PEDIATRICS FINAL NEW CONTENT
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
What are the signs and symptoms of physical abuse?
#1 sign is that the history does not match the injury!
Inconsistent story
Distance from parent
Does not protect physical exam
Apathy
Aggressive behavior
Attention Seeking
Cuts, bruises, fractures in various stages of healing
Infected wounds
Spiral fractures, facial trauma/fractures
Infants with fractures
Burns
Bruises (non-accidental sites: back, butt, groin, thighs, backs of knees)
What are the signs and symptoms of cultural practices that can be mistaken as physical abuse?
Cupping
Coining (lines going down diagonally with spine)
Mongolian Spots
Why are infants and toddlers at greater risk for complications from respiratory illnesses?
Smaller trachea diameter
Infant=4mm (1mm edema=50%diameter reduction)
Adult=10mm (1mm edema=20%diameter reduction)
Anatomy of the ribs
Fewer Alveoli @ Birth
Children: 20m/Adults: 300m
Increased Metabolic Demand
Increased RR: Neonates 40-50, Infants 20-40, 5y/o 15-25
Increase Oxygen Consumption
Neonates 6-8mL/kg/min
Adults 3-4mL/kg/min
Locate and identify the anatomical locations for the respiratory and cardiac conditions covered in class.
Condition | Primary Anatomical Location |
|---|---|
Epiglottitis | Epiglottis (above larynx) |
Croup | Larynx, trachea, bronchi |
Pharyngitis | Pharynx |
Tonsillitis | Palatine tonsils |
Otitis media | Middle ear |
Bronchiolitis | Bronchioles |
Cystic Fibrosis | Lungs, pancreas, GI tract |
Asthma | Bronchi and bronchioles |
Condition | Primary Anatomical Location |
|---|---|
Murmurs | Heart valves |
ASD (Atrial Septal Defect) | Interatrial septum |
VSD (Ventricular Septal Defect) | Interventricular septum |
PDA (Patent Ductus Arteriosus) | Ductus arteriosus (pulmonary artery → aorta) |
Pulmonary Stenosis | Pulmonary valve/outflow tract |
Aortic Stenosis | Aortic valve/outflow tract |
Kawasaki Disease | Coronary arteries |

What are the common s/sx. of laryngotracheobronchitis (CROUP) and how is it best managed?
Hoarseness
Inspiratory Stridor
Croupy/Barky
LTB
Management:
Viral (commonly seen in 6 months-4 years) - Cool mist humidifier, wrap in blanket and take outside, steamy bathroom
Bacterial (whooping cough) - make sure children get vaccinated DTaP (2/4/6/15-18/4-6years)
Severe Croup/w Stridor - EMERGENCY treat in ER with epi, corticosteroids, and albuterol
What are common observations when assessing an infant, toddler’s, preschooler’s, school-ager’s, adolescent’s respiratory patterns.
Retractions
Grunting - expiratory sound (usually suggests pulmonary edema)
Nasal Flaring
Wheezing - expiratory sound (#1 cause asthma, then bronchiolitis, bronchitis)
Stridor - high pitched crowing on inspiration (medical emergency, epiglottitis)
Cyanosis - bluish color
Clubbing -
Apnea - cessation of breathing for 20 seconds or more
What are the priority interventions (what order) when you find a child in respiratory distress with increased work of breathing (WOB)?
1st - reposition the child > 30 degrees (higher and supine)
2nd - check oxygen placement
3rd - bulb suction or Mushroom suction the nose
4th - then slowly adjust oxygen (infants ⅛ L, ¼ L, ½ L, ¾ L)
Other interventions
Elevate the HOB
Supine position
Increase the frequency of RT treatments
Promote rest - stop over stimulation, organize cares
Prevent the spread of infection (nosocomial), contact / droplet precautions if necessary
Which age groups of children and with which conditions/disease processes are at greatest risk for respiratory compromise?
Infections spread easily from one system to another
Most commonly viral
Highest incidence is 3 months - 6 years
We seldom see it in children younger than 3 months due to maternal antibodies
The most serious respiratory infections occur in children < 3 years
Children are often more ill than they appear
Croup → common 6 months - 4 years
How is epiglottitis identified?
