Companion animal mgmt: Musculoskeletal diseases and young musculoskeletal diseases
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
what percent of the Musculoskeletal diseases involve the appendicular skeleton
70%
With normal functioning joints what do they do
They are shock absorbers
Motion/ flexibility
Articular cartilage protects end of the bone
What are 4 functions of the synovial fluid functions
Lubricates articular surface
prevents bone to bone contact
Supplies nutrients to chondrocytes
Removes any waste products
Types of cartilage two main groups
Superficial/ articular
Deep
What is included in the Superficual/ articular cartilage
Chondrocytes
Collagen
Small number of proteoglycans
What is included in the deep cartilage
Less collagen compared to superficial
More proteoglycans
what are the 3 Components of cartilage?
Chondrocytes
Proteoglycans
collagen
Age related changes
GAG content/size decreases (GAG is important for joint fluid)
Synovial fluid decreases
Collagen content decreases
When Chondrocytes become damaged what happens
GAG/collagen breakdown
Increase in matrix metalloproteinases (MMPs)
Increased production of prostaglandins, leukotrienes,
and thromboxanes
Results in further inflammation
Osteoarthristis OA what age group is affected… general?
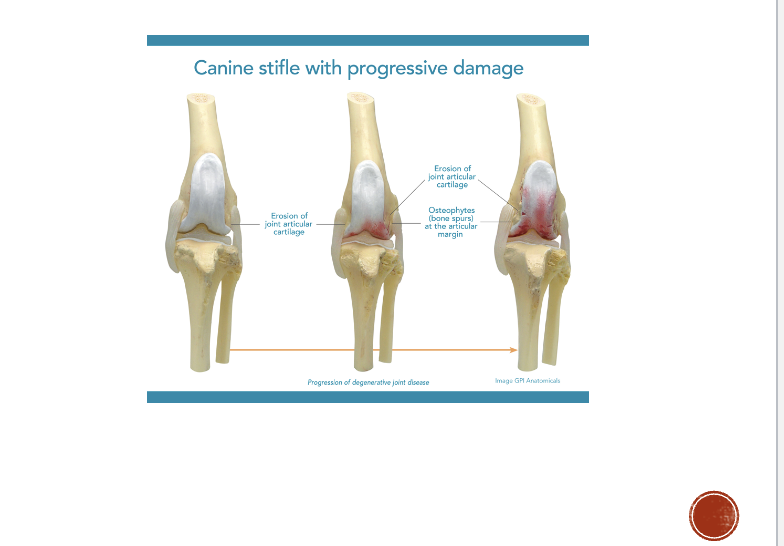
Osteoarthritic is classified as ?
Characterized by these factors
Middle aged to seniors are affected
Chronic and progressive
Destructions of articular bone cartilage
thickening of subchondral bone
Formation of osteophytes


Clinical signs of OA
Lameness
Joint heat/ swelling
pain
stiffness
decreased range of motion
Muscle atrophy
OA treatment (think of it like treating a rusty car)
Reduce pain inflammation
Prevent/ slow further degeneration
Support and restore function

What is important regarding fatty acid supplements in OA
Omega 3 preferred over omega-6
Form less inflammatory products

Glycosaminoglycans importance
GAGs form cross linkages
Have anti-inflammatory effects
Provide chondrocytes with chondroitin sulfate and HA precursers
Several forms are available
