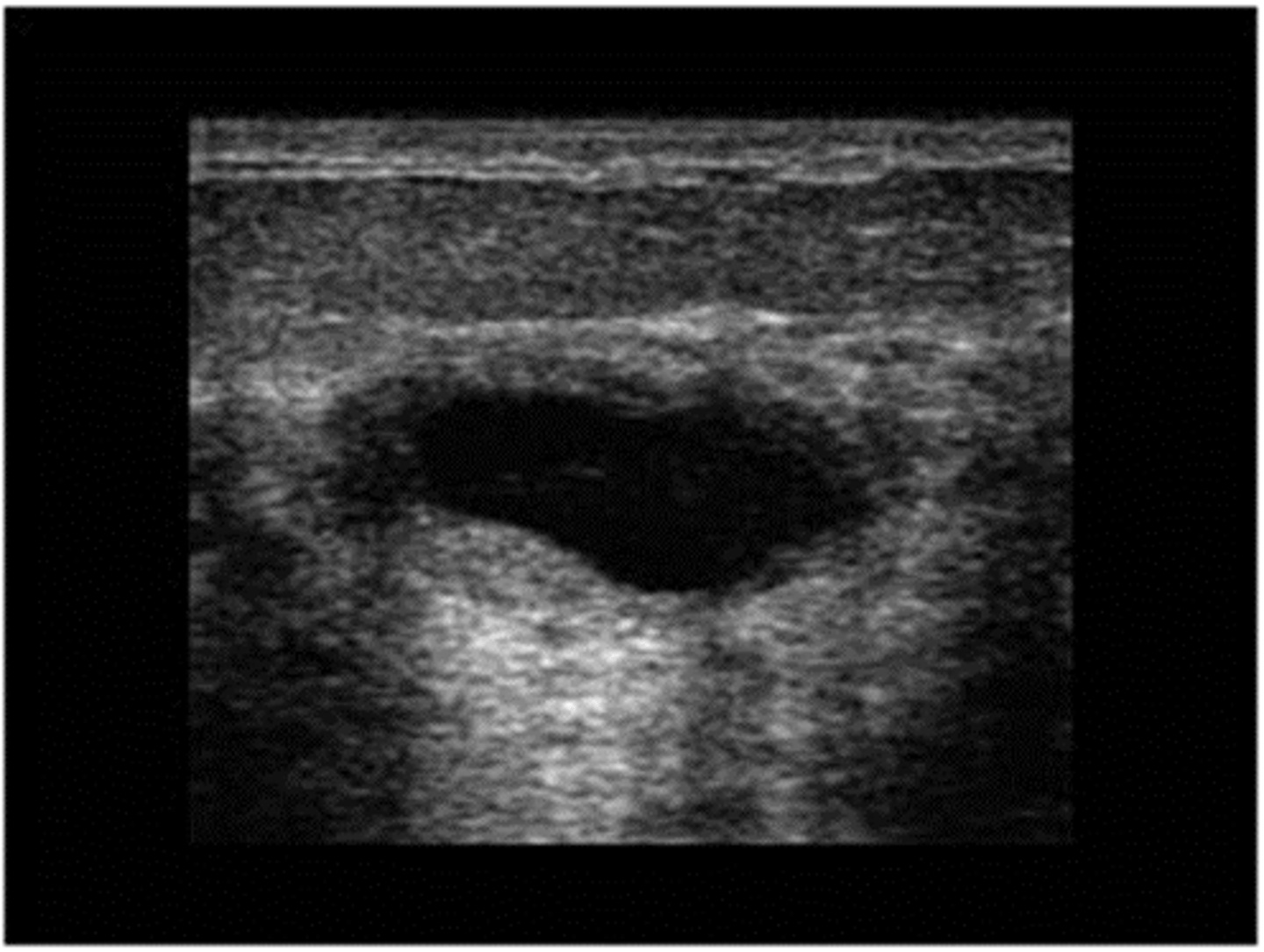
cyst
30-50 yo
Regress after menopause
Single or multiple
Round
Soft/firm, rubbery
Well -demarcated
Mobile
Often tender
fibrocystic disease
25-50
Nodular, rope-like densities
+/- tender
what is the most common cause of cancer in women?
