Lecture 146: Immunogenetics, Lymphocyte Activation, Immune Regulation Tolerance II
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
Immunological synapse
region of contact between APC and T cell including redistributed proteins
- causes early events such as tyrosine phosphorylation of molecules of TCR complex + recruitment of adapter proteins to site of T cell antigen recognition - TF activation
Clonal expansion
within 1 or 2 days after activation - T lymphocytes proliferate - expansion of antigen specific clones
- this helps the adaptive immune response to keep up with rapidly dividing microbes
Differentiation of Naive T cells to Effector Cells
CD4 cells differentiate into effector cells - respond to antigens on surface molecules - activate phagocytes + B lymphocytes - produce Th1 and Th 2 cells
Differentiation of CD4 native cell types
Development of Memory T lymphocytes
some T cells differentiate to memory cells that survive after infection is gone
- Location: lymphoid organs, mucosal tissues
Central memory cells: in lymphoid organs: responsible for rapid clonal expansion after exposure to antigen
Immunological ignorance
antigen specific unresponsiveness: being able to recognize self antigens but not respond to it
- if this fails: autoimmunity
Central tolerance
T cells: cell death
CD4 cells: generation of T reg cells
Negative selection: destroy lymphocyte that binds too strongly to MHC or binds to self antigen (triggers apoptosis)
- doesn't complete maturation
Main processes in Central tolerance
Peripheral tolerance
Peripheral tolerance is induced
= when mature T cells recognize self antigens in peripheral tissues, leading to functional inactivation (anergy) or death,
or when the self-reactive lymphocytes are suppressed by regulatory T cells
Positive selection
- takes place in cortex of thymus
- cortical epithelial cells, which express MHC class I & II molecules bind T cells, which have receptors for our own MHC molecules
- -cell receptor that binds to a self-MHC class I molecule on thymic cortical epithelial cells in the thymus, are signaled to survive
- no binding to MHC I: die
Negative selection
deletion of strongly self- reactive T cells in the thymus.
• T cells that have undergone positive selection then go
to the thymic medulla where they undergo negative
selection
Combinations of positive and negative selection
How are anergy and CTLA4 forms of tolerance?
Anergy: inactivation of T cells when not enough co stimulation is present for full T cell activation
CTLA4: can bind to B7 shutting off T cell response
- interferes with binding of CD28/B7
Immune suppression by Regulatory T cells
develop in the thymus or peripheral tissues upon recognition of self antigens
- they block the activation of potentially harmful lymphocytes specific for these self antigens.
• Most regulatory T cells are CD4+ and express high levels of CD25
Function of FOXP3
- binds to specific regions of DNA
important in activating Treg - inhibits T cell activation and effector functions
Activation Induced Cell Death
Self antigen recognition - apoptosis
- Death receptors + Fas and Fas ligand leads to apoptosis
What influences between t cell tolerance and activation?
Central B vs Peripheral B cell tolerance
Central: Receptor editing (expression of new receptor) or apoptosis (negative selection)
Peripheral:
- A mature B cell that recognizes a self antigen without T cell help is functionally inactivated and becomes incapable of responding to that antigen.
Mature B cells that are partially activated by recognition of self antigens without T cell help may die by apoptosis
Immune responses against Transplants
What is the principal targets of rejection?
Antigens of allografts which are proteins encoded in MHC complex
- recognition of MHC antigens on another individual's cells is one of the strongest immune responses
Indirect vs direct recognition
Indirect:
- T cell recognizes processed peptide of allogenic MHC molecule bound to self MHC molecule on host APC
Direct:
- T cell recognizes unprocessed allogenic MHC molecule on graft APC
Acute transplant rejection
several days or weeks after transplantion
- principal cause of graft failure
- mediated by CD8 cells against allo antigens in graft
Cause of acute transplant rejection
direct pathways of allorecognition that involves activation of recipient T cells by dendritic cells from donor
Hyperacute rejection
occurs within minutes
- thrombosis of graft vessels and ischemic necrosis of graft
- mediated by circulating antibodies, specific for antigens on graft cells - present in recipient before transplantation
- antibodies are specific for blood group antigens or abs specific for allogenic MHC molecules
How do you minimize hyperacute rejection?