Acute inflammation of the supraglottic structures and the epiglottis
The epiglottis is the flap of tissue at the base of the tongue that prevents food from going into the trachea
True pediatric emergency!!
What assessment findings will be noted for epiglottitis?
Sudden onset of respiratory distress → over a few hours the status worsens!!
Tripod sitting position, stridor, high fever, hoarseness, agitated, and refusing to lay down
Drooling
What are the interventions for epiglottitis?
DO NOT VISUALIZE THE UPPER AIRWAY!!!
This can cause the epiglottis to spasm which can lead to it worsening and can potentially close off their airway
Continuous monitoring - stay with the child
Elevate the HOB
Continuous O2 sat
Prepare to intubate
Diagnosis
Clinical signs
Sometimes we don’t have time to get an x-ray. We can tell just by the clinical signs that they likely have epiglottitis (tripod positioning, open mouth, drooling, etc…)
Lateral neck x-ray
Will show a large rounded soft mass at the base of the tongue
What is the pathophysiology for bacterial pharyngitis?
90% of sore throats and fevers in children are due to a virus and not bacteria
Viral pharyngitis:
Hand, foot, and mouth disease (Coxsackie virus)
Spread by droplet
At daycares, we sterilize diaper areas because it can be spread by stool for 8 weeks
We need to keep these babies hydrated
Pharygoconjunctival fever
Bacterial pharyngitis:
10% of children with a sore throat and a fever have a Group A Streptococcal Infection
What is the diagnosis for bacterial pharyngitis?
Rapid antigen tests – very specific, but sensitivity is only 85–90%
Positive (+) result = strep
Negative (-) result → we need to send a culture to the lab (48 hr return)
What are the assessment findings for bacterial pharyngitis?
Assessment Findings:
Sudden sore throat
Fever
Headache
Anterior cervical nodes
Petechiae on the palate
Beefy-red uvula
Tonsillar exudate
If Left Untreated Can Develop into:
Acute Rheumatic Fever
Carditis – inflammation of the heart
Polyarthritis – inflammation of many arteries?
Chorea
Bright red rash of the trunk and extremities
Post Streptococcal Glomerulonephritis
Complications of bacterial pharyngitis
Scarlet Fever
The rash is called “macular papular” → that is what you would document if there was a rash that feels like sandpaper.
PANDAS
controversial but possible (essentially strep caused OCD / tics)
Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS)
Following a strep infection (untreated) is the development of childhood OCD and / or tics
What is the treatment for bacterial pharyngitis?
10 day course of amoxicillin BID
Carrier State: 10 day course of clindamycin BID
Surgery
Tonsillectomy and Adenoidectomy (surgical removal of the tonsils + adenoid glands)
Most common indication is for an obstructed breathing pattern at night
Most children with mouth breathing will eventually develop dental malocclusion
Maxilla narrows due to the unopposed tongue – called adenoidal facies
Tonsil Grading
0 – surgically removed tonsils
1 – tonsils hidden within tonsil pillars
2 – tonsils extending to the pillars
3 – tonsils are beyond the pillars
Starting to intervene at 3 and 4
4 – tonsils extended to the midline
4+ – kissing tonsils (touching)
What is the pathophysiology for cystic fibrosis?
Autosomal recessive genetic condition
If there is a history of CF in an immediate family member, it would be wise to get genetic testing and have the partner get genetic testing as well
CF gene was identified in 1989 and is located on the long arm of chromosome 7 along with its protein product cystic fibrosis transmembrane regulator (CFTR)
Almost 300 alterations that diverge from the original sequence has been reported
The delta ΔF508 gene is the most common alteration (~ 70%) and most deadly
90% of those homozygous for delta ΔF508 have pancreatic insufficiency, whereas only 36% of CF patients with other mutations have pancreatic insufficiency
The gene seems to lead to both pancreatic deficiency and pulmonary disease
Since the CFTR is defective, there is an abnormal electrolyte and fluid transport across epithelial cell membranes by mechanisms not well understood
This alteration explains the thickened mucous and secretions of the pulmonary, GI, and reproductive systems
Also explains the abnormality in the sweat glands, accounting for the elevated NaCl levels from the blocked transport
What is the diagnosis for cystic fibrosis?