Glucosamine
Amino acid sugars produced from glucose/ glutamine
Primary component of GAGs/ proteoglycans
Protect/regenerate CT/ cartilage
Stimulates production of collagen/ proteoglycans
NSAIDS what are the benefits
Decreases production of pro-inflammatory products
Inhibition of COX reduces
Leukotriens
Prostaglandins
Thromboxanes

What is a good diet for dogs and cats that are having some joint issues
A diet high in omega-3 faty acids
Added glucosamine/ chondroitin
What is important for a dog that is suffering with OA
Weight loss may eliminate need for expensive surgical procedures
NSAIDs and joint supplements necessary during weight loss phase

Perspective on exercise with OA
Now pro low impact exercise
Start with short periods of time
Start stiff then warms up
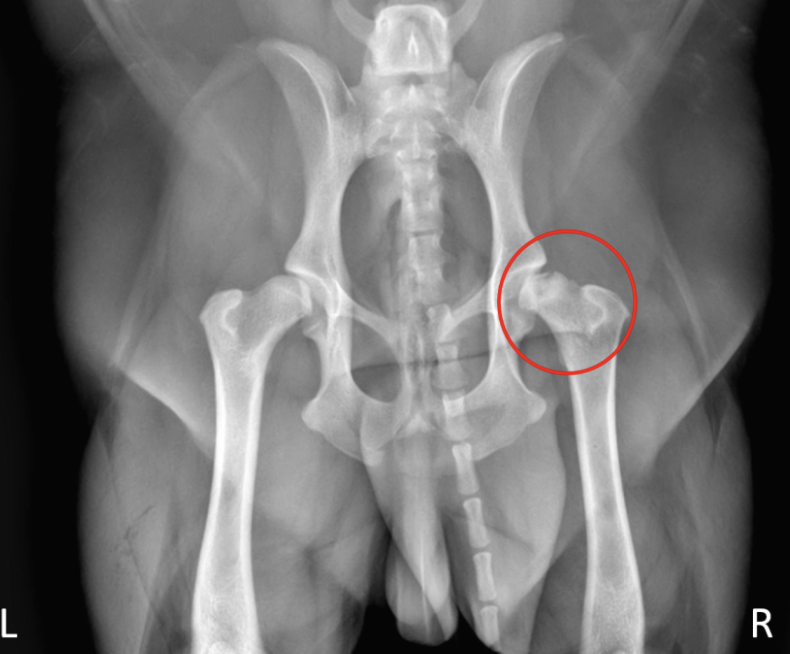
Hip dysplasia what happens
Malformation and degeneration of the coxofemoral joint

What are some of the clinical signs of HD
Can be asymptomatic at the start
May eventually observe an abnormal gait
