Inflammation + Repair
1/50
Earn XP
Description and Tags
Dr. Burns lectures
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
Inflammation
Inflammatio - to set on fire
“-itis” : suffix that signifies inflammation
characteristics of inflammation
provoked response to tissue injury initiated by:
chemical agents
cold, hear
trauma
invasion of microbes
protective response: destroys, dilutes or confines the injurious agent
reparative response: induces and supports tissue repair
potentially harmful: ex: appendicitis that can burst and lead to other inflammation or death
types of inflammation
Acute
Chronic
Distinguished by duration, type of infiltrating inflammatory cells
cardinal signs of acute inflammation
Celcus:
pain
heat
redness
swelling
Galen:
loss of function
Physiological Responses and Symptoms of 4 cardinal signs
release of soluble mediators → swelling (tumor), pain (dolor)
vasodilation → heat (calor), redness (rubor), swelling (tumor)
increased blood flow → heat (calor), redness (rubor), swelling (tumor)
extravasation of fluid (permeability) → swelling (tumor)
cellular influx (chemotaxis) →swelling (tumor)
vascular events at moment of inflammation
First: brief vasoconstriction mediated by
autonomic nerves
direct vessel injury
release of vasoconstrixtors: endothelin-1, thromboxane A2, serotonin)
Second: active hyperemia - increase in organ blood flow
arteriolar smooth muscle relaxes → vasodilation
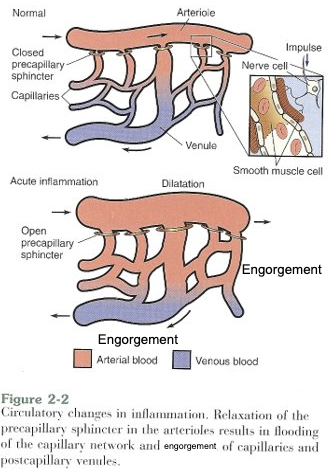
Active hyperemia
Vasodilation
Arteriolar smooth muscle cells relax → precapillary sphincter opens → blood flow increases → increased intravascular pressure→ tissue redness, swelling, warmth → transudate (protein-poor filtrate of plasma - LEAKY!!) leaves vessels → congestion → exudate comes in (protein-rich filtrate) → increases interstitial osmotic pressure → swelling/edema, lymphatic collapse (poor drainage)
exudate: protein-rich, supplies antibodies and complement to the affected area
Can swelling be beneficial?
Yes, it causes pain (dolor) → limits mobility around the affected area (loss of function)
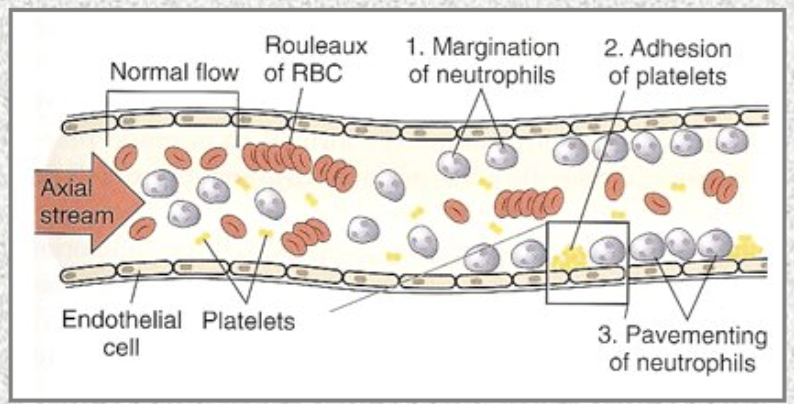
Stasis
loss of fluid from vasculature:
RBC concentrates (rouleaux)
blood viscosity increases
circulation around affected area slows down (stasis)
neutrophils accumulate and pavement along the vessel wall
PAGE 18
diapedesis
neutrophils leave the inflamed vessle by
margination and rolling
adhesion and transmigration
chemotaxis and activation
transmigration
neutrophils rolling on the endothelium until it can embed itself into the layers and exits thru the “aperture”
chemotaxis
neutrophils follow a chemical gradient to site of injury
soluble bacterial products
complement components
chemokines
LTB ( AA metabolite)
Neutrophil activation: binding of chemotactic agents to neutrophil surface receptors (assembly of contractile elements)
how does neutrophil kill bacteria?