breast cancer
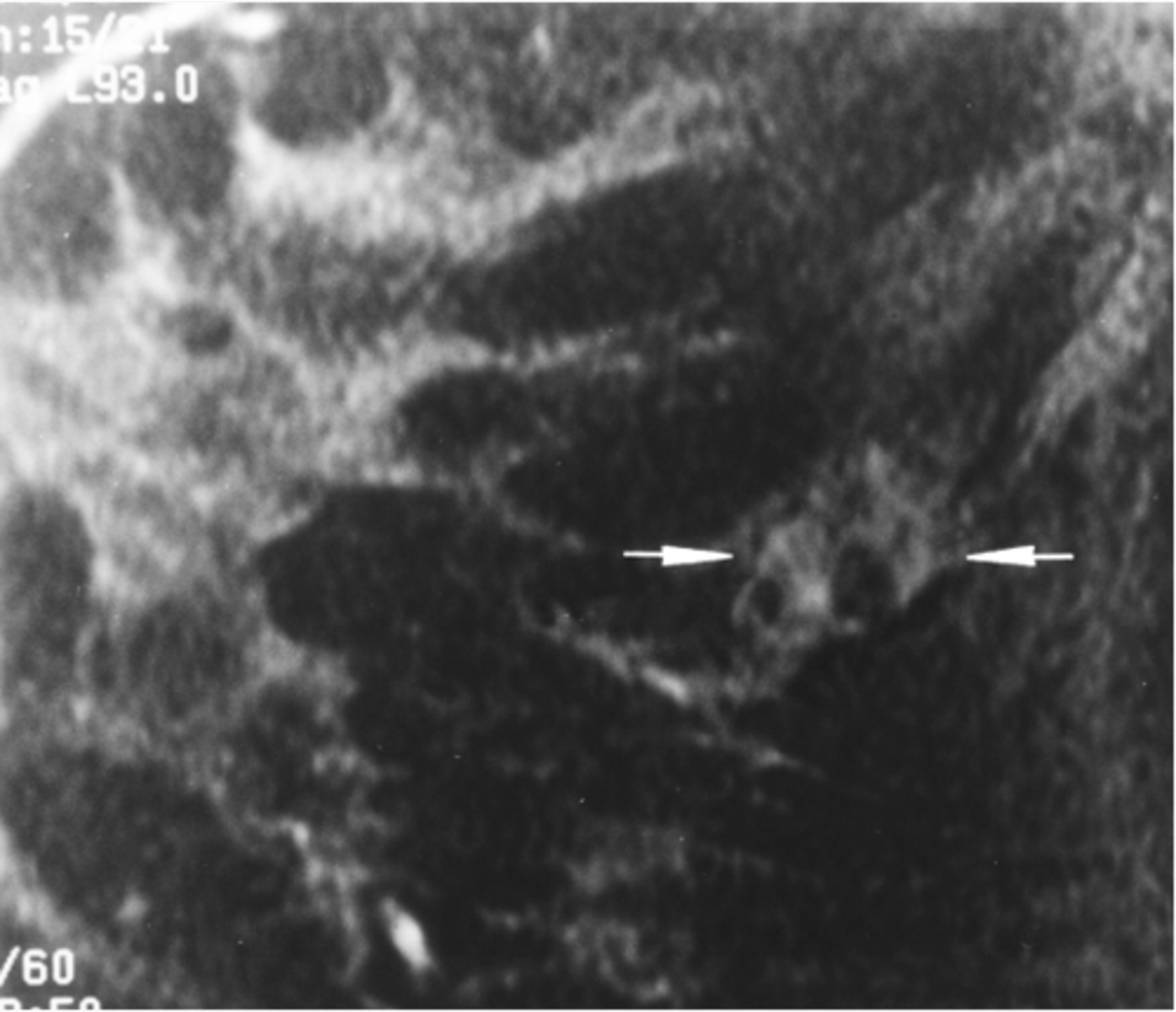
breast cancer
30-90 yo (mostly > 50)
Usually single mass
Irregular or stellate shape
Firm, hard consistency
Not well-demarcated
May be fixed
Usually nontender
May see skin changes or nipple retraction
what are non-modifiable risk factors for breast cancer?
Gender
Age
Race
Family history
Early menarche
Late menopause
High breast density
what are modifiable risk factors for breast cancer?