cross match testing
Test donor WBCs against recipient serum
If recipient has pre-formed antibodies → cell lysis
Negative crossmatch = safe to proceed
Chronic Rejection
months to years
- progressive loss of graft function
- To prevent: give immunosuppressant drugs
- fibrosis of graft tissue and bv
Graft vs host transplant rejection
common with bone marrow transplant and liver transplant
grafted immunocompetent T cell proliferate in host and reject cells with foreign proteins
jaundice, hepatosplenomegaly, diarrhea, maculopapular rash
Tumor cell killing by T cells
A 50 year old male with chronic renal failurehad a cadaveric renal transplant that was successful asdetermined by the production of urine during thesurgery. Two weeks later, his creatinine level began torise and urine production decreased. UA was normal. Abiopsy was taken from the kidney which revealed aninfiltrate.
Which of the following would most likely be found on the surface of the cells responsible for his condition?
a) CD 20
b) CD 27
c) CD 4
d) CD 8
e) CD 9
D
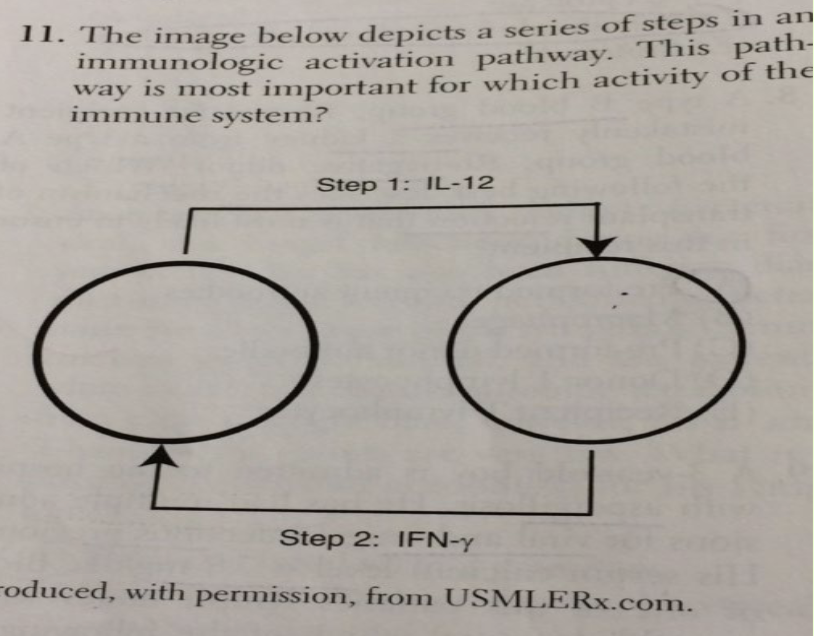
A) Antigen presentation and destruction of intracellular pathogens
B) Defense against parasites and other pathogens by eosinophils
C) Immediate allergic hypersensitivity reaction involving IgE
D) Neutrophil chemotaxis
E) Antibody secretion by plasma cells
A
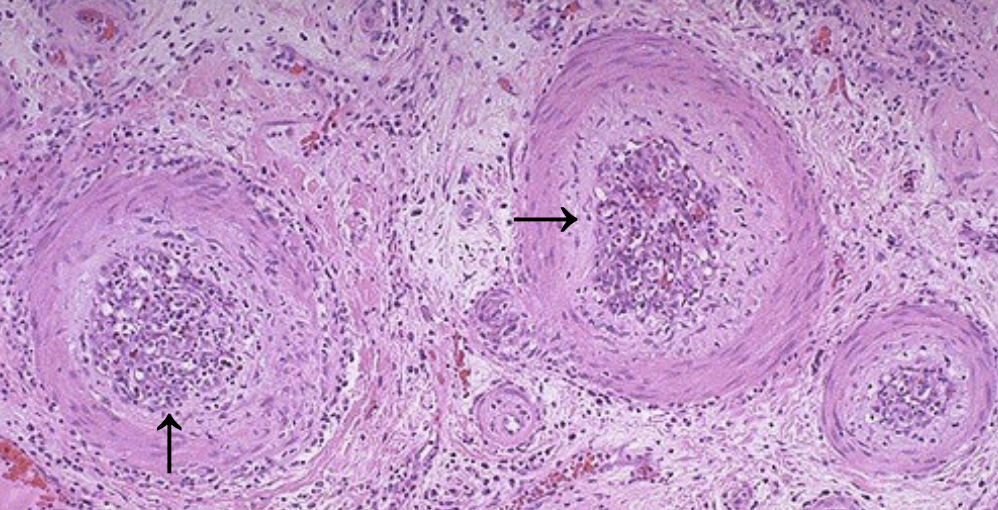
A 48-year-old female with late stage chronic renal failure from diabetes undergoes renal transplantation. Urine production is adequate post- operatively. 8 months later for a follow-up visit, she has a BUN/Cre level well above normal and complains of decreased urine production with symptoms of headache and back pain. A biopsy reveals what is shown on the next slide. What is the pathogenesis of this condition?