As OA developes there is a decrease in activity, trouble rising, lameness
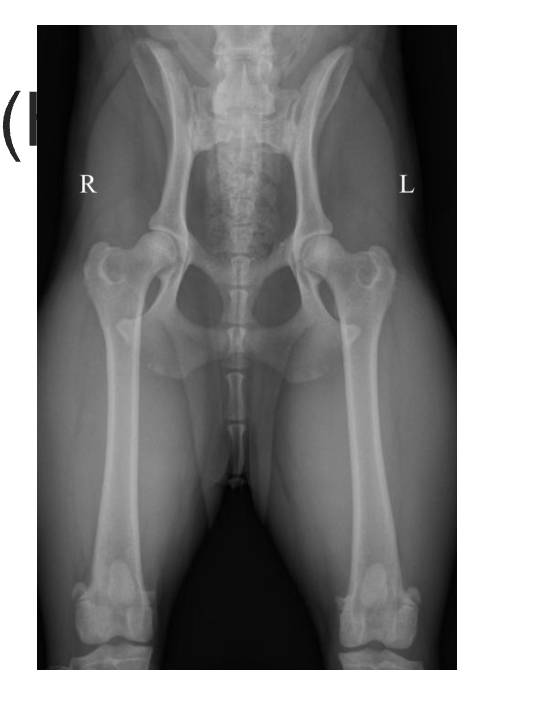
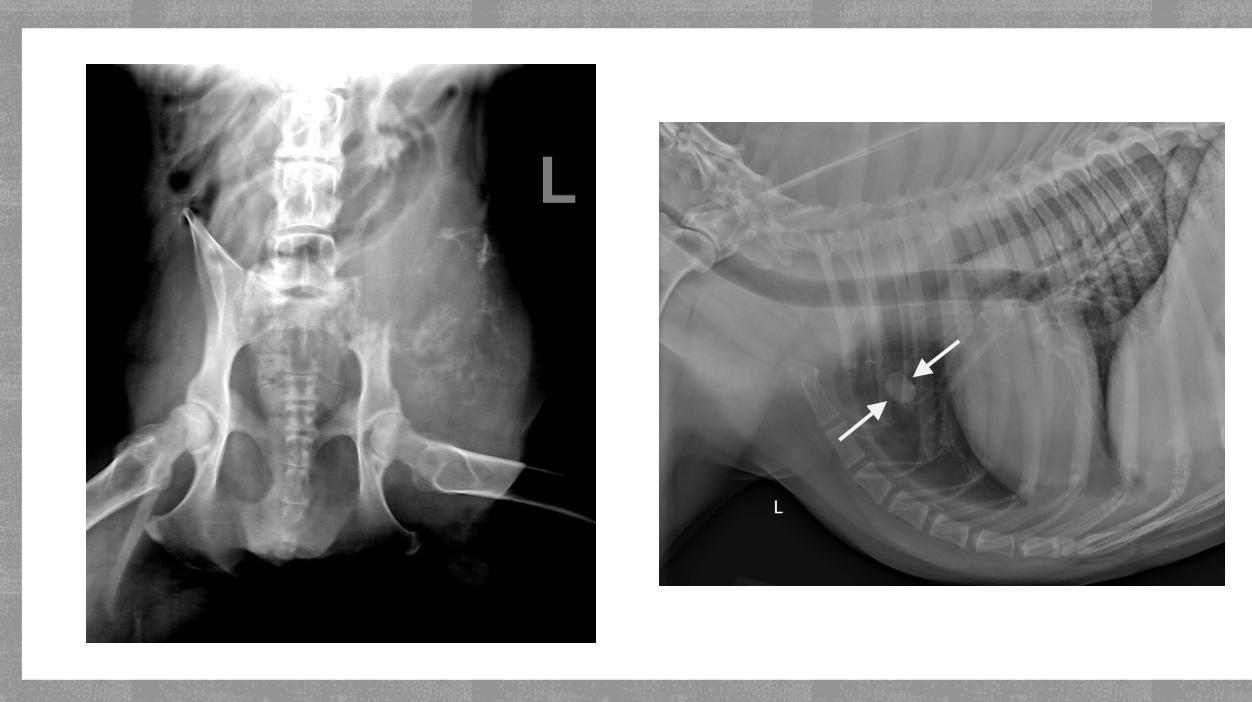
How to diagnoses HD
Pain elicted during palpatation/ extension of hips
Loss of muscle mass
Ortolani sign (clunk)
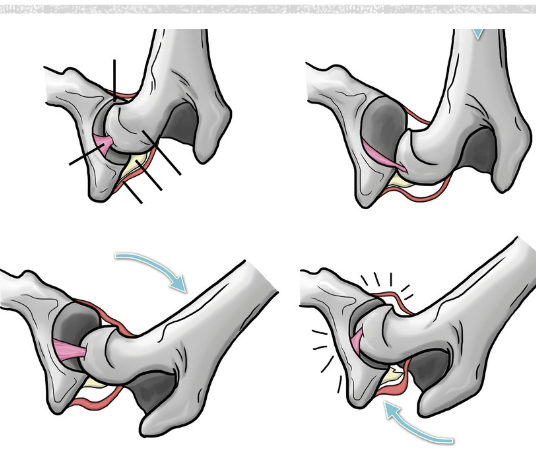
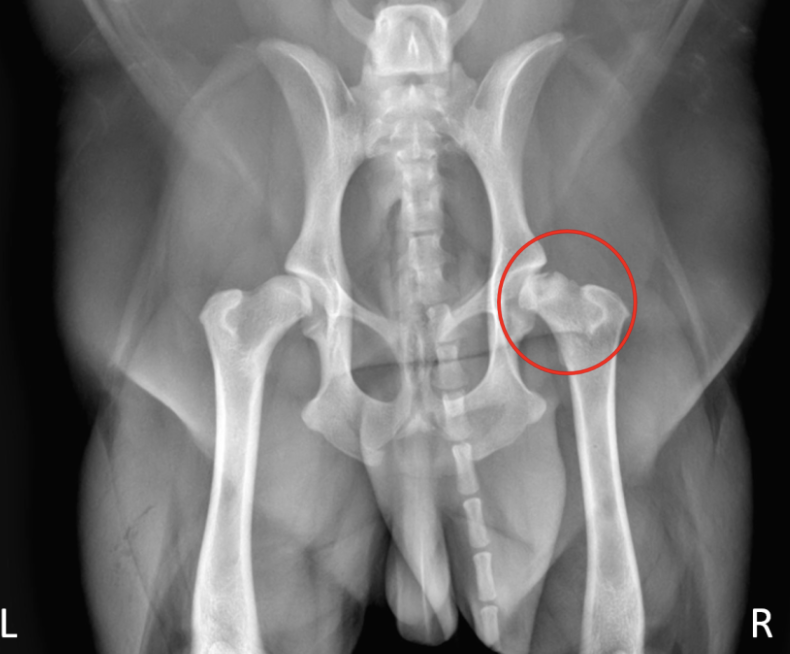
HD what does it look like of radiographs
Flattened femoral head
Thickened femoral neck
Shallow/ sclerotic acetabulum
Numerous osteophytes
Orthopedic foundation for animals
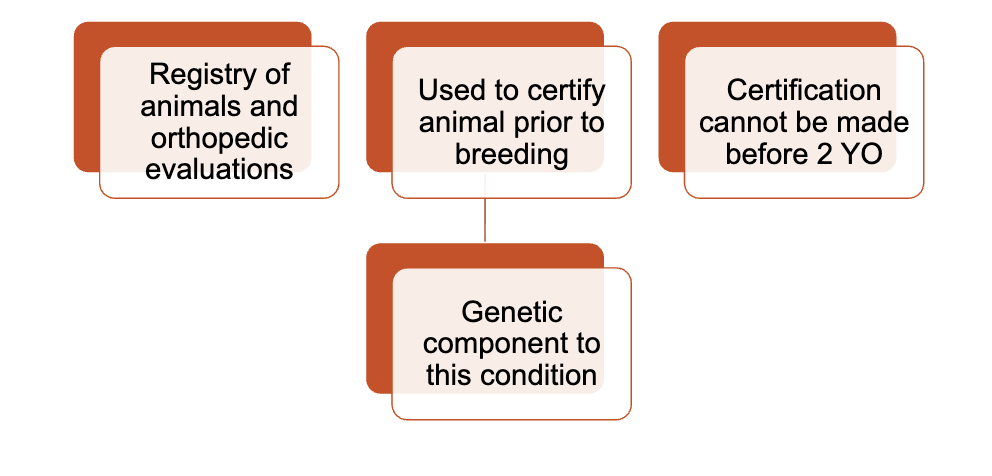
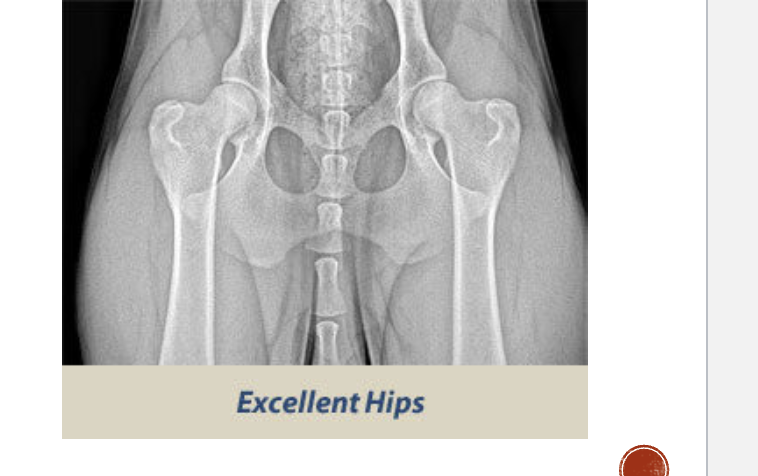
OFA normal classification
Excellent- deep seated ball that fits tightly into a well formed socket
Good- well formed congruent hip joint visualized. The ball fits well into the socket and has a good coverage present
Fair- hip joint is wider. the ball slips slightly out of socket. Socket can appear shallow

OFA mild dysplasia
Significant subluxation present
Ball partially is out of socket
increased joint space
Socket is shallow and only partailly covers the ball