opsonins: involves opsonization by IgG and C3b
oxygen-dependent killing: simply engulfing, driven by NADPH oxidase
pxygen-independent killing: fusion of phagocytic vacuole w lysosomes and cytoplasmic granules contaning hydrolyctic enzymes
oxygen-dependent killing (MOST EFFECTIVE)
ROS formed thru oxidative burst:
glycogen → glucose
glucose oxidation by the hexose monophosphate shunt generates NADPH
increased O2 consumpion (oxidative burst)
oxygen-independent killing
molecules inside neutrophils (granule, phagolysomes, etc) help kill bacteria
not as potent as ROS
degradation and clean up
dead microorganisms degraded by lysosomal acid hydrolases
hydrogen peroxide broken down to water and oxygen by catalase
neutrophil-induced tissue injury
neutrophil engulfs something too difficult to breakdown
degranulation occurs
frustrated phagocytosis
membranolytic substance
persistent leukocyte activation
mediator syystems — vasoactive amines
histamine: vasodilation and endothelial cell contraction, EC junctional widening and increased permeability
released by mast cells, basophils, platelets in response to
injury
immune rxns
anaphylatoxins
cytokines
neuropeptides
leukocytes-deprived histamine -releasing peptide
histamine rxn lasts less than 30 mins (immediate transient reaction)
serotonin: vasodilatory effects similar to histamine
found in platelet granules
release triggered by platelet aggrevation and platelet activating factor
mediator systems — plasma protein systems
clotting:
hemostasis - vasoconstriction & plug (loose clot) formation
vasoconstriction
platelet activation: multiple factors, positive feedback
aggregation
loose clot

coagulation and clot formation - clotting cascade
2 pathways:
intrinsic pathway: contact activation pathway
extrinsic pathway: tissue factor pathway
both pathways join the common pathway where they convert Factor 10 → Active factor 10 which converts Prothrombin → Thrombin , Fibrinogen uses thrombin → fibrin → cross-linked fibrin that is important in stablizing blood clots

plasma protein system
clotting system
kinin system
fibrinolytic system
complement system
kinin system
hageman factor (in both clotting and kinin systems) lead to the production of Bradykinin
Bradykinin is important for increasing vessle permeability, vasodilation, pain (directly stimulate pain receptors), short lasting (30mins)
fibrinolytic system
dissolves the clot
bleeding stops
vessel repaired
endothelial tissue and platelet acts on plasminogen to make plasmin, thrombin from kinin system also indirectly act on plsminogen to make plasmin
plasmin: cut the fibrin into fragments → dissolves blood clots
complement systems
assists antibody in killing bacteria
3 pathways:
classical pathway: triggered by antibodies or C-reactive protein (made in liver) → bind to foreign cell membrane and kill them
C1 binds to C-reactive protein → split into C2 and C4 → split into C2a C2b and C4a C4b → C2b + C4b = C2bC4b aka C3 convertase → C3 split into C3a and C3b → C3b IS THE ACTIVE ELEMENT
alternative: triggered by C3b binding to bacterial cell wall
does not require C1,C2,C4 or specific antibody → more important than classical and lectin pathways in initial defense
factor B + C3b = C3bB → Factor D split Factor B into Ba (leaves) and Bb = C3bBb (unstable/short-lived) → Factor P + C3bBb = C3bBbP (stabilizes c3 convertase) →
lectin: main functional cell is Mannose that has structure and function very similar to C1 but gets recognized by lectin → C4bC2b = C3 convertase → C4bC2bC3b aka C5 convertase split into C5a and C5b
all pathways goes thru C3 convertase step to make C3a + C3b
arachidonic acid (AA)
product of membrane phospholipid
cyclooxygenase pathway act on AA → PGW PGD PGF PGI (vasodilation)
lipoxygenase pathway act on AA → leukotrienes → LTA → LTB (chemotaxis) or LTC → LTC → LTD → LTE (bronchospasm/bronchoconstriction — vascular permeability , vasoconstriction)
C3a, C4a, C5a main characteristic / fucntion
they are all anaphylatoxin, main job is to trigger mast cell degranulation and increase vascular permeability
how does the different systems of mediators connect to each other?
