Nursing Science 2 exam 2 2025
1/229
Earn XP
Description and Tags
everything
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
230 Terms
Inheritance
The passage of hereditary traits from one generation to another.
Genetics
The branch of biology that deals with inheritance.
Genotype
The genetic makeup of an individual, represented by alleles (e.g., Pp).
Phenotype
The physical characteristics determined by the genotype and the environment (e.g., brown hair, blue eyes).
Mutation
A permanent, heritable change in a gene that causes it to have a different effect than it had previously.
Homozygous
An individual with the same alleles on homologous chromosomes (e.g., PP or pp).
Heterozygous
An individual with different alleles on homologous chromosomes (e.g., Pp).
Dominant allele
An allele that is always expressed, overriding the corresponding allele on the other homologous chromosome.
Recessive allele
An allele that is completely hidden or masked by the presence of a dominant allele and is expressed only when no dominant allele is present.
Punnett square
A method of showing the possible genetic combinations in offspring of two individuals.
Autosomes
Any chromosomes other than sex chromosomes; humans have 22 pairs of autosomes.
Sex chromosomes
The 23rd pair of chromosomes that determine an individual's sex; XX for females and XY for males.
Sex-linked traits
Traits determined by genes located on the sex chromosomes, often observed as X-linked traits.
Polygenic or Complex inheritance
Inheritance controlled by two or more genes, often influenced by environmental factors.
Teratogen
Any agent or influence that causes developmental defects in the embryo.
Cystic fibrosis
An autosomal recessive disease characterized by altered function of exocrine glands, particularly affecting the lungs and pancreas.
Down syndrome
A genetic disorder caused by trisomy of chromosome 21.
Environmental influences
Factors that affect phenotype, including nutrition, exposure to chemicals, and other environmental conditions.
Autosomal dominant genetic disorder
Conditions that manifest when at least one allele is dominant and can lead to disease without needing two copies.
X-linked traits
Genetic characteristics determined by genes located on the X chromosome, often affecting males more severely as they have no backup copy on the other x chromosome like females have.
Multiple allele inheritance
A form of inheritance where more than two alleles exist for a gene, leading to a variety of possible phenotypes among individuals. An example is blood groups.
Sex determination
Depending on whether the secondary oocyte is fertilised by a sperm containing a Y or X chromosome because all oocytes have an X. Sex is therefore determined by the father (sperm).