1000 infants are diagnosed per year
Screen newborns
Sweat Chloride > 60 mEq NaCl is diagnostic
Gauze pads soaked with pilocarpine is placed on the forearm and small, electric current stimulates sweat glands
Future Tests:
Fecal Fat Test – look for digestive enzymes
Followed by Pulmonary Function Tests
%FEV1 don’t need to memorize – maria
75% mild disease
50–74% moderate disease
25–49% moderate to severe disease
< 25% very severe disease
40% is when we put the patient on the lung transplant list. Even if they have a lung transplant, they will still have CF
Sputum + CF
1. Staphylococcus Aureus
Staph infections are very common in young children
2. Pseudomonas Aeruginosa
gram negative bacteria – rod appearance
This is what turns the mucus green
3. Burkholderia Cepacia
Grows on potatoes and onions (the bacteria is present when those rot)
If we smell rotten potatoes or onions, that is Burkholderia Cepacia
If they have this, they will not be put on the transplant list because it could be hiding in their body
What are the assessment findings for cystic fibrosis?
Respiratory
Wheezing
Dyspnea
Mucousy cough
It will be turning green - that’s bacteria
Cyanosis
Clubbing
Lack of oxygen causing inflammation in the small capillaries
Chronic sinus problems
Polyps in the sinus cavity - they look like grapes in the nose and they need to be removed frequently.
The anterior posterior ratio usually increases with kids with CF because they are retaining air
GI
Meconium ileus at birth (unable to pass first poop)
Rectal prolapse (#1 GI sign)
Infants are pushing really hard
Loose, bulky, frothy, foul smelling stools
Frothy and bulky stools happen because they don’t have the pancreatic enzymes and they are passing out fat through their stool
Then they can’t gain weight because they are losing all of the stool
Increased appetite
They will start out with this because they are losing so many calories
Increased weight loss
As mucous production gets worse, they won’t want to eat (and lose more weight)
Vitamins A, D, E, K (fat soluble) are lost
A = eyes are affected
D = bones are affected
E = immunity
K = bleeding issues
ABDEK or AquADECK (B vitamins added to fat soluble)
Cardiac
Cor Pulmonale (right sided HF due to obstruction of the pulmonary blood flow)
Anytime you have a chronic respiratory issue, we will see right sided heart failure
Kids with CF should have a chest vest to help shake up the mucous
Reproductive
Males → 98-99% chance of blocking the vas deferens
Females → higher percentage of infertility
Increased viscosity of cervical mucous (blocks entry of sperm)
What is the treatment for cystic fibrosis?
Huffing and coughing (huff coughing)
Autogenic Drainage
Uses different speeds of breathing to move mucus from small airways to medium to large airways
BPD – bronchial postural drainage
CPT – chest percussion treatments (the vest)
Rattling 2–3x / day for about 20–30 mins
Antibiotics
Flutter Valve
A little “ball” inside the nebulizer that creates a vibration → helps break up the mucus down in the lungs
PEEP
Pancrelipase (pancrease) capsules – with all meals and snacks
ABDECK Vitamins daily
ADEK – fat soluble?
BC – water soluble?
Ibuprofen in very high doses
Above the 5–10 mg/kg/dose
Anti-inflammatory → helps lower the inflammation in the lungs
Ranitidine (Zantac)
Helps decrease gastric mucosa and resolve those GERD like s/sx
Pulmonary Function tests to monitor status
We are watching this to make sure it is not getting too low
< 40% → looking at getting a lung transplant at this point
Diet – 130% RDA
New Drugs
Ivacaftor (Kalydeco) by mouth – 1st line (approved in 2013)
Treats G551D mutation (4–5% → about 1,200 people in the US)
Patient Cost = $236,000 ($450 per tablet)
Elexacaftor / tezacaftor / ivacaftor (trikafta) by mouth (approved 2019)
2 years old with at least 1 ΔF508 deletion / mutation
Ivacaftor – chloride channel opener
Elexaftor / Tezacaftor – are CFTR modulators
Repairs delta ΔF508 deletion / mutations
Results in:
Increased transport of Cl and Na ions (correcting fluid shifts) and thins mucus secretions
↓ pulmonary exacerbations → 63% lower
Seen a drop in hospitalizations for children with CF
Sweat Chloride – 41 mEq lower
What is the pathophysiology of asthma?