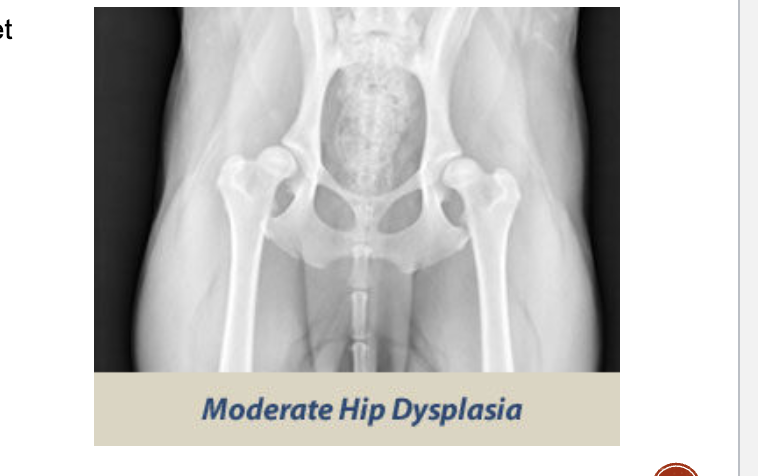
OFA moderate dysplasia
Ball is barely seated in the shaloow socket
Secondaary arthritic bone changes
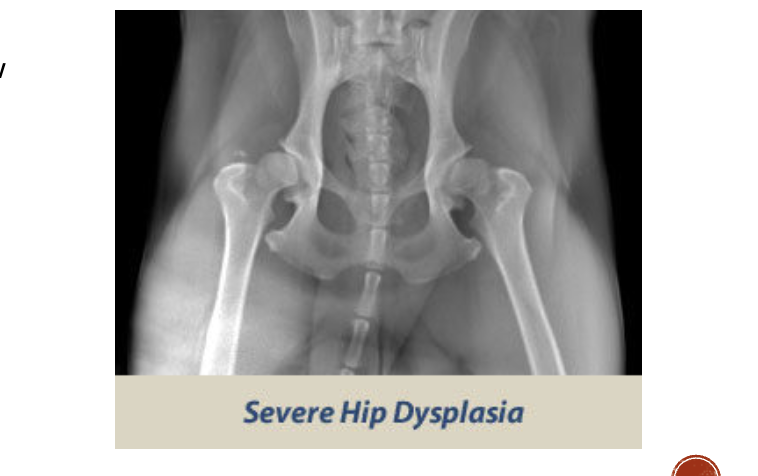
OFA severe dysplasia
Marked evidence
Ball partly/ completly out of shallow socket
significant arthritc bone changes
What are some signs of arthritic changes
Acetabulum is almost not visible
Bone spurs above hip joints
Thickening and remodeling of the femoral head

How to tread HD
Femoral head osteotomy FHO
Total hip replacement
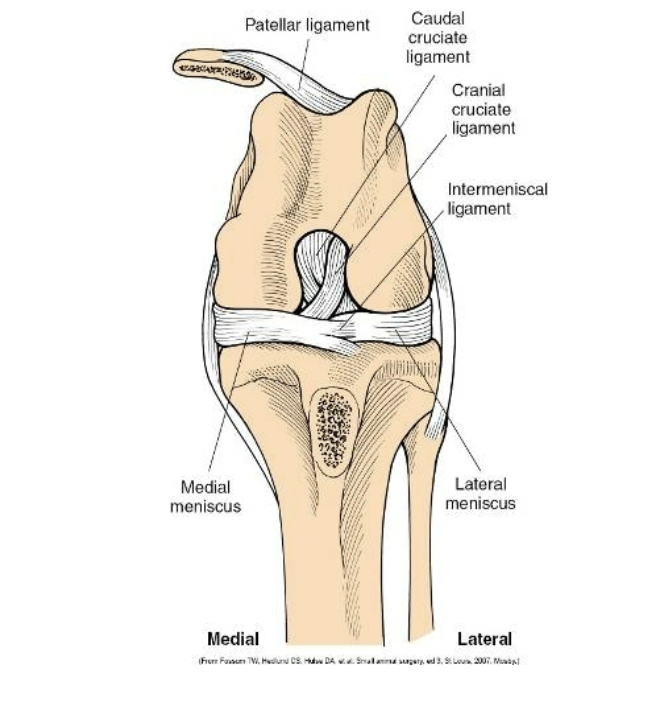
Cranial cruciate ligament rupture
One of the most common orthopedic problems
Usually caused by something
can be a partial or complete rupture
Very common to tear in the opposite leg
CCL rupture what are the clinic signs
Decreased activity level difficulty rising
trouble jumping
Decreased range of motion
swelling
lameness
muscle atrophy
How to diagnose CCL ruptures
Palpation
Cranial drawer sign
Radiographs
How to treat CCL medically
strict cage rest for 6-8 weeks
NSAIDs
joint supp.