Ovaries
Glands in the female reproductive system that produce oestrogen, progesterone, and the secondary oocyte. Positioned laterally to the uterus by several ligaments.
The ovarian cortex contains follicles/oocytes, the ovarian medulla consists of connective tissue and blood/lymphatic vessels.
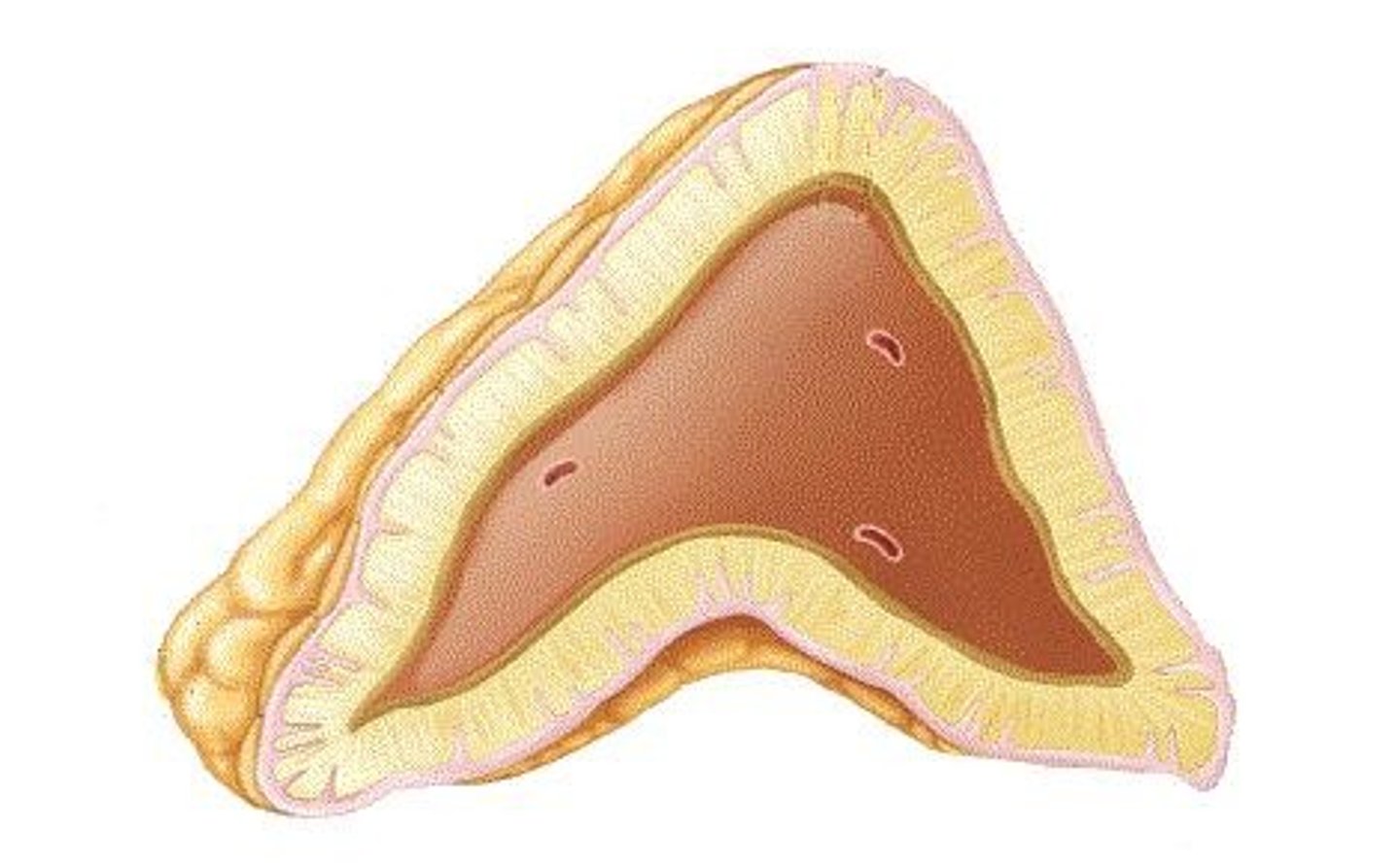
Uterine tubes (Fallopian tubes)
Tubes that transport the ovum from the ovaries to the uterus, where fertilization generally occurs. They have fimbrae and cilia that sweep the oocyte up from the abdominopelvic cavity inside. it has two sections - the ampulla where fertilisation occurs and the isthmus.
Menstrual cycle
The regular natural change that occurs in the female reproductive system, involving the preparation of the endometrium to receive and nourish a fertilized ovum.
Corpus luteum
A temporary endocrine structure formed from the follicle after ovulation, which secretes progesterone and some oestrogen.
Endometrium
The innermost functional layer of the uterus that is shed during menstruation and regenerates in preparation for a potential pregnancy.
Cervical mucus
Mucus produced by the cervical glands that changes in consistency throughout the menstrual cycle, aiding or impeding sperm passage.
Prolactin
A hormone involved in initiating and maintaining milk production in the mammary glands.
Ectopic pregnancy
A pregnancy that occurs outside the uterus, commonly in the fallopian tubes, often due to blocked tubes.
GnRH (Gonadotropin-releasing hormone)
A hormone secreted by the hypothalamus that stimulates the anterior pituitary gland to release FSH and LH.
FSH (Follicle Stimulating Hormone)
A hormone that stimulates the growth of ovarian follicles and the secretion of oestrogen.
LH (Luteinizing Hormone)
A hormone that triggers ovulation and the formation of the corpus luteum.
Graafian follicle
A mature ovarian follicle that is ready for ovulation, containing a secondary oocyte.
Menopause
The time in a woman's life when menstruation ceases completely, typically occurring between ages 46 to 64.
Mammary glands
Modified sweat glands that are responsible for the synthesis, secretion, and ejection of milk.
Vagina
A 10 cm long fibro-muscular canal extending from the cervix to the external body, serving multiple reproductive functions which are a receptacle for the penis, outlet for menstrual flow and a passage-way for childbirth
Myometrium
The middle layer of the uterus composed of smooth muscle that contracts during labor to expel the fetus.
Oestrogen
The primary female sex hormone, secreted by the ovaries, crucial for the thickening of the endometrium and female sexual characteristics.