Pathophysiology
Reversible airway inflammation and increased airway responsiveness to a stimuli
Airways are for some reason hyper–responsive to a precipitant or trigger
Condition is manifested by exaggerated bronchoconstriction of the airways
Mast cells in the airways release histamine, which causes smooth muscle contraction + bronchoconstriction. Goblet cells will hypersecrete mucous and there is epithelial damage that leads to ↑ permeability + sensitivity to inhaled allergens and irritants
End Result of Asthma:
Airway edema
Mucous plugging
Significant airway narrowing
Leading to rapid airway obstruction
What are common triggers for Asthma?
Triggers: be able to identify common triggers
Smoke
Strong Emotions
Furry Pets, dust (can get stuck in carpet → hard flat floors are better), pollen, etc.
House dust mites
Molds
Changes in the weather (ex: I have cold induced asthma)
Colds + Viruses → inflammation
Exercises → spasms in the lungs
Cockroaches
An insect that turns into dust shortly after death → irritating on the lungs
More common in warm, wet environments
Strong Smells → typically adults are more sensitive compared to children
Atopic March (Asthma)
Atopic Derm - Allergic Rhinitis - Asthma
Asthma + Pediatrics
Infancy – Atopic Dermatitis / Eczema (1 in 10 children)
Reactive Airway Disease → considered the precursor to asthma
Eczema → open skin + bleeding → introduces many different potential asthma triggers
Atopic March
symptoms early in childhood (before the child even has asthma) to assess the risk of the child developing asthma
Stresses the importance of skin barriers like petroleum jelly (vaseline) in the prevention of atopy and future development of asthma
Wet-Wraps
Dampen the skin first
then apply a thick coat of vaseline + wrap with cotton
Steroid Creams
Good for decreasing inflammation, but thins the skin after long periods of time. Use only for 1 week and then take a break. NOT preferred.
Skin Microbiome
Research shows: roseomonas mucosa bacterial skin sprays (OTC) have live probiotics that you spray on the skin → improves dermatitis / eczema symptoms
Toddler-Preschool – Allergic Rhinitis
The kid who is always witing their nose
aka the “Allergic Salute” – a dent in the nose from wiping so often
School-Age and Adulthood – Asthma
What are the common cardiac inspections?
Nutritional status
Look at their chest + evaluate if they are taking in enough calories
Assess Skin (color, mottling, cyanosis in mucous membranes)
Mottling in a child: marble appearance of the skin (blotches of red and white in the centers)
Mottling is common + expected in the first week of life (prolonged mottling could be a potential concern)
Excessive perspiration
Mild sweating on the brows + lips
Chest Deformities
Pectus Excavatum (Caving in)
Needs to be monitored by a cardiologist to ensure that the heart has enough space to grow and function appropriately
If not the child may need surgery (open heart) to cut open, detach all of the ribs, and then require the whole chest to pop out
This surgery would be done AFTER puberty (ex: a male in his early 20s) and will need good pain management
Pectus Carinatum (Coming out)
Typically caused by open heart surgery as a child, etc.
There is more space for the heart, but usually indicates some sort of cardiac issue
Retractions
Clubbing
Edema
What are the common cardiac palpations?
PMI – point of maximum index (i think)
< than 7 y/o → @ the 4th ICS (intercostal space)
> than 7 y/o → @ the 5th ICS (intercostal space)
Feel the PMI at the nipple spot
If lower, document at the 5th or 6th ICS
All we should be feeling is the PMI – your hand should NOT be moving
Obviously not ideal findings:
Lifts → beating that feels like it’s lifting / moving your hand of the heart
Heaves → feels like an up and over motion
Thrills → like a cat purr / vibration
Hepatosplenomegaly → can you feel the spleen under the rib cage?