Not considered the gold standard
results in secondary arthritis
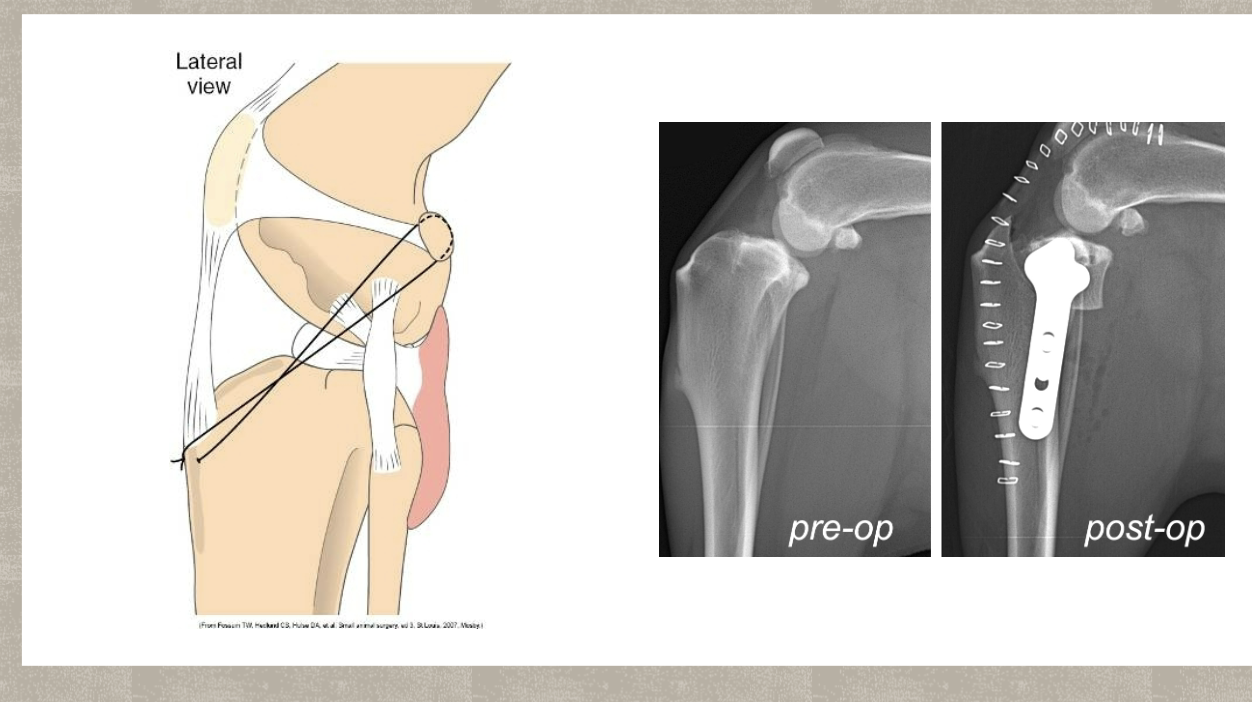
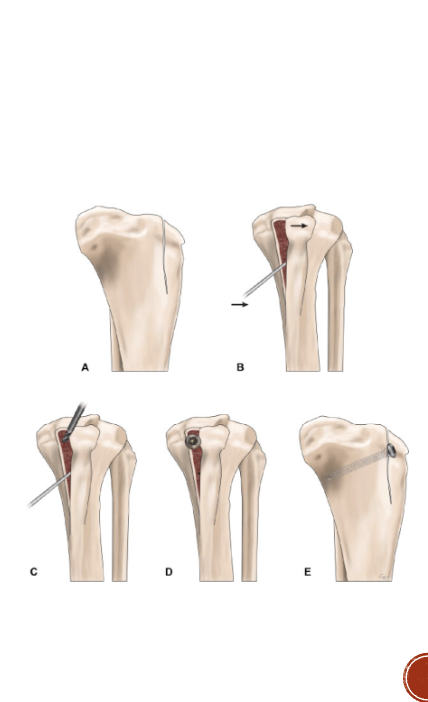
CCL treatment Surgical repair
Is considered the gold standard
Intracapsular
extracapsular
TPLO
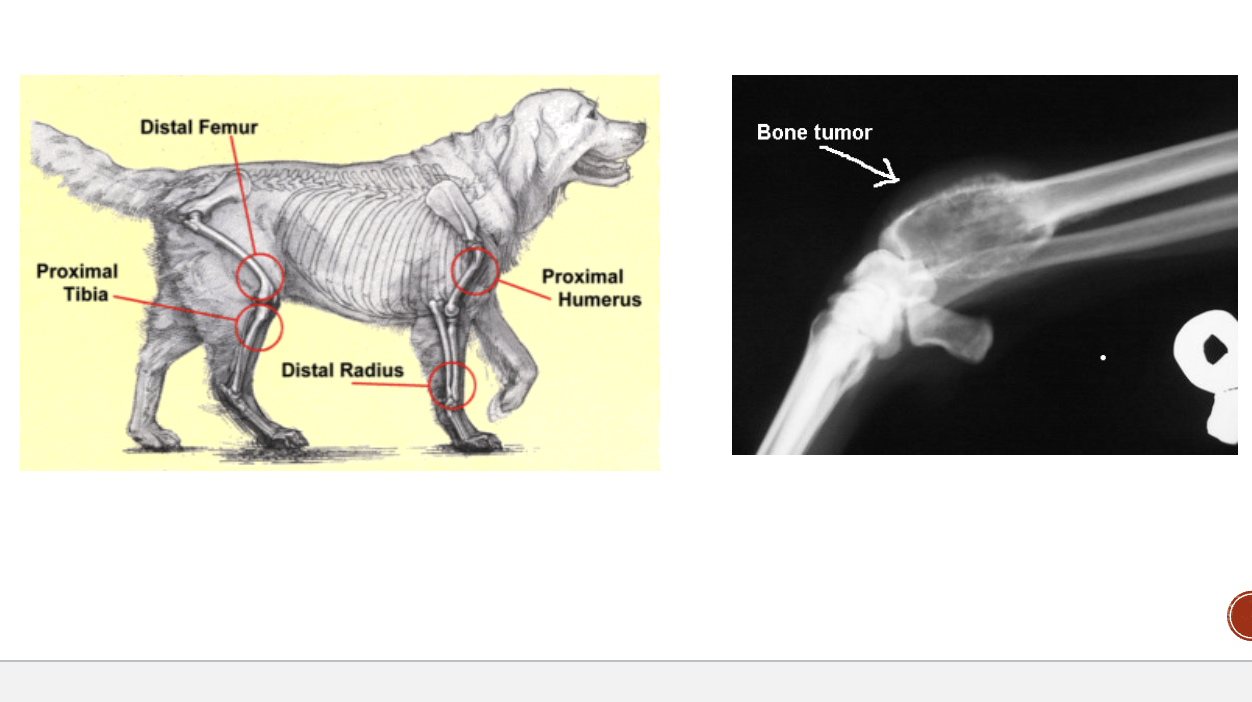
Osteosarcoma
Most common type of primary bone tumor
Can result in secondary mastasis
Common in large/ giant breeds
75% occur in appendicular skeleton
OSA diagnosis
Radiographs of bone
Radiographs of the chest
Bone biopsy
OSA treatment
Pain control
Radiation
Surgery
OSA prognosis
Median survival w/ palliative care ± amputation or radiation is about 4 months
Median survival with surgery and chemotherapy is about 10 months
Prognosis is better in cats
Median luxating patella
Most common in toy breed dogs
Skip and step, running on three legs, holding up hind leg clinical sign
Miraculously walking on all fours as if nothing has happened
50%have in both hind limps
Grading MLP what is grade 1
Kneecap can be moved out of place manually but will immediately fall back
into its natural position; doesn’t require surgery