The Kallikrein in Kinin cascade can trigger plasmin production in fibrinolytic system and boost activity
The plasmin in fibrinolytic system cuts fibrin from the clotting cascade and can also act on C3 and C5 in complement cascade and boost activity
What is the role of NSAIDS (aspirin medicine)
it blocks the cyclooxygenase pathway and prevent the production of prostroglandins → prevent vasodilation
what is role of corticosteroids X (steroid medicine) ?
it blocks the phospholipases → prevents arachidonic acids production → no vasodilation or vasoconstriction → alleviate inflammation symptoms
cytokines and chemokines
protein cell product that act as a message to other cells, tell them how to behave
released by many cell types
IL1, TNF, IL6 activate endothelium and allow leukocyte recruitment
IFN-y activates macrophages/neutrophils, boosting killing ability
IL8 (chemokine) potent chemotactic factor for neutrophils
IL6 (cytokine) acts on hepatocytes to increase fibrinogen production → promotes clot formation

inflammation and resolution
immediate transient rxn: neutrophil recruited → phagocytosis → apoptosis , leaky vessels → edema
monocytes migrate into the tissues → become macrophage → clear out dead neutrophils
macrophage physically changes from M1 (pro-inflammatory) into M2 (pro-resolving) → tissue repair & regeneration (healing)
inflammation outcome
acute inflammation → healing with or without scars (fibrosis)
acute inflammation → pus formation (abscess)→ healing with scars (fibrosis)
acute inflammation → chronic inflammation (worsen/persistent injury) → healing with scars (fibrosis)
chronic inflammation
prolonged process (wks-months-yrs) in which 3 processes are occuring SIMULTANEOUSLY:
active inflammation
tissue destruction by inflammatory cells
tissue healing (repair & fibrosis): attemps at repair, neovasculation
granulomatous inflammation
special case of chronic inflammation
characterized by granulomas — organized collection of macrophages
not preceded by acute, neutrophil-mediated inflammation
circumscribed lesion, often nodular and surrounded by collagen fibers
not a tumor
pathology of inflammation
serous inflammation
watery, protein-poor effusion, excess alveolar fluid
fibrinous inflammation
fibrin accumulation
indicative of severe inflammation
seen in many bacterial infections
purulent inflammation
pus forming bacteria
pus is rich in dead and dying neutrophils, lytic enzymes, fibrin
localized collection of pus = abscess
ulcerative inflammation
necrotic and eroded eopthelial surface
commonly affects stomach or intestines
defined as a defect in the epithelium but may extend into deeper connective tissue
pseudomembranous inflammation
ulcerative inflammation + fibrinopurlent exudation = pseudomembranous inflammation
fibrin + pus + cellular debris + mucus form a pseudomembrane over an ulcer
fever
IL1,TNF and IL6 are regulated by cyclooxygenase which convert AA to prostaglandin → vasoDILATION
NSAIDS blocks cyclooxygenase → blocks prostagandin production → blocks vasoDILATION → reduce blood flow → REDUCE FEVER
leukocytosis
elevated WBC count
bacterial infection
parasitic infection
viral infection
increased erythrocyte sedimentation rate
test performed w anticoagulated blood in upright tube
sedimentation rate is reported in mm/h
during inflammation, fibrinogen is high and causes RBC to stick to each other (rouleaux) and sedimen faster
age and sex can effect sedimentation rate
tissue regeneration
involves restitution of tissue identitcal to that lost of by injury
healing: fibroproliferative response that patches a tissue defect by laying down connective tissue → fibrosis and scar formation
the sequence of healing
inflammatory response to eliminate the initial stimulus and initiate ECM deposition
proliferation & migration of parenchy al and connective tissue cells
formation of granulation tissue
synthesis of ECM proteins
tissue remodeling
wound contraction and development of wound strength
granulation tissue
consist of fibroblasts and vascular endothelial cells proliferation in the loose matrix
appear pink, soft and granular
ECM looks edematous b/c new vessels are leaky allowing protein and RBC escape
new blood vessels regress after 1-2 wks, the site will appear less red
weeks to months after, fibroblasts will secrete enxymes to breakdown collagen 3 and secrete collagen 1
eventually, repairedarea will have 70-80% of its initial strength
cells involved in proliferation and repair
labile cells
stable cells
permanent cells
labile cells
continuouslt dividng/mitotic cells
stem cells found in basal layer of skin, mucosa of internal organs, and limbus surrounding the cornea
cell divisiion occurs at a regular rate and differentiated daughter cells replace shed superficial cells
takes part in tissue regeneration post-injury
stable cells
quescent , facultative mitotic cells
don’t normally divide, can stimulate to divide
takes part in tissue regeneration post-injury
ex: liver regeneration after partial hepatectomy
permanent cells
nondividing, postmitotic cells
never divide
if injured, will be repaired by fibrosis scarring
does not regenerate
ex: neuron cells
clinical wound healing
first intention/primary healing
secondary intention/secondary healing
first intention/primary healing
little tissue loss
minimal scarring occurs
wounds can be closed w sutures
secondary intention/secondary healing
healing of large wounds where sutures is impossible
debris removal performed daily to encourage wound closure and allow granulation tissue formation
myifibroblasts help bring wound edges together
granulation results in a BROAD scar