Postmenopausal obesity
Use of combination HRT
Alcohol use
Physical inactivity
Estrogen containing contraceptive use
Nulliparity
>30yo at first full-term pregnancy
Never breast fed a child
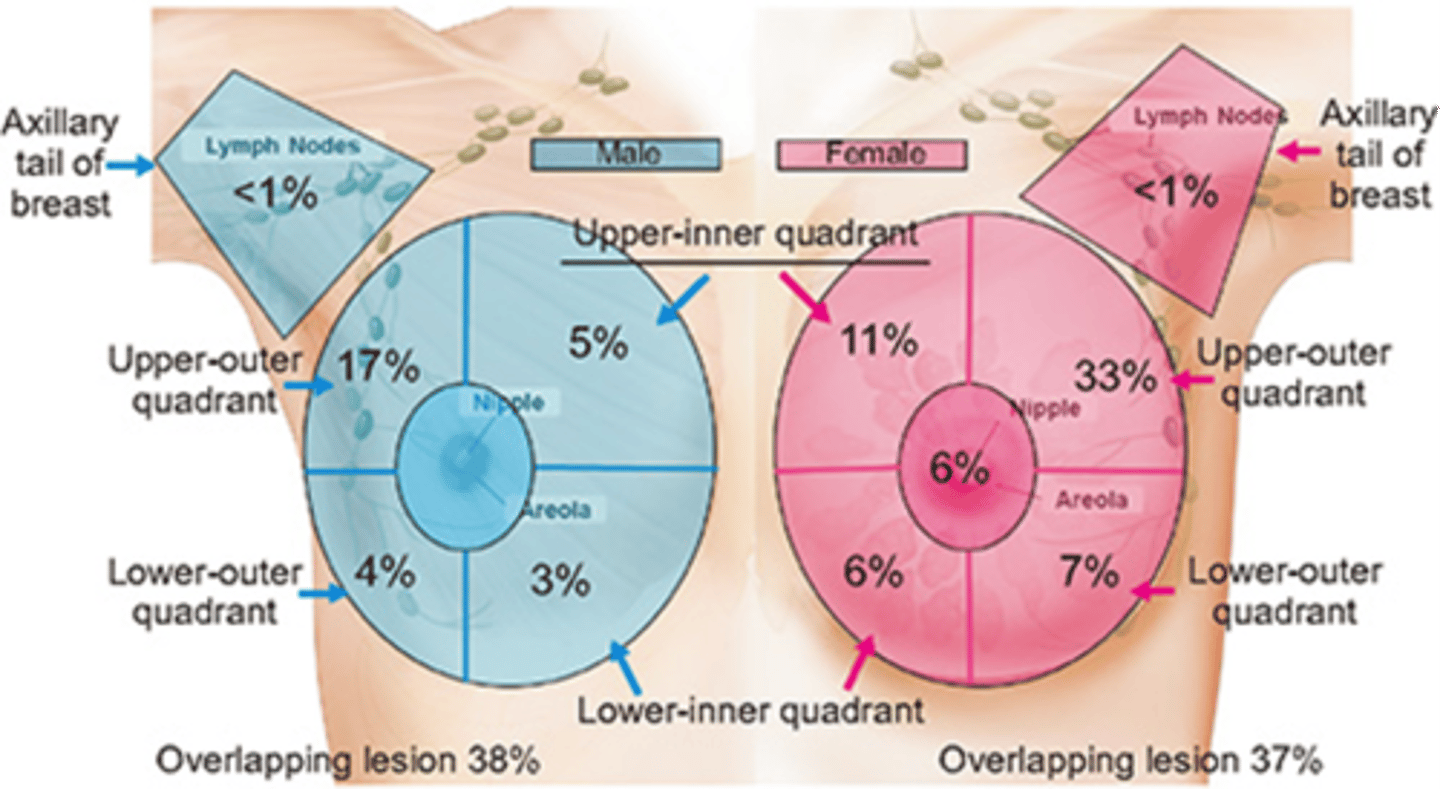
what area of the breast (in males and females) is at highest risk for breast cancer?
upper outer quadrants
what are changes are on PE on the breast that can be associated with cancer?