Grading MLP what is grade 2
Kneecap occasionally slips out of groove, spontaneously creating an
intermittent lameness. Kneecap will go back in place on its own. May or may not need
surgery
Grading MLP what is grade 3
The patella is out of place all of the time but can be manipulated back into its
normal position manually (but doesn’t stay there). Requires surgery
Grading MLP what is grade 4
The patella is out of place all of the time and no amount of manipulation can
return it to its proper place. Requires surgery
MLP surgical procedure
Lateral imbrication
Trochlear modification
Tibial crest (tuberosity) transportation
young musculoskeletal diseases: Hypertrophic osteodystrophy HOD
Developmental suto inflammatory disease
Unknown cause
Fast growing puppies of large giant breeds
Blood flow decreases to part of bone adjacent to joint
Interruption of bone formation
Bones dont harden correctly
Affects more than one leg at a time
Can permanently damage growth plates
Can be really painful
Self-limiting
Chance of reoccurrence
HOD clinical signs
Slight limp
Swollen, warm, painful leg bones
May be non-weight bearing
Reluctance to get up/walk
Anorexia
Weight loss
Fever
Depression
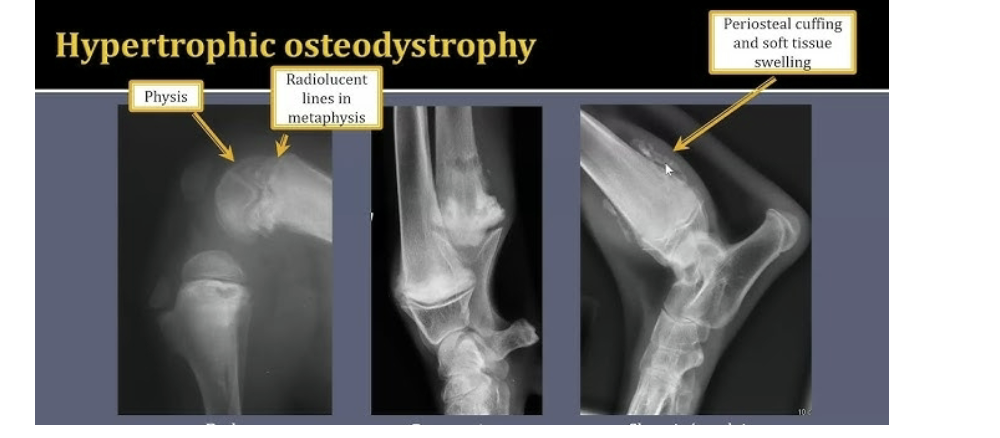
How to diagnose HOD
PE and radiographs
HOD treatment
NSAIDS
IVF
Nutritional support
Antibiotics
Restricted exercise

Panosteitis
Cause is unknown
Involve long leg bones of large breeds
Episodes reoccur
Lameness shifts from one leg to another
Normally outgrow
NSAIDs
Legg calve perthes disease
Aseptic/ avascular necrosis of femoral head
Lameness of the hip joint
Most common in young, small breed dogs
Genetic component
Pathogenesis of Legg calve perthes disease
Interruption of blood supply to head of femur
Portions of bone begin to die
Overlying cartilage that lines hip joint collapses
Results in a painful, poorly fitting hip joint
Clincal signs of Legg calve perthes disease
Crying out when stretching limb/trying to bear weight
Favoring/lameness of affected leg
Muscle atrophy
Diagnosis/ treatment of Legg calve perthes disease
Radiographs required
Surgical intervention recommended
Femoral head and neck ostectomy
NSAIDs