Check for peripheral pulses
Femoral + brachial
What are the common cardiac auscultation locations?
Heart rate and rhythm (listen for 1 full minute, under clothing)
Listen APETM
Components of the cardiac cycle
S1 – Mitral and Tricuspid Closure
Coming from the lower portion of the heart
Heard better with the diaphragm of the stethoscope
S2 – Aortic and Pulmonic Closure
Coming from the upper portion of the heart
Heard better with the bell of the stethoscope
Systole occurs between the S1 and S2
Diasole occurs opposite the pulse
S3
Normal in children with thin chest walls
Abnormal if > age 30 (indicate hyperdynamic circulation)
Sloshing In → sounds like: Slosh (S1) - - ing (S2) - - - in (S3)
Or Kentucky
S4
Almost always abnormal
A stiff wall → sounds like: A (S4) - - Stiff (S1) - - - Wall (S2)
Or tennessee
How would you describe an innocent murmur, how can this be assessed? Should you mention to the parent?
Innocent murmur
Consider how and when to mention to the parents
Psych-social assessment of parent’s readiness
Are you 100% confident it is an innocent murmur?
Still’s Murmur
Most common innocent murmur
Soft, low pitched (typically a grade II/VI)
Early to midsystolic and musical or vibratory (not just a crisp lub-dub)
Heard best at LLSB and the Apex, when the child is supine
PMI (which is at the 4th ICS in children)
LLSB = left lower sternal border
Listen APETM and then have them sit up and listen again
If the murmur becomes louder as the child sits up, there is an increase in the possibility it is no longer “innocent”
Now the heart is louder as it’s closer to the rib cage → concerning
Physical Exam Findings for Innocent Murmurs
Grade I–II / VI
Systolic in timing (except for venous hum)
Musical or vibratory
Duration is short (early systolic)
LLSB or pulmonic areas
Normal Gestation and Delivery
Normal S1 and S2
For the congenital cardiac defects covered in class, where are the anatomical defects located? What does this do to blood flow?
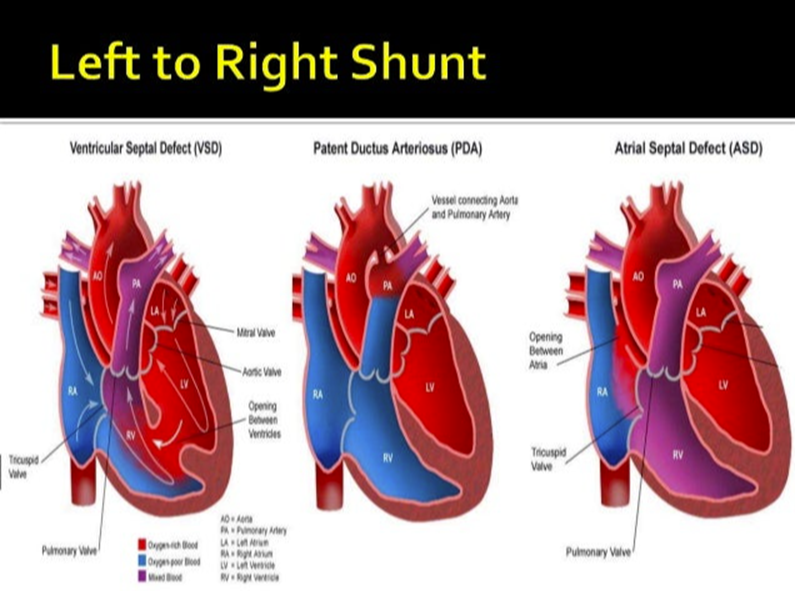
ASD Atrial Septal Defect - hole in septal wall between L & R atria/increased pulmonary flow
VSD Ventricular Septal Defect - hole in septal wall between L & R ventricles/increased pulmonary flow
PDA Patent Ductus Arteriosus - left to right shunt until birth (normally closes 24-48 hrs after birth) instead of the blood going to the lungs, can go to aorta for circulation
Left to Right Shunts
Left to Right Shunts: Acyanotic Congenital Heart Diseases
Left-to-right shunts → the pressure pushes blood over to the right side of the heart from the left
With acyanotic congenital heart diseases, blood goes from the high pressure of the left side to decreased pressure of the right side, which sends more blood to the lung → leading to overwhelming of the lungs.