Retraction, dimpling, contour change
Nipple retraction/deviation

peau d-orange
Code orange (looks like an oranges skin)
Sign of inflammatory breast cancer

inflammatory breast cancer
the most aggressive and least common form of breast cancer; Automatic grade 4

pagets disease of the nipple
uncommon form of breast cancer, starts as scaly eczema like lesion that may weep, crust, or erode

what is the best way to screen for breast cancer?
mammography
Traditional mammography
low dose x-ray with images viewed on 2 dimensional film
Digital mammography
addition of digital technology allows images to be viewed on a computer screen
3D Tomosynthesis
addition of 3D technology allows images to be viewed in multiple planes/layers
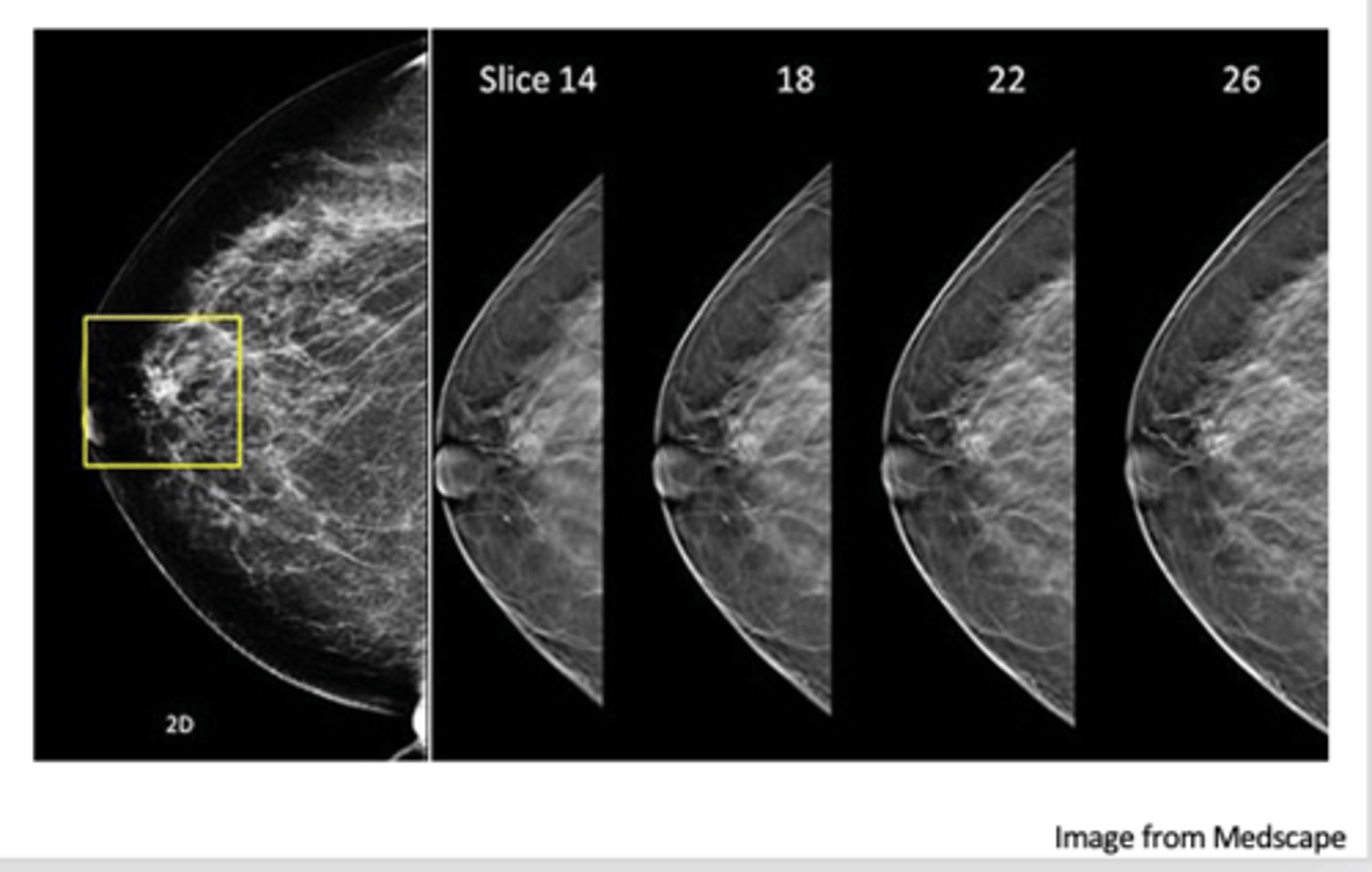
what is an advantage of 3D tomosynthesis?