A. Damage due to infiltrating neutrophils & basophils
B. Damage due to infiltrating dendritic cells
C. Damage due to infiltrating T cells & macrophages
D. Damage due to binding of IgA + complement
C
Due to time passed since transplant
The role of CD3 proteins and the zeta chain on the surface of the cell is to:
a) transduce signals to the interior of the T cell
b) bind to antigen associated with MHC molecules
c) bind to MHC molecules on the APC
d) bind to CD4 or CD8 molecules
e) facilitate antigen processing of antigens that bind to the surface of T cells
A
Which of the following accurately completes this statement: “The function of ____ T cells is to make contact with ____ and ____”? (Select all that apply.)
a) CD8; virus-infected cells; kill virus-infected cells
b) CD8; B cells; stimulate B cells to differentiate into plasma cells
c) CD4; macrophages; enhance microbicidal powers of macrophages
d) CD4; B cells; stimulate B cells to differentiate into plasma cells
e) All of the above
A, C, D
Several years ago, the famous musician Bob Dylan developed a somewhat unusual fungal infection affecting his heart. This type of infection is typically associated with a certain defect of the immune system and is endemic in certain parts of the Midwest. What is the name of the fungal infection that caused his endocarditis, and the nature of the immune defect ?
A. Cryptococcosis; loss of Th2 function
B. Candidiasis; defect in neutrophil activation
C. Nocardiosis; apoptosis of activated macrophages
D. Histoplasmosis; impairment of Th1 function
E. Coccidiomycosis; failure of antigen processing by dendritic cells
D
B/c of location
Which of the following explains why dendritic cells are more efficient than macrophages at stimulating naive T cells?
a) Macrophages do not express MHC class II molecules
b) Dendritic cells are migratory and transport antigen to neighboring secondary lymphoid tissue.
c) Dendritic cells do not repair damaged tissues.
d) Macrophages process only polysaccharide antigens.
e) Dendritic cells, but not macrophages, endocytose foreign antigen
B
An adjuvant enhances the effectiveness of vaccines by inducing the expression of ____ on ____.
a) Co-stimulatory molecules; dendritic cells
b) CD28; macrophages
c) MHC class II molecules; T cells
d) T-cell receptor; T cells
e) Immuno-receptor tyrosine-based activation motifs; dendritic cells
A
Immune checkpoint blocking therapies (ICBTs) have been implemented in the clinic to treat a variety of malignancies based upon their ability to:
A. Activate memory T cells to stimulate B cells
B. Enhance antibody production & binding to C’
C. Target T-cell inhibitory molecules or receptors
D. Prevent apoptosis of cytotoxic CD8 T cells
E. Increase phagocytosis by neutrophils
C
Immunologic Synapse Formation Key Molecules
- Involves TCR, CD3, CD4/CD8
- Co-stimulatory molecules (CD28 on T cell ↔ B7 on APC)
- “SMAC” = Supramolecular Activation Complex
Antigen Recognition Key Molecules
- CD4 binds MHC II
- CD8 binds MHC I
- Trigger early signaling
Signal Transduction Key Molecules
- Tyrosine phosphorylation of CD3 ζ-chain
- Adaptor proteins like ZAP-70
- Activates transcription factors: NF-κB, NFAT, AP-1
Clonal Expansion Key Molecules
- Driven by IL-2 secretion and IL-2 receptor (CD25) expression
Differentiation Key Molecules
- CD4+ → Th1, Th2, Th17, Treg
- CD8+ → Cytotoxic T cells
Mnemonic: "Signal 1 = TCR; Signal 2 = CD28-B7; Signal 3 = Cytokines"
No Signal 2 → Anergy
IL-2 = "T-cell growth factor" (autocrine)
Allorecognition
Cause of acute rejection of transplanted tissues or organs, involves activation of recipient’s T cells by dendritic cells of donor origin