What are the functions and effects of oestrogen?
endometrial thickening and development of glands
increases vascularisation of myometrium and endometrium
development of ducts in breasts and breast enlargement
maintains female secondary sex characteristics
increases protein anabolism including building strong bones
lowers total blood cholesterol level, protecting from cardiovascular disease
Progesterone
A hormone secreted by the corpus luteum that prepares the endometrium for potential pregnancy after ovulation.
Hormonal feedback loop
Process by which hormonal levels regulate the release of other hormones, ensuring balance in the reproductive cycle.
Phases of the female reproductive cycle
In order:
Menstrual phase, pre-ovulatory phase, ovulation, post-ovulatory phase
Menstrual Phase
What days and outline
days 1 to 5, where the uterine lining is shed and menstrual bleeding occurs. Low progesterone causes spiral arterioles to constrict so lack of blood supply causes functional layer endometrium to die. This detaches from the uterine wall and is shed.
Pre-ovulatory phase
Days and outline
days 6 to 13, where the endometrium begins to thicken in preparation for a potential pregnancy. Follicle-stimulating hormone (FSH) promotes the growth of ovarian follicles which secretes estrogen so levels rise. A dominant follicle matures into a mature follicle which bulges at the surface of the ovary. In the uterus this phase involves the regeneration of the endometrial lining, spiral arterioles grow back - called proliferative phase.
Ovulation
Days and outline
This phase occurs around day 14 of the cycle when a mature (Graafian) follicle releases a secondary oocyte into the abdominopelvic cavity. A surge in LH triggers this process, marking the transition to the next phase, and the egg is available for fertilization.
Signs of Ovulation
Increased basal body temperature, cervical mucus thins to allow sperm through - caused by increased oestrogen, cervix softens, discomfort/pain.
Following Ovulation
the ovarian follicle collapses
so the follicular cells begin to enlarge and change to form the corpus luteum - caused by LH
the corpus luteum secretes progesterone and oestrogen.
Post-ovulatory phase
Days and outline
Days 15-28 between ovulation and next period. In ovary the corpus luteum secretes progesterone and oestrogen, if the ovum is not fertilized the corpus luteum becomes a corpus albicans.
in the uterus progesterone and oestrogen promote thickening of endometrium which becomes highly vascular and glandular if there is an embryo otherwise next menstrual phase will begin.
Functions and effects of progesterone
stimulates development of secretory tissue in the thickened endometrium
vascularisation of the myometrium and endometrium
development of glandular tissue in breasts
2 menstrual disorder and what they are
Dysmenorrhea = pain/discomfort associated with menstruation that is not pathologically explicable. It may show high levels of prostaglandins so treatment is medications that block prostaglandins.
Amenorrhea = absence of menstruation usually by pregnancy or menopause or very low body fat. Results in menstrual cycle ceasing and loss of bone mass and oestrogen levels decrease.
The combined oral contraceptive pill
Combined oestrogen and progesterone that work a negative feedback mechanism on the anterior pituitary gland blocking FSH and LH, inhibiting ovulation and development of the follicle.
Benefits are that it combats irregular, painful or heavy periods.
The main complication is thromboembolism and other cardiovascular risks, especially in smokers.
The 2 hormone controlled contraceptives
Mirena = hormonal IUD that releases a hormone similar to progesterone in low doses, preventing growth of endometrium and thickening the cervical mucus.
Jadelle = inserted under the skin in the upper arm, slow-release progesterone that prevents ovulation and thickens cervical mucus.
Menarche is …
the first occurrence of menstruation in a female
Consequences of low oestrogen
reproductive and breast tissue atrophy
dry vagina
weight gain
loss of bone mass
rising blood cholesterol but decreased HDL
hot flushes and sweating
some women experience irritability and depression or mood changes
Structure and functions of the uterus
The uterus is a muscular organ located in the female pelvis, responsible for housing and nurturing the developing fetus during pregnancy. It has 3 layers - endometrium, myometrium and perimetrium.
Its functions are a route for sperm, receives, retains and nourishes the fertilised ovum and the myometrium muscles expel the fetus during labour.
Location and functions of the cervix
It is the narrow neck of the uterus
It produces cervical mucus, allows passage during labour, and protects the uterus from bacteria etc.
Cervical cancer
A type of cancer that occurs in the cervix, often caused by persistent infection with human papillomavirus (HPV). It can lead to abnormal cell growth and, if untreated, may progress to invasive cancer.
Gardasil vaccine and cervical smears help prevent it.