Fewer false negative results
Fewer false positive results
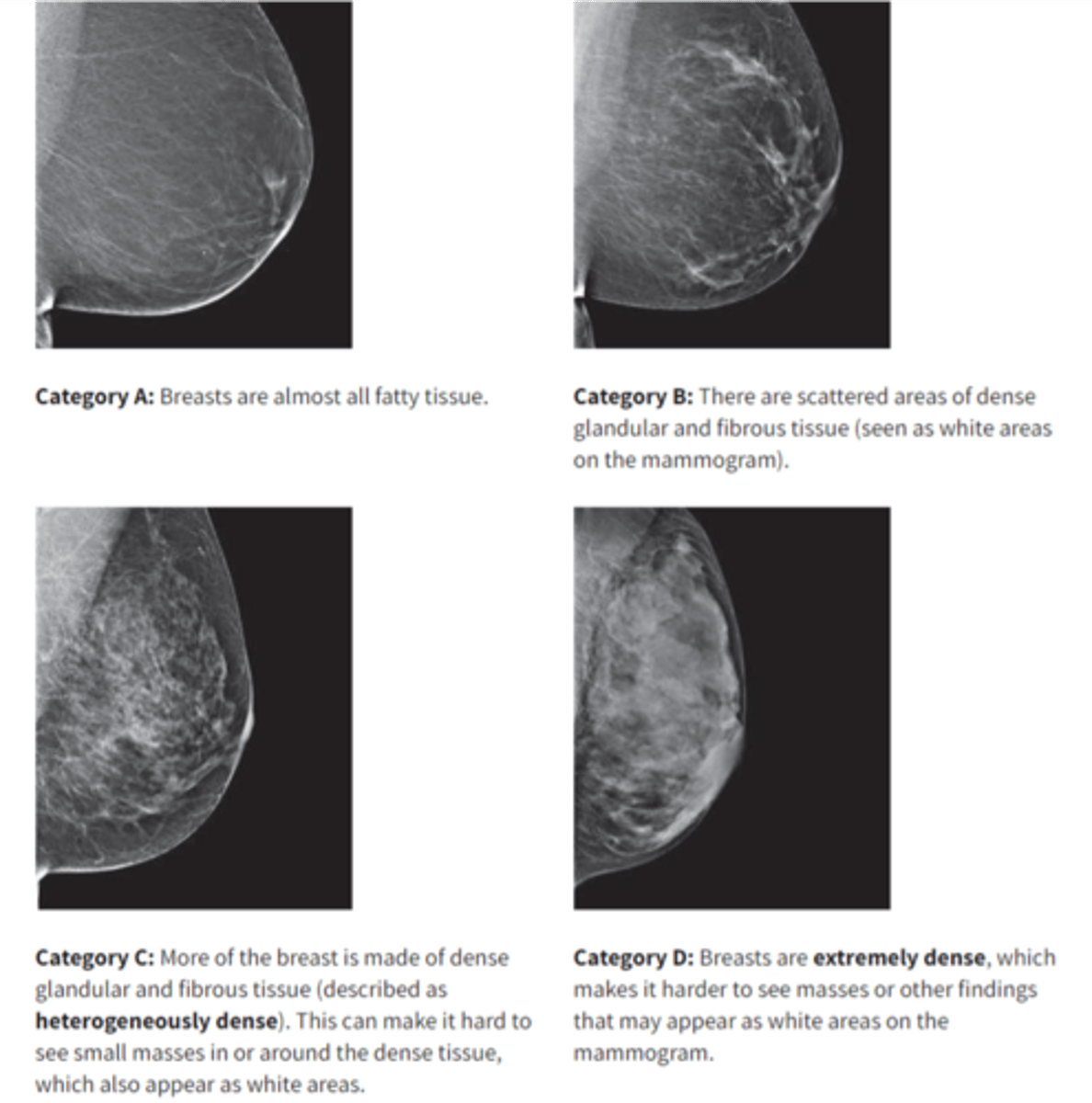
Increased breast density is known to increase breast cancer risk in what two ways?
1. As an independent risk factor
2. By obscuring small findings
what are the BI-RADS categories?
A- Almost entirely fatty
B- Scattered areas of fibroglandular density
C- Heterogeneously dense
D- Extremely dense
what are supplemental screening tools for dense breast?
Contrast Enhanced MRI
Whole Breast Ultrasound
Emerging Technologies
Contrast Enhanced MRI
More sensitive than mammography
Limited by cost and availability
Requires local expertise in reading breast MRIs
Whole Breast Ultrasound
Two types, handheld US and automated breast US
High risk of false positive results
Affect of repetitive doses of contrast gadolinium is unknown
what are the emerging technologies for screening dense breasts?