We will hear wet lungs, tachypnea, sweating while eating, CHF, etc…
Atrial Septal Defect (ASD) - Involves Foramen Ovale
Left-to-right shunt
Makes up 10% of those with CHD
ASD is a murmur meeting:
Grade II-IV/VI
@ the second left intercostal space (LIS)
May radiate to the back
Will increase pulmonary blood flow + most will need surgery by 3-5 y/o
There is not enough pressure within the heart to close off the foramen ovale (after birth), so the blood that already got oxygenated at the lungs is just coming back and repeating the cycle – overwhelms the lungs
Pulmonary vascular changes occur after many years if there is no repair and can lead to an enlarged heart
ALWAYS listen to the top of the heart
APETM → the aortic and pulmonic site (top of the heart) is where we are able to identify murmurs and defects like this
Ventricular Septal Defect (VSD)
Makes up 20-25% of those with CHD (congenital heart diseases)
The size of the hole determines how much of in increase there is of blood flowing to the lungs
Murmur is heard @ LLSB and is grade II-IV/VI
The bigger the hole - the quieter the murmur
The smaller the hole - the louder the murmur
Higher pitched
You will see pulmonary edema!!
Patients with VSD are at risk for bacterial endocarditis
Patent Ductus Arteriosus (PDA) → Involves Ductus Arteriosus
Left-to-right shunt → blood is sent back to the lungs again
Pulmonary edema!!
CHF
Left atrial and ventricular hypertrophy!!
Sweating during feeds
Murmur is at the 2nd ICS, under the clavicle
Has a machinery type of sound (murmur), with split S2 bounding pulses (sounds like lub de dub).
Treatment
Indocin (indomethacin) - prostaglandin inhibitor
Constricts / closes the ductus
Education
What are also prostaglandin inhibitors? → NSAIDS
Educate expecting mothers to NOT take ibuprofen during pregnancy because if it is used, it may close the ductus arteriosus
Arteriosus of the fetus → unable for blood to shunt & is related to stillbirths
Coils in the cath lab will close the PDA
Obstructive Flow - Pulmonary Stenosis
Makes up about 8% of those with CHD
Loud murmur (grade III-IV/VI), @ the LUSB (left upper sternal border)
Radiates to the back with a thrill and split S2 sounds (lub-de-dub)
Results in right ventricular hypertrophy and decreased pulmonary blood flow
Obstructive Flow - Aortic Stenosis
Makes up about 5% of those with CHD
Murmur is grade II-IV/VI at the 2nd and 3rd ICS
Thrill is present + felt at the suprasternal notch
Will be able to actually feel the thrill if you place your hand on their chest (upper heart sounds → aortic and pulmonic sites)
Unless the condition is severe, it may not be picked up until adulthood
However, that realization may not get “picked up” early enough because it can also cause → Sudden Cardiac Death!!
Lynn had a friend who was in the Marines (clearly a fit guy) who passed out exercising + died → and the mother could only remember a past “sign” being him fainting in the pool one time or something when he was younger
So if we know that they have this condition, educate them to avoid sports → so we can avoid that sudden cardiac death :)
May also see:
poor pulses due to the stiff aorta → results in difficulty pushing blood out to the body
Becomes fatigue easier than what would be considered normal
CXR (chest x-ray) → cardiomegaly
Coarctation of the Aorta
Usually occurs near the ductus arteriosus
Left ventricular overload occurs resulting in ↓ BP and weakened pulses in the lower extremities
Males 2:1 (more prevalent in men)
Systolic ejection murmur is present at the left infraclavicular region, that transmits to the back – it is hard to tell where it is actually coming from
Good idea to get an ultrasound → helps visualize
Right to Left Shunts: Cyanotic Congenital Heart Disease
With right-to-left shunts, the blood is going right from the right side to the left side without ever going through the lungs. This causes deoxygenated blood to go to the rest of the body and we will see cyanosis in the baby
Tetralogy of Fallot (TOF)
Ventricular Septal Defect
There is no separation between the left and right ventricles (no separation between oxygenated and deoxygenated blood)
The defect is high up in the septum → so close to the aorta that the aorta will suck up both deoxygenated and oxygenated blood and push that out to the rest of the body (overriding aorta)
Pulmonary Stenosis
The most important part of TOF!!