Vulva …
mons pubis - fat pad that cushions pubis symphasis
labia majora - outer folds
clitoris - erectile tissue that has a role in sexual excitement
labia minora - inner folds
vestibule - area between labia minora
Breast cancer
Happens in epithelial cells of ducts.
Risk factors include early menses and late menopause, no pregnancies or breastfeeding and family history.
Diagnosis - change in skin texture, skin puckering, leakage from nipples, mammogram detects it.
Oxytocin
On a positive feedback loop so the more the baby feeds the more it stimulates the release of oxytocin, which promotes milk ejection and strengthens uterine contractions during labor.
Pathway of sperm to the oocyte
Vagina → cervix → uterus → fallopian tube ampulla where fertilization occurs.
Metabolism
Refers to all the chemical reactions in the body.
Anabolism
The process of building up larger molecules from smaller ones.
Catabolism
The process of breaking down larger molecules into smaller ones.
Glycogenesis
The process of glucose storage where excess glucose molecules are joined together to form glycogen.
Glycogen
Stored mostly in skeletal muscle fibres and some in liver cells.
Glycogenolysis
The process where glycogen stored in the liver is broken up to release glucose into the bloodstream.
Gluconeogenesis
The process where the liver makes glucose from lipids (from glycerol in triglycerides) and proteins (amino acids) when glycogen stores are used up.
Lipid catabolism
The breakdown of fats, which are the most concentrated store of energy, yielding approximately twice the energy as glucose or protein breakdown.
Lipolysis
The breakdown (catabolism) of triglycerides into glycerol and fatty acids.
Glycerol
Converted into pyruvate (pyruvic acid) and enters the Krebs cycle to produce ATP or can be converted to glucose by gluconeogenesis.
Fatty acids
Converted into acetyl coenzyme A (CoA) in the liver, which then enters the Krebs cycle to form ATP.
Ketone bodies
Produced when the levels of CoA (from gluconeogenesis of proteins) are too high for the Krebs cycle to process.
Lipogenesis
The process where more calories are consumed than are needed, resulting in glucose and amino acids being made into lipids by liver cells and adipose tissue.
Protein metabolism
Amino acids cannot be stored, so a regular intake is required to synthesize new proteins to build or repair body tissues.
Triglycerides
The main lipids used to supply energy.
ATP
Adenosine triphosphate, the energy currency of the cell.
Krebs cycle
A series of chemical reactions used by all aerobic organisms to generate energy.
Excess amino acids
Used for energy production or converted into other compounds.
Clinical significance of ketone bodies
Indicates the state of metabolism, particularly in conditions like diabetes.
Urea
A waste product formed from the breakdown of proteins.
Factors influencing metabolic rate
Includes age, sex, muscle mass, and physical activity levels.
Excess amino acids
Broken down by the liver and used for production of ATP, converted into glucose (gluconeogenesis) and triglycerides (lipogenesis).
Ketone bodies
Produced in small quantities and can be used as fuel; overproduction occurs in severe starvation and uncontrolled diabetes.
Toxicity of ketones
High levels of ketones are toxic, especially to the brain. They are acidic and cause ketoacidosis.
Excretion of excess ketones
Occurs through the lungs, giving the breath a characteristic sweet smell of acetone, and through the urine (ketonuria).
Clinical significance of ketone bodies
Excess production can lower blood pH and cause metabolic acidosis (ketoacidosis).
Amino acid catabolism
The process of breaking down unwanted amino acids
Conversion of ammonia
The liver converts ammonia (highly toxic) to urea, which is excreted in the urine.
Clinical significance of urea
Elevated levels of urea and creatinine in urine indicate decreased renal function.
Metabolic Rate
The rate at which energy is produced during cellular respiration.
Basal metabolic rate (BMR)
The metabolic rate measured under resting/fasting conditions.
Thyroxine
A hormone that increases BMR by stimulating cell respiration, leading to more oxygen use and ATP production.
Factors affecting metabolic rate
Age, gender, body size, pregnancy, eating a meal, physical activity, fever, starvation, and emotional stress can all affect metabolic rate.
Exercise and metabolic rate
Exercise can increase metabolic rate by as much as 15 times.
Hormones affecting BMR
Thyroxine, insulin, growth hormone, testosterone, and the sympathetic nervous system's release of epinephrine and norepinephrine increase BMR.
Body temperature and BMR
Higher body temperature raises BMR.
Food ingestion and BMR
Ingestion of food raises BMR by 10-20%.
Children's BMR
Children's BMR is double that of an elderly person.