Abbreviated MRI
Molecular breast imaging
Contrast enhanced mammography
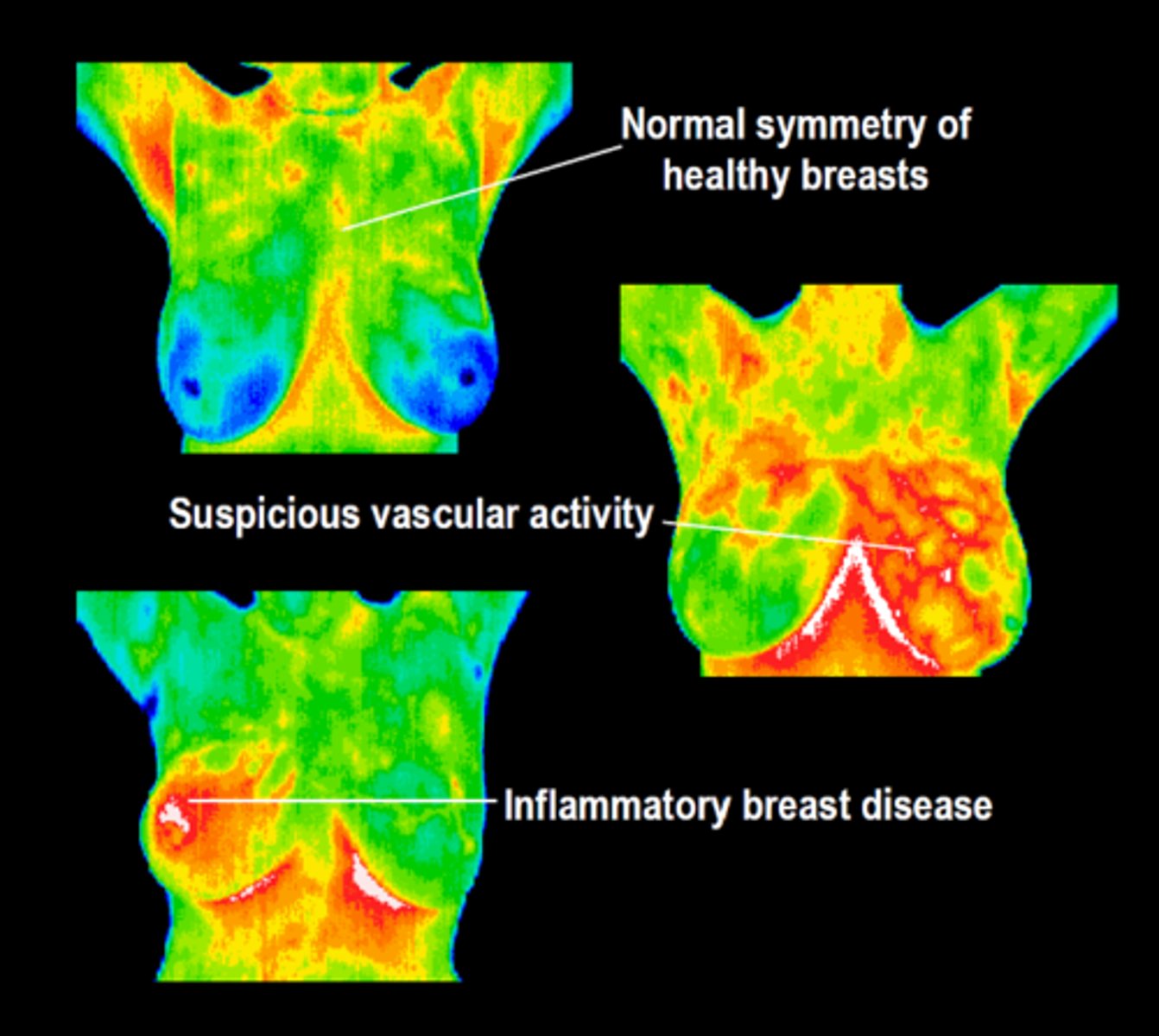
what is a potential future screening method that is approved by the FDA as an adjunct to mammography?
thermography
what genetic mutations increase the risk of possible breast/ovarian cancer?
BRCA1 and BRCA2
who should get a mammogram?
All women should be encouraged to have breast self- awareness.
All women age 40yo and older should be talking to their health care provider about breast cancer screening
All healthcare providers must be knowledgeable about screening modalities, risk, and benefits for the patient