Blood cannot get to the lungs easily (due to narrowing of the pulmonary artery), so blood takes an easier route.
The easier route is to go through the VSD into the left ventricle (the pressure on the right side is so high because of the narrowed pulmonary artery, so it pushes the blood to the left side)
Then, it will go from the left ventricle out the aorta to the rest of the body (deoxygenated blood going to the body due to not being able to go through the lungs)
Right Ventricular Hypertrophy
Blood is not able to exit easily to the lungs due to the pulmonary stenosis → this makes the right ventricle work harder to pump blood out, and this leads to an enlarged heart / hypertrophy
Overriding Aorta
The aorta sits directly over the ASD instead of the left ventricle
Basically the aorta is misplaced and “sucking” blood from both ventricles
Pulls oxygenated blood from the left side, but it also pulls deoxygenated blood from the right side
“Tet spells” (cyanosis around the fingers and mouth)
When the baby cries, feeds, or poops.
O2 demand increases → right to left shunting increases → MORE deoxygenated blood enters the aorta → the baby turns blue
Assessment finding
Harsh systolic murmur at LUSB
Thrill present
Loud S2 → not split because of the decreased pulmonary blood flow
What are the interventions for a child who is having cyanosis, and why does this work?
When a baby is cyanotic, have them squat!!!
Squatting in a knee-chest position helps re-oxygenate the child because that position compresses the body and stops blood flow to the feet and arms (shunting blood to brain and organs) → increased perfusion!!
This is why we tell people to sit down and put their head between their legs when they faint or feel unwell
What is the pathophysiology/etiology for Kawasaki’s Disease?
First described in 1967 as a mucocutaneous lymph node syndrome
It is an acute, self-limiting multiple organ system disease of childhood resulting in severe inflammation of blood vessels (coronary arteries)
Importance related to the fact 20% of those will develop coronary artery abnormalities
Aneurysms are a big concern because if the coronary arteries get too inflamed, it could cause the vessels to burst which could cause death
Etiology:
Majority of children of Japanese Heritage
African American → intermediate risk
Caucasians → lowest risk (but actually more at risk in WI)
Residence near a large body of water
Non-contagious
< 5 years old
Higher Incidence in the Winter to Spring
Many respiratory illnesses are going around during this time
Bellin sees about 2–5 cases / year
5% of those with Kawasaki’s Disease die
What is the diagnosis for Kawasaki’s Disease?
On clinical grounds only – there are NO blood / lab tests
Assessment findings are our only clue
5% death rate with this, which is concerning :(
Fever for 5 days
Dry, cracked lips
Conjunctivitis
Strawberry tongue, red oral mucosa (papilla are raised)
Edema of hands + feet
Very puffed out → so much it starts to pull the skin away from the nails
Pelling of fingertips and toes – “classic sign” -Lynn
Reddening of the palms and soles of the feet
Swelling of cervical lymph nodes
Patchy rash
What is the treatment for Kawasaki’s Disease?
Intravenous Immune Globulin (IVIG) → x 2 doses
Helps prevent an increase in the size of the coronary arteries of the heart
High Dose Aspirin (high dose while hospitalized) → then lowered to a therapeutic range (TR) for 2 months of home use
Anti-inflammatory effects in acute phase (bc aspirin is a NSAID)
Anti-platelet effects in recovery to prevent blood clots / thrombosis
There is a mandatory report to the County Health Department to track the incidence